Last Updated on November 27, 2025 by Bilal Hasdemir

Did you know some surgeries are considered the most painful surgery procedures? The intensity of post-operative pain can vary widely depending on the type of surgery and the individual patient’s pain tolerance.
Procedures like thoracotomy, spinal fusion, and myomectomy are often listed among the most painful surgery experiences. However, determining exactly which is the most painful surgery is difficult because pain perception is subjective and differs from person to person.
This article explores what makes certain procedures the most painful surgery options. Factors such as tissue damage, incision size, and the patient’s overall health contribute to the level of discomfort.
By understanding the most painful surgery types and pain management strategies, patients can better prepare mentally and physically for recovery, and healthcare providers can improve post-operative care.
Key Takeaways
- Certain surgeries are known to be more painful than others.
- Pain intensity can vary greatly depending on the procedure and patient.
- Thoracotomy, spinal fusion, and myomectomy are often cited as painful surgeries.
- The subjective nature of pain makes it challenging to determine the most painful surgery.
- Understanding the factors that influence surgical pain is important.
Understanding Surgical Pain and Its Measurement
Understanding surgical pain is key to managing it well. It’s a complex and personal experience. People can feel different levels of pain even when they have the same surgery.
Doctors use many ways to measure surgical pain. Pain scales are a main tool. They help doctors know how much pain a patient is in.
Pain Scales Used in Medicine
Pain scales are vital for measuring surgical pain. There are a few common ones:
- The Numeric Rating Scale (NRS), where patients rate their pain from 0 to 10 or 0 to 100.
- The Faces Pain Scale (FPS), which uses facial expressions to help patients, like kids, show their pain.
- The Visual Analog Scale (VAS), a continuous scale that measures pain intensity.
| Pain Scale | Description | Usage |
| NRS | Rates pain from 0 to 10 or 0 to 100. | Commonly used for adults. |
| FPS | Uses facial expressions. | Often used for children. |
| VAS | Continuous scale for pain intensity. | Used for precise measurement. |
Subjective vs. Objective Pain Assessment
Pain assessment can be both subjective and objective. Subjective pain comes from what the patient says about their pain. Objective pain is seen through changes in the body and behavior.
Subjective pain assessment is important because pain is personal. Doctors use pain scales to understand this personal experience.
Objective indicators of pain include heart rate, blood pressure, and facial expressions. These signs help doctors understand pain levels, along with what the patient says.
Factors That Influence Surgical Pain Intensity
It’s important to know what makes surgical pain more intense. This knowledge helps in managing pain better for patients. Surgical pain is complex, influenced by both physical and psychological factors.
Tissue Trauma and Nerve Damage
Tissue trauma and nerve damage greatly affect surgical pain. Surgeries with more tissue damage, like big incisions, cause more pain. Nerve damage during surgery also increases pain by releasing chemicals that make pain worse.
Individual Pain Tolerance Variations
People’s pain tolerance varies a lot when they have surgery. Age, gender, genetics, and past pain experiences play a role. Some might naturally handle pain better due to their genes.
Psychological and Emotional Factors
Psychological and emotional factors also impact surgical pain. Anxiety, fear, and stress can make pain feel worse. But, a positive mindset and good coping skills can help reduce pain.
| Factor | Influence on Surgical Pain | Examples |
| Tissue Trauma | Increased pain due to tissue damage | Larger incisions, complex dissections |
| Nerve Damage | Potential for neuropathic pain | Nerve injury during surgery |
| Pain Tolerance | Variability in pain perception | Genetic factors, previous pain experiences |
| Psychological Factors | Impact on pain perception and coping | Anxiety, stress, positive outlook |
The Most Painful Surgery: Thoracotomy
The thoracotomy procedure is known for being very painful. It needs strong pain management. This surgery cuts into the chest to reach the lungs or other organs inside.
What is a Thoracotomy Procedure?
A thoracotomy is a big surgery that opens up the chest. It’s done for lung, heart, and esophageal surgeries. The cut goes through the chest wall, including skin, muscles, and sometimes ribs.
Why It Ranks as Extremely Painful
Thoracotomy is very painful because it hurts a lot of tissue and nerves. The big cut can cause a lot of pain after surgery. This pain is among the worst patients can feel.
The pain from thoracotomy comes from several things:
- The size and where the cut is made
- The damage to tissue and muscle
- Nerve irritation or damage
Patient Experiences and Recovery Timeline
Patients with thoracotomy often feel a lot of pain right after surgery. The recovery time can be long. It takes a while to get better.
| Recovery Stage | Timeline | Patient Experience |
| Immediate Post-operative | 0-3 days | Significant pain, managed with strong analgesics |
| Early Recovery | 3-14 days | Pain gradually decreases, mobility improves |
| Late Recovery | 2-6 weeks | Pain becomes manageable, return to light activities |
Surgical tips for managing pain include following a pain plan, doing gentle exercises, and going to follow-up appointments. This helps track how well you’re recovering.
Top Contenders for Most Painful Surgeries
Painful surgeries go beyond thoracotomy. They include many complex procedures that test patients and doctors. Pain varies from person to person. Yet, some surgeries are known for causing more pain due to their complexity and the body areas involved.
Complex Spinal Fusion Procedures
Spinal fusion joins two or more vertebrae together. It uses bone grafts, rods, and devices to stabilize the spine. This surgery treats spinal deformities, fractures, or degenerative conditions. The recovery is long and painful because of the surgery’s invasiveness and tissue damage.
Key aspects of spinal fusion surgery that contribute to its painful nature include:
- The harvesting of bone grafts from other parts of the body, which adds to the overall trauma.
- The use of instrumentation like rods and screws to stabilize the spine.
- The fusion process itself, which can lead to stiffness and discomfort.
Major Joint Replacement Operations
Joint replacement surgeries, like hip or knee replacements, replace damaged or arthritic joints with artificial ones. These surgeries can greatly improve life quality but are also very painful after. The pain comes from the incision, tissue manipulation, and the body’s reaction to the new prosthetic.
The recovery from joint replacement surgery requires extensive physical therapy, which, while vital for mobility and strength, can also be painful.
Extensive Abdominal and Bowel Resections
Abdominal and bowel resections remove diseased bowel parts or repair abdominal organ damage. These surgeries are very painful because of the sensitive abdominal cavity. They also risk complications like adhesions or ileus.
| Surgery Type | Common Pain Sources | Recovery Considerations |
| Complex Spinal Fusion | Bone graft harvesting, instrumentation | Lengthy recovery, possible stiffness |
| Major Joint Replacement | Surgical incision, tissue manipulation | Extensive physical therapy needed |
| Abdominal and Bowel Resections | Sensitivity of abdominal cavity, possible complications | Risk of adhesions or ileus, careful post-operative care needed |
Maxillofacial and Cranial Reconstructions
Maxillofacial and cranial reconstruction surgeries fix facial bone and skull defects or damage. They’re needed for trauma, congenital conditions, or tumors. These surgeries are very painful because of the delicate and complex structures involved.
Different surgeries show the need for tailored pain management. Knowing the pain risks and preparing can help improve recovery and the patient’s experience.
Patient Perspectives: Living Through the Most Painful Surgery
The most painful surgeries leave a big mark on patients. They shape their recovery journeys. Patients face big challenges, not just physically but also emotionally.
First-Hand Accounts of Surgical Pain
Patients share their stories, giving us a deep look into their pain. For example, a patient who had a thoracotomy said the pain felt like being crushed. This shows the intense physical discomfort of major surgeries.
Another patient, after a spinal fusion, had chronic pain for months. This pain didn’t just hurt their body. It also hurt their mental health.
Long-Term Physical and Emotional Recovery
Recovering from painful surgeries is a long and hard journey. Patients must heal physically and emotionally. Physical therapy and pain management are key to their recovery.
Emotional recovery is just as important. Many patients need support from loved ones or counselors. They face feelings of fear, anxiety, and relief. The support they get is vital to their recovery.
Understanding what patients go through helps healthcare providers. By knowing the physical and emotional challenges, they can give better care. This meets the full needs of their patients.
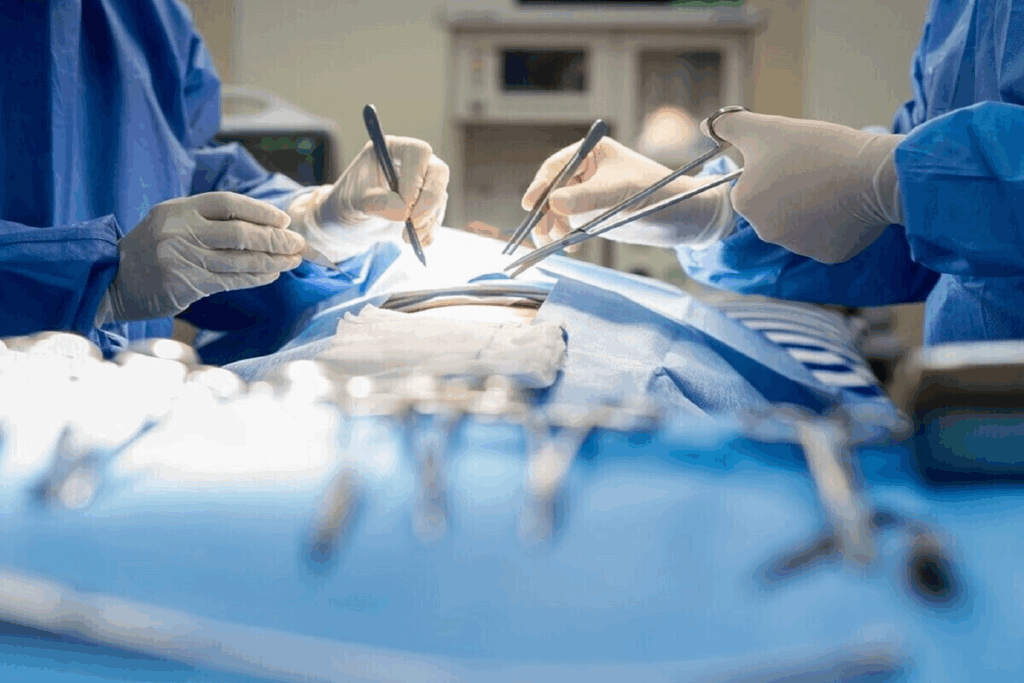
Comprehensive Pain Management for Major Surgeries
Pain management for major surgeries is a complex process. It covers pre-operative, intra-operative, and post-operative care. It’s not just about easing pain. It also helps avoid complications, speeds up recovery, and improves patient results.
Pre-operative Pain Prevention Strategies
Preventing pain before surgery is key. Pre-emptive analgesia is used to lessen post-operative pain. It involves giving pain relief medicine before surgery. Other methods include educating patients about pain management and using multimodal analgesia to target different pain pathways.
A study in a Journal found that pre-emptive analgesia reduces post-operative pain and boosts patient satisfaction.
“Pre-emptive analgesia has been shown to be effective in reducing post-operative pain and improving outcomes in patients undergoing major surgeries.”
Intra-operative Anesthesia Techniques
Anesthesia during surgery is critical for pain management. Regional anesthesia, like nerve blocks, numbs specific body areas. General anesthesia is also used, often with regional techniques for full pain control.
- Regional anesthesia, like epidural anesthesia, can cut down on the need for post-operative pain meds.
- Local anesthetics in wound infiltration enhance pain relief.
Post-operative Pain Control Methods
Managing pain after surgery is just as important. It involves both medicine and non-medicine strategies. Patient-controlled analgesia (PCA) lets patients give themselves pain relief as needed. Other methods include nonsteroidal anti-inflammatory drugs (NSAIDs) and adjuvant therapies like gabapentinoids for nerve pain.
Good post-operative pain management improves comfort and lowers the risk of complications. Experts say a detailed pain management plan can greatly improve recovery and shorten hospital stays.
Historical Context: Surgery Before Modern Pain Control
Before modern pain control, surgery was a last resort because of the intense pain. The history of surgery is complex. Early practices were very hard for patients.
Early Surgical Practices and Patient Experiences
In the past, surgeries were done without enough pain relief. This led to a lot of suffering for patients. Patients were often restrained or held down by assistants or family members. This was because anesthesia had not been invented yet.
Early surgeries were brutal and done in dirty conditions. There was no understanding of infection control or pain management. This made surgery a dangerous and painful experience.
The Revolutionary Impact of Anesthesia
Anesthesia was introduced in the mid-19th century and changed surgery. Ethers and other early anesthetics let patients go through surgery without feeling all the pain. This was a big change in medical history.
Anesthesia made surgeries better for patients. It let surgeons do more complex and longer surgeries. This was key in making surgery a real option for treating many conditions.
- Anesthesia became common, changing surgery.
- Surgeons could now focus on technique, not just speed.
- Patient outcomes got much better because of less pain and stress.
Looking back, anesthesia’s arrival was a major moment in surgery’s history. It opened the door to modern pain control methods. It continues to shape surgery today.
Modern Advancements Reducing the Pain of Surgery
Recent breakthroughs in medical technology have changed the surgical experience. They make post-operative pain less of an issue. Now, patients can recover more comfortably.
Minimally Invasive Surgical Techniques
Minimally invasive surgical techniques have made a big difference. They use smaller cuts, causing less damage and pain. Laparoscopic and robotic-assisted surgeries are now common. They help patients heal faster and feel less pain.
Targeted Nerve Blocks and Regional Anesthesia
Targeted nerve blocks and regional anesthesia are also key. They involve injecting anesthetics around specific nerves. This numbs the surgery area, reducing pain during and after surgery. It often means patients don’t need strong pain meds.
Future Innovations in Surgical Pain Management
Looking to the future, future innovations will likely improve pain management. New materials and technologies are being explored. This could include better nerve block methods and advanced pain apps and devices.
The field is constantly evolving to better care for patients. It aims to reduce the pain of surgery.
Conclusion
Understanding and managing surgical pain is key to better patient outcomes. Surgeries like thoracotomy and complex spinal fusions are very painful. They need strong pain management plans.
Good pain management uses many strategies. This includes preventing pain before surgery, using anesthesia during it, and controlling pain after. By understanding surgical pain, doctors can help patients more.
As medical tech gets better, so will pain management during surgery. This will help make recovery easier for patients. By focusing on pain management, we can make surgery less painful for everyone.
FAQ
What is elective surgery?
Elective surgery is planned ahead of time. It’s different from emergency surgery, which is urgent.
What are the most painful surgeries?
Thoracotomy, complex spinal fusion, major joint replacements, and big abdominal surgeries are very painful.
How long does it take to recover from surgery?
Recovery time varies. It depends on the surgery type, your health, and other factors. It can take weeks to months to fully recover.
What is the hardest surgery to recover from?
Surgeries with a lot of tissue damage, nerve issues, or complex repairs are tough. Thoracotomy and complex spinal fusion are examples.
What are the top 3 most painful surgeries?
Thoracotomy, complex spinal fusion, and major joint replacements are often the most painful. They cause a lot of tissue damage and are complex.
How much pain can the human body handle?
Pain tolerance varies. It depends on your mental state, emotional health, and past pain experiences.
What is the most common surgical procedure?
Common surgeries include cesarean sections, cataract surgeries, and orthopedic surgeries. The most common varies by region.
What surgeries have the most painful recovery?
Surgeries with a lot of tissue damage or complex repairs are painful. Thoracotomy and bowel resections are examples.
What is the bloodiest surgery?
Surgeries on major blood vessels or vascular areas are very bloody. This includes some cancer and trauma surgeries.
Are there surgeries that are considered worse than others in terms of pain?
Yes, surgeries like thoracotomy, complex spinal fusions, and some abdominal surgeries are very painful. They involve a lot of surgical intervention.
How has modern medicine reduced surgical pain?
Modern medicine has made surgery less painful. Advances in techniques and anesthesia, like targeted nerve blocks, have helped a lot.
What is the role of pre-operative pain prevention?
Pre-operative pain prevention helps reduce post-surgery pain. It includes certain medications and techniques that address pain pathways before surgery.
Can surgery on self be considered?
While some have tried self-surgery, it’s not safe. It risks infection and lacks proper anesthesia, leading to complications.
What is the impact of psychological factors on surgical pain?
Psychological factors greatly affect pain perception. Stress, anxiety, and expectations can change how pain is felt and reported.
Are there any future innovations in surgical pain management?
Yes, research is ongoing. New ERAS protocols, anesthesia techniques, and pain management strategies aim to reduce surgical pain further.
References
- Vrancken, D., et al. (2018). Procedure-specific pain intensity four days after surgery: A prospective cohort study. PLOS ONE, 13(11), e0208034. https://pmc.ncbi.nlm.nih.gov/articles/PMC6347732/