Thinking about bariatric surgery can be scary, with worries about risks. But, contemporary data shows that today’s bariatric surgeries have very low mortality rates.Data on the mortality rate for bariatric surgery (All procedures).
Bariatric surgery is now a safe choice for severe obesity. The mortality rates are about 0.1 to 0.15 percent. This shows how much medical tech and surgery skills have improved.
At top centers, serious problems happen less than 5% of the time. This proves how safe and effective these surgeries are. Knowing these facts helps ease worries and gives a clear view of what to expect.
Key Takeaways
- Bariatric surgery has a low mortality rate of 0.1 to 0.15 percent.
- Major complication rates at accredited centers are under 5%.
- Modern bariatric procedures have significantly improved safety.
- Bariatric surgery is a reliable treatment for severe obesity.
- Advancements in medical technology have contributed to the reduced mortality rates.
The Evolution of Bariatric Surgery
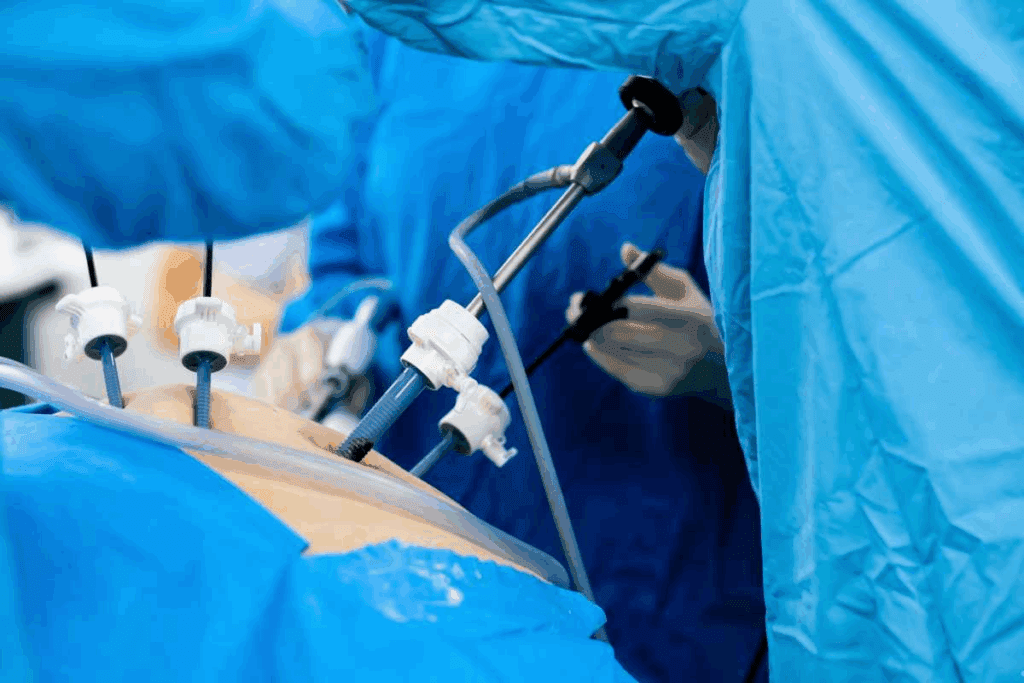
Bariatric surgery has changed a lot over the years. It now offers safer and more effective ways to treat obesity. What was once a simple procedure is now a key treatment for severe obesity and related health issues.
There are several types of bariatric surgery, each with its own benefits and risks. The main ones are Roux-en-Y gastric bypass, sleeve gastrectomy, adjustable gastric banding, and biliopancreatic diversion with duodenal switch. Studies show that sleeve gastrectomy and Roux-en-Y gastric bypass are among the most effective, leading to significant weight loss over 5 years.
Common Types of Weight Loss Procedures
Over time, several bariatric surgeries have been developed. Roux-en-Y gastric bypass is well-known for its effectiveness in weight loss and improving health. Sleeve gastrectomy involves removing a big part of the stomach, leaving a narrow “sleeve” to limit food intake.
Adjustable gastric banding is a less invasive method. It uses an adjustable band around the stomach to create a small pouch. Biliopancreatic diversion with duodenal switch is more complex. It removes a large part of the stomach and reroutes the intestines to reduce calorie absorption.
The Growing Popularity of Bariatric Interventions
Bariatric surgery is becoming more popular because it effectively treats severe obesity and related health problems. More people are seeing it as a viable treatment option. This is because our understanding of obesity and its effects on health has improved.
Advances in surgical techniques and better care before and after surgery have made bariatric procedures safer and more effective. This has led more patients to consider bariatric surgery for significant weight loss and better health.
Current Mortality Rate for Bariatric Surgery
Bariatric surgery has seen a big drop in death rates. This is thanks to better surgery methods and care before and after surgery. These changes have made outcomes for patients much better.
Overall 30-Day Mortality Statistics
Recent studies show the 30-day death rate for bariatric surgery is very low. Gastric bypass surgery, a common procedure, has a 30-day death rate of about 0.15 percent. Sleeve gastrectomy procedures have even lower rates, around 0.13 percent in 30 days.
These numbers show how far the field has come. Gastric bypass death rates range from 0.2% to 0.3%. For gastric sleeve, rates are about 0.1% to 0.2%. These improvements come from better surgery and care before and after surgery.
Historical Trends in Surgical Safety
Bariatric surgery has changed a lot over the years, making it safer. We’ve seen death rates go down thanks to better surgery and care. Laparoscopic techniques and better patient choices have been key in this progress.
As we keep improving bariatric surgery, watching death rates is key to better patient results. By looking at past trends and current numbers, we can understand the risks and benefits of these surgeries better.
Mortality Rates by Procedure Type
When thinking about bariatric surgery, it’s key to know the death rates for each type. Bariatric surgery includes many procedures aimed at weight loss. But, the death rates differ for each one.
Gastric Bypass Surgery
Gastric bypass surgery, or Roux-en-Y gastric bypass, is a common choice. It has a 30-day death rate of about 0.15%. This surgery makes a small pouch from the stomach and connects it to the small intestine. It’s effective, leading to 65% to 77% weight loss, but it’s riskier than some other surgeries.
Sleeve Gastrectomy
Sleeve gastrectomy is popular for its good results and lower risks. Its 30-day death rate is around 0.13%. This surgery removes most of the stomach, leaving a narrow “sleeve.” It leads to 60% to 70% weight loss. Its lower death rate and good results make it a good choice for many.
Gastric Banding
Gastric banding, or laparoscopic adjustable gastric banding, is less invasive. It has a death rate of 0.02% to 0.03%. This surgery puts a band around the stomach to make a small pouch. It’s safer but leads to less weight loss, about 40% to 50%.
Knowing these death rates helps patients choose the right bariatric surgery. It’s important to talk about risks and benefits with a healthcare expert.
Common Causes of Mortality After Bariatric Surgery
Knowing the common causes of death after bariatric surgery helps in reducing risks. Bariatric surgery is mostly safe, but serious complications can happen. These complications can be deadly.
Several factors lead to death after bariatric surgery. Cardiovascular events, pulmonary complications, and infections are the main causes. It’s important to understand these risks to improve patient care and inform patients about dangers.
Pulmonary Embolism
Pulmonary embolism is a major risk after bariatric surgery. It happens when a blood clot blocks blood flow in the lungs. Preventive measures like anticoagulants and compression stockings are key to lowering this risk.
Anastomotic Leaks
Anastomotic leaks are serious and can be deadly. These leaks occur when the surgical connection between parts of the intestine breaks. This allows digestive contents to leak into the abdomen, leading to severe infection and sepsis if not treated quickly.
Quick diagnosis and treatment are vital for managing anastomotic leaks. Surgeons and healthcare teams must watch for signs like fever, abdominal pain, and fast heart rate in patients.
Sepsis and Infection
Sepsis and infection are big risks after bariatric surgery. Sepsis is when the body’s response to an infection gets out of control. In bariatric surgery, sepsis can come from infections, leaks, or pneumonia.
Early recognition and treatment of sepsis are key to saving lives. Healthcare providers need to know the signs of sepsis, like fever, fast heart rate, and organ failure. They must start treatment right away.
Risk factors for death after bariatric surgery include higher body mass index, older age, male gender, and certain health conditions. Knowing these risk factors helps in identifying patients who need more careful pre and post-surgery care.
Risk Factors Affecting Surgical Outcomes
The success and safety of bariatric surgery depend on many risk factors. It’s important to know how certain patient characteristics can affect the outcome. This knowledge is key when considering bariatric surgery.
Impact of BMI on Mortality Risk
A higher Body Mass Index (BMI) raises the risk of death after bariatric surgery. Patients with a higher BMI need more careful preoperative and postoperative care. Studies show that a higher BMI increases the risk of complications.
Age and Gender Considerations
Older age and being male also increase the risk of death after surgery. Older patients and men face a higher risk of complications. These factors must be considered during the preoperative assessment.
Pre-existing Medical Conditions
Conditions like type 2 diabetes, hypertension, and metabolic dysfunction–associated steatotic liver disease (MASLD) can affect surgery outcomes. Preoperative optimization of these conditions is vital to reduce risks. A thorough preoperative evaluation is recommended to manage these conditions well.
By understanding and addressing these risk factors, we can make bariatric surgery safer and more successful for our patients.
Cardiovascular and Respiratory Risk Factors
Patients getting bariatric surgery often have heart and lung problems. These issues can affect how safe and effective the surgery is.
Pulmonary Hypertension
Pulmonary hypertension means high blood pressure in the lungs’ blood vessels. It’s a big risk for death after surgery. It’s important to check and manage it before surgery to lower risks.
Congestive Heart Failure
Congestive heart failure (CHF) is when the heart doesn’t pump well. It can cause problems during and after surgery. Improving heart function before surgery helps avoid bad outcomes.
Sleep Apnea and Respiratory Compromise
Sleep apnea is common in the obese and can cause breathing problems during surgery. Using CPAP therapy is key to avoid breathing issues.
Understanding and managing heart and lung risks can make bariatric surgery better. A thorough check before surgery helps find and fix these risks.
Liver Disease and Other Medical Considerations
Liver disease can make bariatric surgery more complicated. It’s important to carefully evaluate each case. Liver disease is a big concern because it can affect surgery results.
Impact of Liver Disease on Surgical Risk
Liver disease, like non-alcoholic steatohepatitis (NASH), is common in bariatric surgery patients. It can raise the risk of problems during and after surgery. Careful assessment of liver function is key to reduce these risks. We check liver health with imaging, tests, and sometimes a biopsy.
Diabetes and Metabolic Factors
Diabetes is also a big factor in bariatric surgery results. Patients with diabetes often have impaired metabolic function. This can impact how well they do after surgery. It’s important to manage diabetes well before, during, and after surgery.
Metabolic factors like insulin resistance and metabolic syndrome also matter. By understanding and addressing these, we can tailor our approach to each patient. This improves their chances of success.
Minimizing Your Personal Risk Factors
Understanding and reducing personal risk factors is key to safe bariatric surgery. Taking proactive steps can greatly improve outcomes and lower complication risks.
Selecting a Skilled Surgeon
Choosing an experienced surgeon is critical. A surgeon with many successful procedures can greatly impact patient results. The
“American Society for Metabolic and Bariatric Surgery (ASMBS), ‘the expertise of the surgeon is a critical factor in the success of bariatric surgery'”
. Look for a surgeon with good credentials, experience, and patient feedback.
Pre-Surgical Preparation
Pre-surgical optimization is vital. It includes a detailed nutritional assessment and managing any health issues. Preoperative optimization may involve diet changes, weight loss, and medication adjustments. This step can enhance health before surgery, leading to better results and fewer complications.
Adhering to Post-Operative Guidelines
Following post-operative instructions is also key. This means sticking to a special diet, attending follow-ups, and making lifestyle changes. Postoperative care is essential for long-term success. It helps avoid issues like nutritional deficiencies and weight gain.
By picking a skilled surgeon, preparing well before surgery, and following post-op advice, patients can greatly reduce risks. This leads to a successful bariatric surgery outcome.
Conclusion: Balancing Risks and Benefits of Bariatric Surgery
Bariatric surgery helps with weight loss and improves health problems linked to obesity. It has a low death rate. Studies show it can make people live longer and feel better overall.
The good things about bariatric surgery, like losing weight and fixing health issues, are more important than the bad. This makes it a good choice for many people. Understanding and reducing risks helps patients get the most health benefits.
In short, bariatric surgery is a safe and effective way to fight obesity. By looking at both the good and bad sides, patients and doctors can make the best choices together.
FAQ
What is the overall mortality rate for bariatric surgery?
The 30-day death rate after bariatric surgery is about 0.1 to 0.15 percent.
How do mortality rates vary by bariatric surgery procedure type?
Rates differ by procedure. Gastric bypass has a 0.15% rate. Sleeve gastrectomy is at 0.13%. Gastric banding ranges from 0.02-0.03%.
What are the most common causes of mortality after bariatric surgery?
Common causes of death include pulmonary embolism, anastomotic leaks, and sepsis.
How does BMI impact mortality risk in bariatric surgery?
A higher BMI increases the risk of death after surgery.
What pre-existing medical conditions affect bariatric surgery outcomes?
Conditions like diabetes, hypertension, and heart failure can greatly affect outcomes.
How can patients minimize their personal risk factors for bariatric surgery?
Patients can reduce risks by choosing an experienced surgeon and following post-op instructions.
What is the impact of liver disease on bariatric surgery risk?
Liver disease can significantly raise surgical risks, requiring careful evaluation.
How has the mortality rate for bariatric surgery changed over time?
The death rate has dropped over years due to better techniques and care.
What are the benefits of bariatric surgery in terms of weight loss and comorbidity improvement?
Surgery offers significant weight loss and improves conditions like diabetes and hypertension.
What is the mortality rate for gastric sleeve surgery?
Gastric sleeve surgery’s death rate is about 0.13%.
Are there any specific risk factors that increase the likelihood of complications after bariatric surgery?
Yes, older age, male gender, and certain medical conditions raise complication risks.







