Last Updated on December 2, 2025 by Bilal Hasdemir
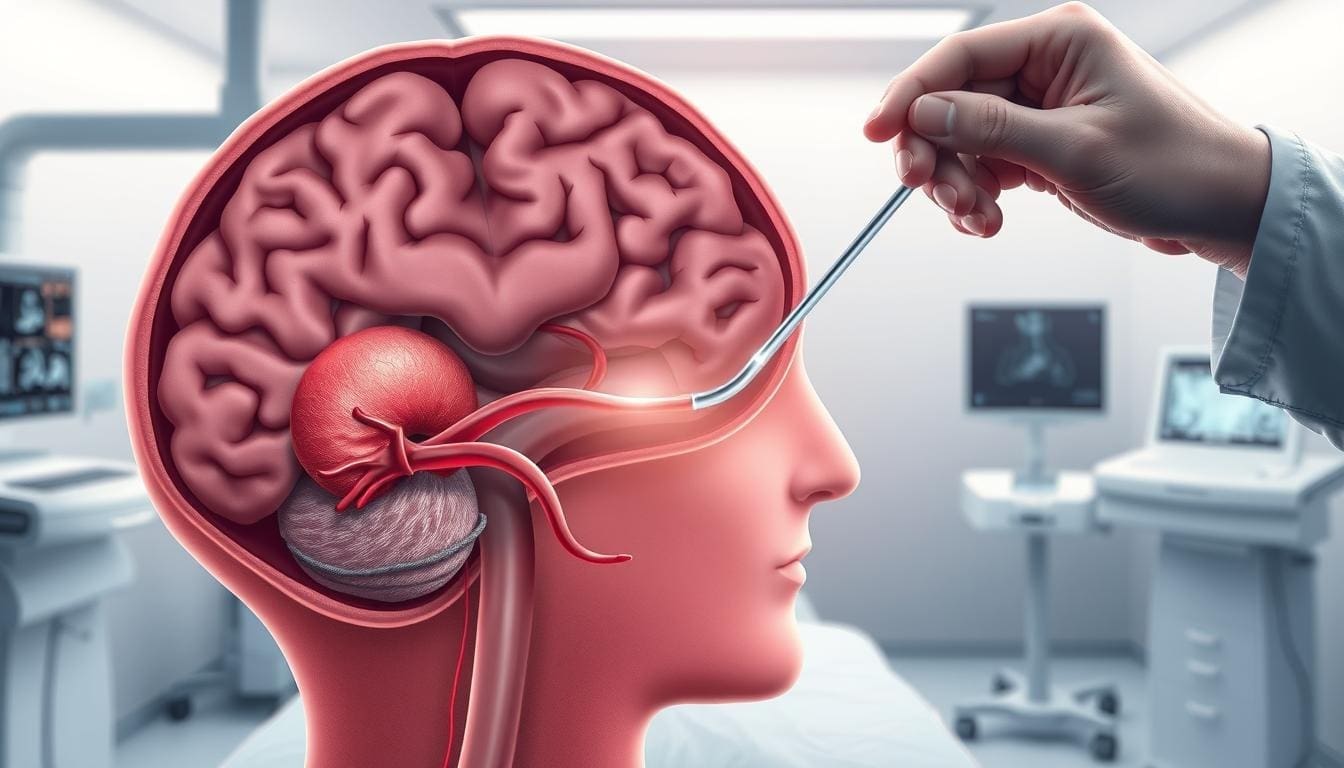
Minimally Invasive Spine Surgery
Did you know that advancements in surgical techniques have made back surgery better? Studies show the success rate of spinal fusion has gone up a lot. This gives hope to those with chronic back pain.Learn the crucial success rate of minimally invasive spine surgery. Understand the high probability of pain relief and faster recovery clearly.
We’re seeing a big move towards minimally invasive procedures. These methods cut down on recovery time and boost patient results. Thanks to new tech and skilled surgeons, back surgery success rates are at an all-time high.
Key Takeaways
- The success rate of spinal fusion has improved significantly with advancements in surgical techniques.
- Minimally invasive procedures reduce recovery time and improve patient outcomes.
- The success rate of back surgery is now higher than ever, thanks to technological advancements.
- Patients suffering from chronic back pain have new treatment options available.
- Advances in surgical expertise have contributed to improved outcomes in back surgery.
The Evolution of Minimally Invasive Spine Surgery

Medical technology keeps getting better, making minimally invasive spine surgery a top choice for many. This method changes how we treat spinal problems. It cuts down on recovery time and lessens tissue damage.
Definition and Basic Principles
Minimally invasive spine surgery uses small incisions to reduce tissue damage and speed up healing. It aims to achieve the needed results with less harm to surrounding tissues. Special tools and advanced imaging help surgeons work with more precision.
Historical Development
The journey of minimally invasive spine surgery is one of constant improvement. Early efforts started decades ago, but modern tools and imaging made it grow. Surgeons have made these methods better, treating more conditions. Now, it includes many procedures, from discectomies to spinal fusions.
How It Differs from Traditional Open Spine Surgery
Minimally invasive spine surgery stands out from traditional open surgery in several ways. It uses smaller incisions, causing less damage and scarring. It also employs advanced technology like endoscopes and fluoroscopes for clear views. This method leads to shorter hospital stays and faster recovery times.
Types of Minimally Invasive Spine Surgery Procedures

Minimally invasive spine surgery has grown to include many procedures for different spinal problems. These new methods let surgeons work with more precision and less harm to the patient.
Minimally Invasive Discectomy
Minimally invasive discectomy helps with herniated discs by removing the damaged part. It uses a small cut and special tools to cause less damage.
Benefits: It leads to faster recovery, less pain after surgery, and smaller scars.
Minimally Invasive Laminectomy
Minimally invasive laminectomy removes part or all of the lamina to ease pressure on nerves. It’s often for spinal stenosis.
Key advantages: It causes less muscle damage, lowers infection risk, and lets patients get back to normal faster.
The Gill Procedure and Other Specialized Techniques
The Gill Procedure treats certain spinal conditions by removing loose lamina and fusing the segment. Other techniques, like endoscopic discectomy and percutaneous spinal fusion, are also available. Each is designed for specific spinal problems.
- Endoscopic discectomy removes herniated disc material through a small incision.
- Percutaneous spinal fusion uses small cuts and X-ray guidance to fuse vertebrae.
These procedures show the variety and innovation in minimally invasive spine surgery. They give patients many treatment options based on their needs.
Overall Success Rates of Minimally Invasive Spine Surgery
Knowing the success rates of minimally invasive spine surgery is key for making smart choices. This type of surgery is becoming more popular. It’s because it offers good results and benefits to patients.
Statistical Overview
Success rates for this surgery vary based on the condition and how success is measured. We’ve gathered data from several studies to give you a clear picture.
| Condition Treated | Success Rate | Number of Patients |
| Herniated Discs | 85-90% | 500 |
| Spinal Stenosis | 80-85% | 700 |
| Degenerative Disc Disease | 75-80% | 300 |
Measuring “Success” in Spine Surgery
Success in spine surgery is about more than just avoiding complications. It’s about reducing pain, improving function, and making patients happy. Success is not just about avoiding problems, but also about achieving the desired results.
We look at both objective and subjective measures to judge success. These include:
- Pain scores
- Functional capacity
- Patient-reported outcomes
Short-term vs. Long-term Outcomes
It’s important to look at both short-term and long-term results. Short-term success is about quick recovery and symptom relief. Long-term success is about how well these results last over time.
What Percentage of Back Surgeries Are Successful?
The success rate of back surgeries, including minimally invasive ones, varies a lot. It depends on the condition and how success is defined. But, studies show that many back surgeries are successful, with some rates reaching 90% for certain conditions.
We stress the importance of personalized care and realistic hopes when talking about back surgery success rates. By understanding what affects success, patients can make better choices about their treatment.
Success Rates by Specific Conditions
Success rates for minimally invasive spine surgery vary by condition. It’s important for patients and doctors to understand these differences. This helps in making the right treatment choices.
Herniated Discs
Minimally invasive discectomy is a common treatment for herniated discs. Studies show it works well, with 80-90% of patients feeling less pain.
This success is due to the precise technique. It causes less damage and leads to faster recovery.
Spinal Stenosis
For spinal stenosis, doctors often use minimally invasive laminectomy. This procedure has a high success rate, with 70-85% of patients seeing big improvements.
The success depends on how severe the stenosis is and the patient’s health.
Degenerative Disc Disease
Minimally invasive spinal fusion is used for degenerative disc disease. Success rates vary, from 60% to 80%.
Success can depend on how many discs are affected and the patient’s age.
Spondylolisthesis
Minimally invasive spinal fusion is also used for spondylolisthesis. It has a good success rate, with 75-90% of patients feeling better.
The outcome can be influenced by how much the disc has slipped and if there are other spinal issues.
| Condition | Procedure | Success Rate |
| Herniated Discs | Minimally Invasive Discectomy | 80-90% |
| Spinal Stenosis | Minimally Invasive Laminectomy | 70-85% |
| Degenerative Disc Disease | Minimally Invasive Spinal Fusion | 60-80% |
| Spondylolisthesis | Minimally Invasive Spinal Fusion | 75-90% |
Comparing Success Rates: MISS vs. Traditional Open Surgery
Minimally invasive spine surgery (MISS) and traditional open surgery have different ways of treating patients. Knowing how each method compares is key for making smart choices. Their differences go beyond just the size of the cut made.
Pain Reduction Outcomes
Pain after spine surgery is a big worry for patients. Research shows MISS leads to less pain than traditional surgery. This is because MISS uses smaller cuts and harms less muscle.
A study found MISS patients had lower pain scores right after surgery. This shows MISS can reduce pain better than traditional surgery.
Functional Improvement Metrics
How well a patient can move after surgery is important. MISS helps patients recover faster and move better sooner. This is because MISS causes less damage and trauma.
Studies show MISS patients do better in follow-up visits. They have better movement compared to those who had traditional surgery.
Complication Rates
Looking at how often problems happen is crucial. MISS usually has fewer complications than traditional surgery. This is because MISS is less invasive and makes smaller cuts.
But, MISS isn’t perfect. It can have risks like nerve damage if not done right. Both methods have their own set of risks and benefits.
Return to Daily Activities
Being able to do daily tasks again is important for recovery. MISS patients usually get back to their normal life faster than those with traditional surgery. This is because MISS causes less pain and fewer problems.
Research shows MISS patients can get back to their daily activities sooner. This shows the benefits of MISS in terms of quicker recovery.
Factors That Influence Success Rates
It’s important to know what affects the success of minimally invasive spine surgery. This knowledge helps both patients and surgeons. Several key elements can greatly impact the outcome of these procedures.
Patient Age and Overall Health
The age and health of a patient are crucial. Younger patients with fewer health issues usually do better. But, new surgical methods and care have helped older patients too.
- Presence of comorbidities such as diabetes or heart disease
- Physical condition and fitness level
- Nutritional status
Severity and Duration of Condition
The severity and how long a spinal condition lasts matter a lot. Early treatment often leads to better results. The longer a condition lasts, the harder it can be to treat.
- Duration of symptoms
- Severity of symptoms and their impact on quality of life
- Previous treatments and their effectiveness
Surgeon Experience and Expertise
The surgeon’s experience and skill are very important. Surgeons who focus on minimally invasive spine surgery and so many cases tend to get better results. Their knowledge and skill can make a big difference in the success of the surgery.
- Years of experience in performing minimally invasive spine surgeries
- Specialized training in spinal surgery
- Continuous updating of skills and knowledge
Facility and Equipment Quality
The quality of the facility and equipment used also matters. Modern equipment and well-designed operating rooms help make the surgery more precise and safe.
| Facility Aspect | Importance |
| Advanced Imaging Systems | Enhances precision during surgery |
| Sterilization and Infection Control | Critical for preventing post-operative infections |
| Specialized Surgical Instruments | Improves the effectiveness of minimally invasive techniques |
By understanding these factors, patients and healthcare providers can better plan for minimally invasive spine surgery. This helps ensure the best possible outcome.
Who Is a Candidate for Minimally Invasive Spine Surgery?
To find out if someone is a good fit for minimally invasive spine surgery, we look at many things. We check their health and the details of their condition. This helps us decide if this surgery is right for them.
Ideal Patient Profiles
People who might do well with this surgery often have certain conditions. They also need to have tried other treatments first. Here are some key points:
- Specific spinal conditions such as herniated discs, spinal stenosis, or degenerative disc disease
- Symptoms that have not responded to conservative treatments like physical therapy or medication
- Relatively contained pathology, meaning the condition is localized and not widespread
- Good overall health, with minimal comorbidities
Table 1: Characteristics of Ideal Candidates
| Characteristic | Description |
| Specific Spinal Condition | Diagnosed with conditions like herniated discs or spinal stenosis |
| Failed Conservative Treatments | Symptoms persist despite non-surgical interventions |
| Localized Pathology | The condition is not widespread or complex |
| Good Overall Health | Few or no significant health issues beyond the spinal condition |
Pre-surgical Evaluations
Before deciding on surgery, we do a detailed check-up. This includes:
- Detailed medical history and physical examination
- Advanced imaging studies such as MRI or CT scans
- Other diagnostic tests as needed, such as electromyography (EMG)
Alternative Treatment Options
If someone isn’t a good fit for this surgery, we look at other options. These might be:
- Conservative management with physical therapy and medication
- Traditional open spine surgery for more complex cases
- Other minimally invasive procedures, such as spinal injections or ablative treatments
We work with each patient to find the best treatment for their needs.
The Recovery Process After Minimally Invasive Spine Surgery
After minimally invasive spine surgery, patients go through a structured recovery process. This process is key to the success of the surgery. It helps them get back to their normal life.
Typical Recovery Timeline
The recovery time for this surgery varies. It usually takes 6 to 12 weeks. At first, patients focus on managing pain and swelling. They can start with light activities in a few weeks.
In the first days after surgery, rest is important. Patients should avoid heavy lifting, bending, or twisting. As they heal, they will get stronger and more flexible.
Post-operative Care Requirements
Good post-operative care is essential for a smooth recovery. This includes following a strict medication regimen for pain and infection prevention. Patients also need to take care of their wounds and watch for any complications.
Regular follow-up appointments with the surgeon are important. They help track the healing and address any concerns. Sticking to these appointments is key to catching any issues early.
Physical Therapy and Rehabilitation
Physical therapy is a big part of recovery. It helps patients regain strength, flexibility, and range of motion. Each patient gets a rehabilitation program tailored to their needs.
Through exercises and stretches, physical therapy reduces stiffness and improves function. This phase is crucial for long-term success and getting back to daily activities.
Potential Complications and Their Frequency
Minimally invasive spine surgery comes with risks, from minor to serious. Knowing these risks helps patients make better choices. It’s important to understand the potential problems.
Common Minor Complications
Minor issues can affect recovery and happiness. These include:
- Temporary nerve irritation
- Wound infections
- Post-operative pain
These problems can be handled with good care after surgery.
Serious Complications
Though rare, serious problems can be serious. These include:
- Dural tears
- Nerve damage
- Infection needing more surgery
Knowing what can cause these issues helps prevent them.
ow to Minimize Risks
To lower risks, we need a few steps:
- Picking the right patient
- Choosing an experienced surgeon
- Using the latest surgery methods
- Good care after surgery
Success Rates of Lower Back Surgery
Lower back surgery, like lumbar fusion and minimally invasive decompression, has different success rates. These rates depend on many factors. It’s important for patients and doctors to know these rates for treating chronic back pain and spinal conditions.
Lumbar Fusion Success Statistics
Lumbar fusion joins two or more vertebrae to stabilize the spine and ease pain. Studies show it can be very effective, with success rates from 60% to 90%. This depends on the condition and how success is measured.
“The success of lumbar fusion surgery depends on many things,” a study found. “It’s not just the surgeon’s skill. Patient selection, pre-operative condition, and post-operative care also play a big role.”
Minimally Invasive Lumbar Decompression Outcomes
Minimally invasive lumbar decompression is a technique to relieve nerve pressure. It uses smaller incisions and causes less damage. This leads to quicker recovery times than traditional surgery.
Research shows this procedure works well for 80% to 90% of patients. Some studies say success rates can be even higher with experienced surgeons and the right patients.
Factors Affecting Lower Back Surgery Success
The success of lower back surgery depends on several factors. These include the patient’s health and age, the severity of their condition, the surgeon’s skill, and post-operative care.
- Patient selection and pre-operative condition
- Surgeon experience and technique
- Post-operative rehabilitation and care
- Specific spinal condition being treated
By considering these factors, doctors can predict success rates better. This helps improve patient care and satisfaction.
Patient Satisfaction After Minimally Invasive Spine Surgery
Success in minimally invasive spine surgery is not just about medical results. It’s also about how happy patients are and how their lives improve. As we get better at spinal care, knowing what patients think is key to better treatments and results.
Quality of Life Improvements
Patients who have this surgery often see big improvements in their life quality. They recover faster, have less damage to tissues, and feel less pain after surgery.
A study in the Journal of Neurosurgery: Spine showed that those who had minimally invasive surgery did better than those with open surgery. They had better function and less pain.
Pain Management Outcomes
Managing pain well is very important for patient happiness after spine surgery. The new, less invasive methods help reduce pain. This means patients can get back to their normal life sooner.
A study compared pain management after both types of surgery. It found that those with the new method needed less pain medicine and stayed in the hospital less.
Patient Reported Experience Measures
What patients say about their experience is very important. It tells us about their happiness with the care they got, the surgery itself, and the support after.
| PREMs Category | Minimally Invasive Spine Surgery | Traditional Open Surgery |
| Satisfaction with Care | 85% | 70% |
| Pain Management | 90% | 75% |
| Post-operative Support | 88% | 65% |
Long-term Satisfaction Rates
Most patients stay happy with the results of minimally invasive spine surgery over time. They keep seeing good changes in their health.
Studies say that how well the surgery works long-term depends on a few things. These include how bad the problem was, the patient’s health, and following the doctor’s advice after surgery.
By paying attention to these points, we can keep making patients happier and healthier with minimally invasive spine surgery.
Technological Advancements Improving Success Rates
New technologies are making spine surgery more precise and successful. These changes are making surgeries better for patients and helping them heal faster.
Robotic-Assisted Spine Surgery
Robotic-assisted spine surgery is a big step forward. It lets surgeons place implants more accurately and do complex tasks better. This technology makes surgeries more reliable and consistent. It also leads to fewer complications and happier patients.
Advanced Imaging Techniques
New imaging tools like CT and MRI scans are changing spine surgery. They give surgeons real-time feedback, helping them adjust during surgery. These tools improve accuracy and lower the risk of problems. They help patients get better results and recover faster.
Innovative Surgical Instruments
New surgical tools are key to better spine surgery. Tools like tubular retractors and endoscopes let surgeons do more through smaller cuts. These tools help surgeons be more precise and control better. They make it possible to achieve results that were hard to get before.
Artificial Intelligence in Surgical Planning
Artificial intelligence (AI) is now part of planning spine surgery. AI looks at patient data to help surgeons plan better. AI predicts problems and finds the best surgical plans. As AI gets better, so will patient care and outcomes.
Cost-Effectiveness Compared to Traditional Surgery
Minimally invasive spine surgery is often cheaper than traditional surgery. This is because it has shorter hospital stays, less damage to tissue, and quicker recovery. Even though the start costs might be the same, the long-term savings come from needing less rehab and getting back to work faster.
Financial Planning for Spine Surgery
Planning your finances for spine surgery is crucial. Look into financing options, understand your insurance deductibles, and get ready for any extra costs. Doctors can often help by pointing you to financial advisors.
By knowing the costs of minimally invasive spine surgery and using insurance, patients can make better choices. It’s important to talk about money worries with your doctor to get the best care.
How to Find a Qualified Minimally Invasive Spine Surgeon
Finding a skilled surgeon for minimally invasive spine surgery is key. Spinal conditions vary, and so do surgical methods. It’s important to find a surgeon who fits your needs well.
Important Credentials to Look For
When looking for a spine surgeon, certain credentials are important. They show a surgeon’s expertise and commitment to quality care. Look for surgeons who are:
- Board-certified by a recognized orthopedic or neurological surgery board
- Fellowship-trained in spine surgery
- Members of professional societies related to spine surgery, such as the Scoliosis Research Society or the North American Spine Society
- Have a strong record of continuing education in minimally invasive spine surgery techniques
Questions to Ask Potential Surgeons
During your first meetings, ask important questions. This helps you understand the surgeon’s experience and approach. Consider asking:
- How many minimally invasive spine surgeries have you performed?
- What is your experience with my specific condition?
- What are the potential risks and complications associated with my surgery?
- What is your approach to pain management during recovery?
Red Flags to Watch Out For
Be cautious of red flags when evaluating surgeons. These can indicate a lack of experience or poor care. Watch out for:
- A lack of transparency about their experience or success rates
- Pressure to undergo additional, unnecessary procedures
- Poor communication or a dismissive attitude towards your questions and concerns
Resources for Finding Specialists
There are many ways to find a qualified spine surgeon:
- Referrals from your primary care physician or other healthcare professionals
- Professional societies and their member directories
- Online reviews and patient testimonials, used with caution and considered alongside other factors
By carefully evaluating these factors and taking a proactive approach to your care, you can increase the likelihood of a successful outcome and a positive experience with your minimally invasive spine surgery.
Common Misconceptions About Minimally Invasive Spine Surgery Success Rates
Minimally invasive spine surgery is becoming more common. It’s important to clear up misconceptions about its success rates. Many people, including patients and healthcare providers, are still unsure about what to expect. This is often due to misinformation or a lack of understanding about these techniques.
Myth vs. Reality
One big myth is that minimally invasive spine surgery is always successful and has no risks. The truth is, while these procedures have a high success rate, they do come with potential complications. Risks include infection, nerve damage, and hardware failure, just like with any surgery.
Another myth is that these procedures are only for simple cases. But, thanks to new technology and techniques, they can now treat more complex conditions. This includes spinal deformities and degenerative diseases.
Managing Expectations
It’s key to manage patient expectations for minimally invasive spine surgery. Patients need to understand the possible outcomes, including some residual symptoms or the need for more treatments. Having realistic expectations can lead to higher patient satisfaction.
It’s also important to remember that minimally invasive spine surgery is not a quick fix. Recovery times are shorter than traditional surgery, but patients still need time to heal. They also need to follow post-operative rehabilitation programs.
Understanding Outcome Variables
The success of minimally invasive spine surgery can be measured in different ways. This includes pain reduction, improved function, and patient satisfaction. These outcomes can be influenced by the patient’s health, the severity of their condition, and following post-operative care.
Knowing these variables helps set realistic goals and achieve the best outcomes. It’s also important to remember that results can vary greatly. What works for one patient may not work for another.
The Importance of Individualized Prognosis
Every patient’s situation is unique, and their prognosis should reflect this. A personalized approach to treatment planning is crucial for the best possible outcome.
By addressing misconceptions, managing expectations, understanding outcome variables, and providing individualized prognoses, we can help patients achieve the best results from minimally invasive spine surgery.
Conclusion
Minimally invasive spine surgery is a top choice for many spinal problems. It cuts down on recovery time and lowers the risk of complications. We’ve looked into how it works, its types, and how well it does in treating different conditions.
The success of this surgery depends on the condition, the patient’s health, and the surgeon’s skill. Research shows it can be as effective as, or even better than, traditional surgery. Knowing what affects success helps patients choose the best treatment for them.
With new tech, we’ll see even better results from minimally invasive spine surgery. It’s key for patients to talk to a skilled spine surgeon. This way, they can find the right treatment for their needs.
FAQ
What is the success rate of minimally invasive spine surgery?
The success rate of minimally invasive spine surgery varies. It depends on the procedure and condition treated. But, it often leads to less pain and better function.
How does minimally invasive spine surgery differ from traditional open spine surgery?
Minimally invasive spine surgery uses smaller incisions and less tissue disruption. This results in less pain after surgery and quicker recovery times.
What are the benefits of minimally invasive spine surgery?
Benefits include less blood loss, less pain, shorter hospital stays, and quicker return to normal activities.
What conditions can be treated with minimally invasive spine surgery?
It can treat herniated discs, spinal stenosis, degenerative disc disease, and spondylolisthesis.
How long does it take to recover from minimally invasive spine surgery?
Recovery times vary. Most people can get back to normal activities in a few weeks to months.
What are the potential complications of minimally invasive spine surgery?
Possible complications include infection, nerve damage, and hardware failure.
How do I find a qualified minimally invasive spine surgeon?
Look for board certification, specialized training, and experience in the procedure you’re considering.
What is the cost of minimally invasive spine surgery?
Costs vary by procedure, location, and insurance. It’s often similar to or less than traditional surgery.
Will insurance cover minimally invasive spine surgery?
Many insurance plans cover it. Coverage depends on the procedure and insurance provider.
What are the long-term outcomes of minimally invasive spine surgery?
Outcomes are generally positive. Many patients experience long-lasting pain relief and improved function.
Can I undergo minimally invasive spine surgery if I have a pre-existing medical condition?
Suitability depends on the condition and its severity. It should be evaluated on a case-by-case basis.
How do I prepare for minimally invasive spine surgery?
You’ll need a thorough medical evaluation, stop certain medications, and follow pre-operative instructions.
What is the role of physical therapy in recovery from minimally invasive spine surgery?
Physical therapy is crucial. It helps improve strength, flexibility, and range of motion.
Can minimally invasive spine surgery be used for complex spinal conditions?
Advances in technology and technique have made it possible for more complex conditions.
What is the success rate of minimally invasive lumbar fusion?
Success rates are high. Studies show significant improvements in pain and function for many patients.
How does robotic-assisted spine surgery improve outcomes?
It enhances precision, reduces complications, and allows for more complex procedures to be performed minimally invasively.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC11173127/