Last Updated on November 27, 2025 by Bilal Hasdemir

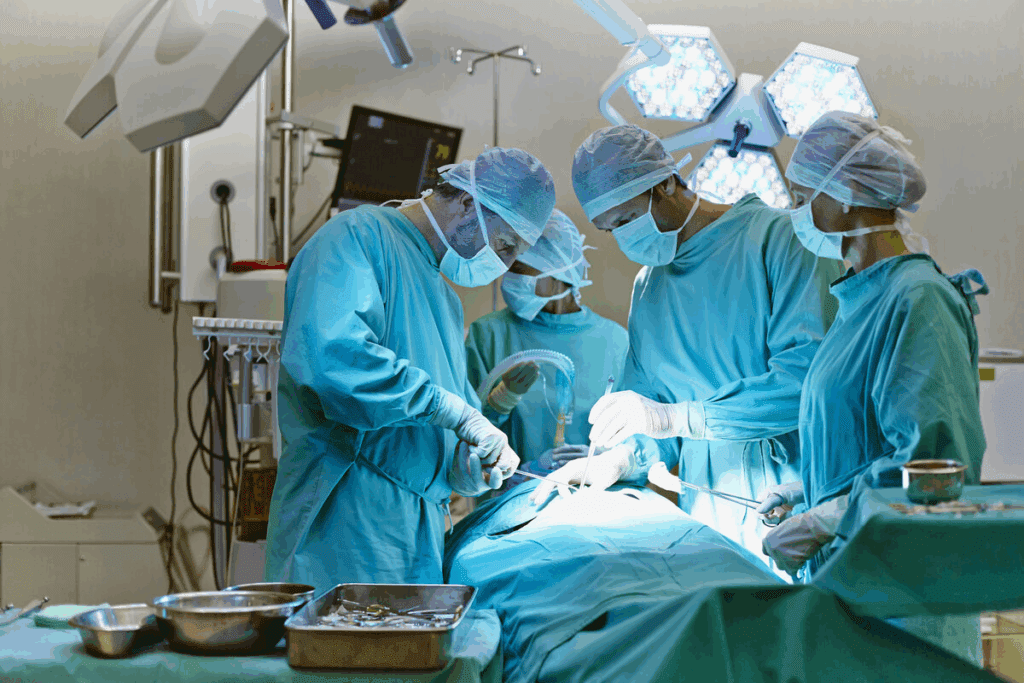
Surgical procedures are known to carry inherent risks, and some are considered more perilous than others. Brain surgery, heart surgery, and transplant surgeries are among the most complex and risky procedures.
The complexity of these surgeries is attributed to various factors, including the delicate nature of the organs involved and the high level of precision required. Understanding the risks and complications associated with these procedures is crucial for patients and medical professionals alike.
Key Takeaways
- Certain surgeries are considered riskier due to their complexity and the organs involved.
- Brain, heart, and transplant surgeries are among the most challenging procedures.
- The mortality and complication rates for these surgeries vary based on several factors.
- Understanding the risks is essential for informed decision-making.
- Medical professionals must exercise high precision and care during these procedures.
The Evolution of High-Risk Surgical Procedures

Surgical procedures have undergone substantial evolution, from primitive battlefield amputations to sophisticated modern operations. This transformation reflects broader advancements in medical science and technology, significantly impacting how high-risk surgeries are performed today.
From Battlefield Amputations to Modern Operating Rooms
The history of surgery is replete with examples of high-risk procedures, many of which were initially developed to address emergency situations on the battlefield. Early surgical interventions were often crude and associated with high mortality rates. For instance, amputations were commonly performed without the benefit of anesthesia or sterile conditions, leading to frequent complications and deaths.
The advent of modern surgical techniques, antiseptic practices, and anesthesia marked a significant turning point in the history of surgery. These advancements enabled surgeons to perform more complex procedures with greater safety, laying the groundwork for the sophisticated surgical practices seen today.
How Mortality Rates Have Changed Over Time
Mortality rates associated with surgical procedures have decreased dramatically over the centuries, thanks to improvements in surgical techniques, patient care, and post-operative management. Statistical analyses of surgical outcomes have shown a steady decline in mortality rates for various procedures, including those considered high-risk.
Despite these improvements, certain surgical procedures continue to carry significant risks. Understanding the historical context and evolution of these high-risk surgeries is crucial for appreciating the challenges they pose and the ongoing efforts to improve outcomes.
How Surgical Risk is Measured and Evaluated
Surgical risk assessment is a multifaceted process that involves evaluating various factors to determine the likelihood of complications during and after surgery. This complex evaluation is crucial for healthcare professionals to make informed decisions and for patients to understand the potential risks associated with their surgical procedures.
Statistical Methods for Assessing Surgical Mortality
Statistical methods play a vital role in assessing surgical mortality. These methods include risk-adjusted mortality rates and complication rates, which provide a quantifiable measure of surgical risk. By analyzing these statistics, healthcare providers can better understand the risks associated with different procedures and improve patient outcomes.
The use of risk-adjusted mortality rates allows for a more accurate comparison of surgical outcomes across different institutions and surgeons. This adjustment is crucial because it accounts for variations in patient populations, such as age, comorbidities, and the complexity of the procedures performed.
Factors That Determine Surgical Risk Classification
Several factors contribute to the classification of surgical risk. These include patient health status, the complexity of the surgical procedure, and the expertise of the surgical team. Understanding these factors is essential for accurately assessing surgical risk and making informed decisions.
| Factor | Description | Impact on Surgical Risk |
| Patient Health Status | Pre-existing conditions, age, and overall health | Higher risk for patients with significant comorbidities |
| Procedure Complexity | Technical difficulty and invasiveness of the procedure | More complex procedures generally carry higher risk |
| Surgeon Expertise | Experience and skill level of the surgical team | Higher expertise is associated with lower complication rates |
By considering these factors and utilizing statistical methods, healthcare professionals can effectively measure and evaluate surgical risk. This comprehensive approach enables better patient care and improved outcomes.
The Most Dangerous Surgery: Craniopagus Twin Separation
The surgical separation of craniopagus twins is considered a high-stakes operation due to their shared brain tissue. This complex procedure requires a multidisciplinary team of experts with extensive experience in neurosurgery and pediatric care.
Anatomical Challenges of Conjoined Brain Tissue
Craniopagus twins are conjoined at the head, and their brains are often connected in complex ways, making separation a daunting task. The shared vascular and neural structures pose significant anatomical challenges, requiring meticulous preoperative planning and precise surgical techniques.
The surgical team must carefully evaluate the twins’ brain anatomy using advanced imaging techniques such as MRI and CT scans. This information is crucial in determining the feasibility of separation and planning the surgical approach.
Notable Cases and Their Outcomes
Several notable cases of craniopagus twin separation have been documented, highlighting the complexity and risks involved. One such case involved twins conjoined at the back of their heads, sharing a major blood vessel. The surgical team successfully separated the twins, but the procedure required over 24 hours of surgery and a highly skilled team.
The outcomes of craniopagus twin separation surgeries vary widely, depending on the extent of the connection and the overall health of the twins. While some separations are successful with minimal long-term complications, others may result in significant neurological deficits or even mortality.
| Case | Year | Outcome |
| Twins A | 2010 | Successful separation with minimal complications |
| Twins B | 2015 | Separation resulted in significant neurological deficits |
| Twins C | 2018 | Successful separation with good long-term outcomes |
These cases underscore the importance of careful planning, advanced surgical techniques, and a skilled multidisciplinary team in achieving successful outcomes in craniopagus twin separation surgeries.
Hemicorporectomy: Surviving Half a Body
In cases of severe trauma or life-threatening conditions, hemicorporectomy may be considered as a last resort. This extreme surgical procedure involves the removal of the lower half of the body, a drastic measure that poses significant risks to the patient’s survival and quality of life.
When This Extreme Procedure is Considered
Hemicorporectomy is typically considered in cases where the patient’s lower body is severely damaged or diseased beyond recovery. The decision to undergo this surgery is made after all other treatment options have been exhausted. Severe trauma, malignant tumors, and life-threatening infections are some of the conditions that may necessitate hemicorporectomy.
- Severe trauma to the lower body
- Malignant tumors in the pelvic region
- Life-threatening infections
The surgical team must carefully evaluate the patient’s condition and consider the potential outcomes before proceeding with hemicorporectomy. This involves a thorough assessment of the patient’s overall health, the extent of the damage or disease, and the likelihood of survival.
Long-term Survival and Quality of Life
The long-term survival and quality of life for patients undergoing hemicorporectomy are significant concerns. While some patients have survived this procedure, the quality of life post-surgery can be challenging due to the extensive nature of the operation. Patients require ongoing care and rehabilitation to manage their condition and adapt to their new circumstances.
- Post-operative care and management
- Rehabilitation and physical therapy
- Ongoing psychological support
Despite the challenges, advancements in surgical techniques and post-operative care have improved outcomes for some patients. The decision to undergo hemicorporectomy requires careful consideration and a comprehensive understanding of the potential risks and benefits.
Complex Cardiac Surgeries With High Mortality Rates
Advanced cardiac surgical procedures, while lifesaving, are associated with significant risks and mortality. These complex surgeries demand not only the expertise of skilled surgeons but also cutting-edge technology and comprehensive post-operative care to improve patient outcomes.
Aortic Dissection Repair: Racing Against Time
Aortic dissection repair is one of the most critical and complex cardiac surgeries. It involves fixing a tear in the aorta, the major artery that carries blood from the heart. This condition is life-threatening and requires immediate surgical intervention. The complexity of this procedure lies in the delicate nature of the aorta and the need for precise surgical techniques to repair or replace the affected section.
The urgency of aortic dissection repair cannot be overstated. The faster the surgery is performed, the better the chances of survival for the patient. Surgical teams must work with precision and speed, utilizing advanced imaging techniques and monitoring to navigate the intricacies of the aorta.
Multiple Valve Replacements and Reconstructions
Multiple valve replacements and reconstructions are another category of complex cardiac surgeries with high mortality rates. These procedures involve repairing or replacing more than one of the heart’s valves, which are crucial for maintaining proper blood flow. The complexity arises from the need to address multiple valves, each requiring precise repair or replacement, while ensuring the overall function of the heart is maintained or improved.
The success of these surgeries depends on various factors, including the patient’s overall health, the severity of the valve dysfunction, and the surgical team’s experience. Advanced surgical techniques, including minimally invasive procedures, are being increasingly used to reduce recovery times and improve outcomes.
Understanding the risks and potential outcomes of these complex cardiac surgeries is crucial for both medical professionals and patients. By examining surgical outcome statistics and the factors influencing them, we can better appreciate the challenges and advancements in this field of medicine.
Multi-Organ Transplant Procedures
Surgical teams undertaking multi-organ transplants face a myriad of technical and immunological challenges. These complex operations involve transplanting multiple organs simultaneously, requiring a high degree of coordination and expertise among the surgical team.
Technical Challenges of Simultaneous Transplantation
The technical challenges associated with multi-organ transplants are significant. Simultaneous transplantation of multiple organs demands precision and a deep understanding of the intricate relationships between the organs being transplanted. The surgical team must be adept at handling unexpected complications that may arise during the procedure.
One of the key technical challenges is the coordination among multiple surgical teams. Each team must work in harmony to ensure that the transplantation process is carried out smoothly. This requires not only technical skill but also excellent communication and teamwork.
Immunological Complications and Rejection Risks
Immunological complications are a major concern in multi-organ transplant procedures. The introduction of multiple foreign organs can trigger a severe immune response, increasing the risk of rejection. Careful patient management and immunosuppressive therapy are crucial for mitigating these risks.
To minimize the risk of rejection, patients undergo rigorous testing to ensure compatibility between the donor organs and the recipient’s immune system. Despite these precautions, the risk of immunological complications remains a significant challenge in the field of multi-organ transplantation.
Face Transplant Surgery: Risks Beyond Survival
As a highly complex and relatively new field, face transplant surgery poses significant technical and psychological risks. This innovative procedure involves not only the transplantation of a donor face but also the reconnection of delicate vascular and nerve structures, making it one of the most challenging surgeries in modern medicine.h
Vascular and Nerve Reconnection Challenges
The technical challenges of face transplant surgery are multifaceted. One of the primary concerns is the reconnection of vascular structures. The surgery requires precise microsurgical techniques to reattach arteries and veins, ensuring proper blood flow to the transplanted tissue. Any complications during this process can lead to graft failure or other serious complications.
Nerve reconnection is another critical aspect. The procedure involves reconnecting sensory and motor nerves to restore function and sensation to the transplanted face. This requires not only technical skill but also a deep understanding of the complex nerve anatomy involved.
Psychological and Identity Complications
Beyond the technical challenges, face transplant patients often face significant psychological and identity complications. Adjusting to a new facial appearance can be a profound experience, affecting a patient’s self-perception and identity. Studies have shown that patients may experience a range of emotions, from excitement and gratitude to anxiety and depression.
The psychological impact of face transplantation is an area of ongoing research. Surgical complication studies have highlighted the need for comprehensive psychological support both before and after the surgery to help patients navigate these complex emotions and adapt to their new appearance.
In conclusion, while face transplant surgery offers new possibilities for patients with severe facial disfigurement, it is crucial to carefully consider the associated risks and complications. By understanding these challenges, both patients and healthcare providers can better prepare for the complex journey involved in face transplantation.
Artificial Heart Implantation and Mechanical Circulatory Support
Advanced heart failure treatment now includes artificial heart implantation and mechanical circulatory support, significantly improving patient outcomes. These critical interventions are designed for patients with severe heart failure who have not responded to other treatments.
Artificial heart implantation involves replacing a patient’s failing heart with a mechanical device, either as a bridge to heart transplantation or as destination therapy. Mechanical circulatory support devices, including total artificial hearts and ventricular assist devices, support the heart’s function, improving circulation and reducing the workload on the heart.
Total Artificial Heart vs. Ventricular Assist Devices
The choice between a total artificial heart and ventricular assist devices depends on the patient’s condition and the extent of heart failure. Total artificial hearts replace both ventricles and are used when both sides of the heart are failing. In contrast, ventricular assist devices support one or both ventricles, depending on the device and patient need.
“The total artificial heart is a lifeline for patients with biventricular failure, offering a chance at survival until transplantation.”
Long-term Complications and Survival Rates
While artificial heart implantation and mechanical circulatory support can be life-saving, they are associated with significant long-term complications. These include infection, thrombosis, and device failure. Understanding the risks and benefits is crucial for making informed decisions.
Survival rates vary depending on the device, patient condition, and other factors. Studies have shown that with proper management, patients with these devices can achieve improved survival and quality of life.
According to recent data, the one-year survival rate for patients with ventricular assist devices is approximately 80%, highlighting the potential for these devices to significantly improve outcomes.
High-Risk Neurosurgical Procedures
High-risk neurosurgical procedures demand precision and expertise, given the potential for significant complications. Neurosurgery, a field that deals with surgical treatments of the brain and nervous system, encompasses some of the most complex and delicate operations in medicine.
Awake Craniotomy for Eloquent Brain Regions
Awake craniotomy is a procedure where the patient remains awake during part of the surgery. This technique is used to remove brain tumors or epileptic foci located in eloquent areas of the brain, which control critical functions such as speech, movement, and sensation.
- Benefits: Allows for real-time monitoring of brain function, reducing the risk of damaging critical areas.
- Challenges: Requires careful patient selection, precise anesthesia, and the ability to manage potential complications during the procedure.
Brainstem and Deep Brain Tumor Resection
Brainstem and deep brain tumors are particularly challenging due to their location and proximity to critical brain structures. Surgical resection of these tumors requires advanced techniques and a thorough understanding of brain anatomy.
- Surgical Risks: Include damage to surrounding brain tissue, neurological deficits, and potential for stroke or infection.
- Advancements: Improved imaging techniques, microsurgical tools, and intraoperative monitoring have enhanced the safety and efficacy of these procedures.
Understanding the risks and benefits of these high-risk neurosurgical procedures is crucial for both surgeons and patients. By leveraging advanced surgical techniques and technologies, the outcomes of these complex operations can be significantly improved.
Emergency Trauma Surgeries With Critical Mortality Rates
The realm of emergency trauma surgery is characterized by high-stakes decision-making and rapid intervention. Emergency trauma surgeries are performed under extreme pressure, with the patient’s condition often deteriorating rapidly. These surgeries require a high level of skill and precision from the surgical team.
In such critical situations, the management of polytrauma patients becomes a significant challenge. Polytrauma management involves a comprehensive approach to stabilize the patient, addressing multiple injuries simultaneously.
Polytrauma Management in Unstable Patients
Managing polytrauma in unstable patients requires a coordinated effort from a multidisciplinary team. The initial assessment is crucial, as it sets the stage for subsequent interventions. The team must work efficiently to identify and address life-threatening injuries.
“The key to successful polytrauma management lies in the ability to prioritize and act swiftly,” says a leading trauma surgeon. Effective communication among team members is vital to ensure that all aspects of the patient’s care are addressed promptly.
Damage Control Surgery Principles
Damage control surgery is a critical strategy employed in emergency trauma situations. The primary goal is to control bleeding and contamination, thereby preventing further deterioration of the patient’s condition. This approach allows for stabilization before definitive repair is undertaken.
The principles of damage control surgery include rapid control of hemorrhage, thorough assessment of injuries, and temporary closure of wounds. This staged approach enables surgeons to manage complex trauma cases more effectively.
In conclusion, emergency trauma surgeries, including those involving polytrauma management and damage control surgery, require a highly skilled and coordinated response from medical teams. By understanding the principles and challenges of these procedures, healthcare providers can improve outcomes for critically injured patients.
Surgical Risk Factors in Critically Ill Patients
Critically ill patients undergoing surgery face a complex array of risk factors that can significantly impact their outcomes. The presence of underlying health conditions, the nature of the surgical procedure, and the patient’s overall physiological reserve all contribute to the risk profile.
Impact of Age and Pre-existing Conditions
Age is a significant factor in surgical risk, as older patients often have reduced physiological reserves and a higher prevalence of comorbid conditions such as diabetes, hypertension, and heart disease. These pre-existing conditions can complicate surgical procedures and postoperative care, increasing the risk of adverse outcomes.
Pre-existing conditions that are particularly relevant include cardiovascular disease, chronic obstructive pulmonary disease (COPD), and diabetes mellitus. These conditions not only increase the risk of surgical complications but also affect the patient’s ability to recover from surgery.
Emergency vs. Elective Procedures: Risk Comparison
The distinction between emergency and elective surgical procedures is crucial in assessing risk. Emergency surgeries are often performed under less than ideal circumstances, with less time for preoperative optimization and a higher likelihood of complications. In contrast, elective procedures allow for thorough preoperative evaluation and planning, potentially reducing risks.
Understanding the differences in risk between emergency and elective procedures is essential for clinicians to make informed decisions and for patients to be aware of the potential risks and benefits associated with their surgical options.
Experimental Surgical Procedures on the Frontier
Surgical innovation is on the cusp of a revolution with the development of experimental procedures like xenotransplantation and gene therapy. These cutting-edge medical interventions are designed to address complex health issues that have long been considered incurable or challenging to treat.
The exploration of such experimental surgical procedures represents a significant shift in medical science, offering new avenues for treatment and potentially improving patient outcomes. However, these procedures also come with their own set of challenges and uncertainties.
Xenotransplantation: Animal Organs in Humans
Xenotransplantation involves transplanting organs or tissues from one species to another, typically from animals to humans. This procedure is being explored as a potential solution to the shortage of human organs available for transplantation.
The use of xenotransplantation raises several considerations, including the risk of zoonotic infections and the need for immunosuppression to prevent organ rejection. Researchers are working to overcome these challenges through genetic modification of donor animals and the development of new immunosuppressive therapies.
| Aspect | Challenge | Potential Solution |
| Zoonotic Infections | Risk of transmitting animal viruses to humans | Genetic screening and modification of donor animals |
| Immunosuppression | Need for lifelong immunosuppressive drugs | Development of targeted immunosuppressive therapies |
Emerging Gene and Cell Therapy Surgical Applications
Gene and cell therapies represent another frontier in surgical innovation, offering the potential to treat a wide range of diseases at the molecular level. These therapies involve either correcting genetic defects or using cells to repair or replace damaged tissues.
One of the key challenges in gene and cell therapy is ensuring the safe and effective delivery of therapeutic genes or cells to the target site. Researchers are exploring various techniques, including viral vectors and biomaterials, to enhance the efficacy of these therapies.
“The future of surgery lies not just in the technical skill of the surgeon, but in the innovative application of science to solve previously unsolvable problems.”
A renowned surgeon and researcher
As these experimental surgical procedures continue to evolve, it is crucial to carefully evaluate their safety and efficacy through rigorous clinical trials. The potential benefits of these innovations must be weighed against the risks, and ongoing research is needed to fully realize their therapeutic potential.
How Hospitals Measure and Compare Surgical Mortality Rates
The assessment of surgical mortality rates involves complex statistical analysis to account for varying patient conditions and procedural complexities. Hospitals and healthcare systems use various metrics to evaluate their performance in surgical care.
Risk-Adjusted Mortality Statistics
Risk-adjusted mortality statistics are crucial for comparing surgical outcomes across different hospitals and healthcare systems. These statistics adjust for the varying levels of risk associated with different patient populations and surgical procedures. By doing so, they provide a more accurate comparison of surgical quality. Risk adjustment is essential because it helps to level the playing field, allowing for fair comparisons between institutions that may have different patient demographics and case complexities.
For instance, a hospital that frequently performs high-risk surgeries may appear to have a higher mortality rate than a hospital that performs less complex procedures. However, after risk adjustment, the comparison becomes more nuanced, reflecting the true quality of care provided by each institution.
Volume-Outcome Relationship in High-Risk Procedures
The volume-outcome relationship is another critical factor in understanding surgical mortality rates. Research has shown that higher-volume centers tend to have better outcomes for high-risk procedures. This is because higher volume often correlates with greater experience and expertise among surgical teams.
A notable study highlighted that “hospitals with higher volumes of complex surgeries tend to have lower mortality rates, underscoring the importance of experience in surgical care.” This relationship is attributed to several factors, including improved preoperative care, refined surgical techniques, and enhanced postoperative management.
“The relationship between volume and outcome is a critical consideration in the organization of surgical services, suggesting that centralization of complex procedures can lead to better patient outcomes.”
Understanding the volume-outcome relationship can inform healthcare policy and guide patients towards hospitals with better outcomes for specific procedures.
Reducing Mortality in the World’s Most Dangerous Surgeries
Reducing mortality in complex surgeries requires a dual approach, focusing on technological innovation and specialized surgical expertise. As surgical procedures become increasingly intricate, the need for advanced technology and highly skilled teams has never been more critical.
Technological Innovations Improving Outcomes
Technological advancements have revolutionized the field of surgery, offering new tools and techniques that significantly improve patient outcomes. Robotic surgery, for instance, allows for greater precision and flexibility, enabling surgeons to perform complex procedures with enhanced accuracy. Additionally, advanced imaging technologies provide real-time data during surgery, helping to identify potential complications early.
Another significant innovation is the use of 3D printing in surgical planning. By creating detailed models of patient anatomy, surgeons can better understand the complexities of each case and plan their approach more effectively. This not only improves surgical precision but also reduces the risk of complications.
Specialized Multidisciplinary Surgical Teams
The importance of specialized multidisciplinary surgical teams cannot be overstated. These teams bring together experts from various fields, including surgery, anesthesiology, and critical care, to provide comprehensive care for patients undergoing high-risk surgeries. By working together, these teams can anticipate and manage potential complications more effectively, improving overall patient outcomes.
Effective communication is a critical component of successful multidisciplinary teams. By ensuring that all team members are informed and aligned, surgical teams can respond quickly to changing circumstances during surgery, further enhancing patient safety.
Conclusion
Surgical procedures carry inherent risks, and some are considered more dangerous than others. Understanding these risks is essential for making informed decisions about surgical interventions.
The most dangerous surgeries are complex and high-risk procedures that require careful consideration and planning. By acknowledging the challenges and complexities of these procedures, we can work towards reducing mortality rates and improving the quality of care for patients undergoing high-risk surgeries.
Reducing surgical risks requires a multifaceted approach, including technological innovations, specialized multidisciplinary surgical teams, and a thorough understanding of the risks and complications associated with these surgeries. As medical professionals continue to advance their knowledge and skills, patients can expect better outcomes and improved quality of life.
Ultimately, the key to successful surgical outcomes lies in a comprehensive understanding of surgical risks and a commitment to delivering high-quality care. By prioritizing patient safety and well-being, we can minimize the risks associated with the most dangerous surgeries.
FAQ
What is craniopagus twin separation, and what are the risks involved?
Craniopagus twin separation is a complex surgical procedure that involves separating conjoined twins who share brain tissue. The risks involved include significant anatomical challenges, unpredictable outcomes, and a high risk of complications, such as neurological deficits, infection, and stroke.
What is hemicorporectomy, and when is it considered?
Hemicorporectomy is an extreme surgical procedure that involves removing the lower half of the body. It is typically considered in cases of severe trauma or disease, where the patient’s life is at risk. The decision to undergo this surgery requires careful consideration and a thorough understanding of the potential outcomes.
What are the risks associated with complex cardiac surgeries?
Complex cardiac surgeries, such as aortic dissection repair and multiple valve replacements, pose significant risks, including high mortality rates, complications, and the need for precise and timely intervention. The complexity of these procedures contributes to their high mortality rates, emphasizing the need for careful patient selection, skilled surgical teams, and advanced post-operative care.
What are the technical challenges of multi-organ transplant procedures?
Multi-organ transplant procedures pose significant technical challenges, including the need for coordination and expertise among the surgical team, as well as the risk of immunological complications and rejection. Careful patient management and immunosuppressive therapy are crucial for mitigating these risks.
What are the risks and benefits of face transplant surgery?
Face transplant surgery is a highly complex and innovative procedure that involves transplanting a donor face onto a recipient. The risks include technical challenges, such as reconnecting delicate vascular and nerve structures, as well as psychological and identity complications. The benefits include improved appearance and quality of life for the recipient.
What are the long-term complications associated with artificial heart implantation?
Artificial heart implantation and mechanical circulatory support devices are associated with significant long-term complications, including infection, thrombosis, and device failure. Understanding the risks and benefits of these devices is essential for making informed decisions about their use.
What are the risks associated with high-risk neurosurgical procedures?
High-risk neurosurgical procedures, such as awake craniotomy and brainstem tumor resection, pose significant risks, including neurological deficits, infection, and stroke. Understanding the risks and benefits of these procedures is essential for making informed decisions.
How do hospitals measure and compare surgical mortality rates?
Hospitals use various metrics to measure and compare surgical mortality rates, including risk-adjusted mortality statistics. These metrics help to account for differences in patient populations and procedure complexity.
What is the volume-outcome relationship in high-risk procedures?
The volume-outcome relationship refers to the observation that higher-volume centers tend to have better outcomes for high-risk procedures due to their increased experience and expertise.
How can mortality rates be reduced in high-risk surgeries?
Reducing mortality rates in high-risk surgeries requires a multifaceted approach, including technological innovations, such as advanced imaging and robotic surgery, as well as the use of specialized multidisciplinary surgical teams.
Reference:
National Center for Biotechnology Information (PMC). Surgical mortality and risk assessment insights. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4191488/ . Accessed October 14, 2025.