
At Liv Hospital, we aim to provide top-notch healthcare with full support for international patients. Accurate diagnosis of prostate cancer is key to good treatment. We use advanced imaging, like MRI-guided methods, to find cancer better.
Our method for finding prostate cancer uses MRI to pinpoint areas in the prostate gland for samples. This method is less invasive and has made finding cancer more accurate. It also cuts down on unnecessary biopsies. By focusing on specific areas seen as abnormal, we give more precise diagnoses.
Key Takeaways
- Advanced imaging techniques improve cancer detection rates.
- MRI-guided procedures enhance the accuracy of prostate cancer diagnosis.
- Minimally invasive procedures reduce the risk of unnecessary biopsies.
- Liv Hospital is a trusted leader in patient-centered care.
- Our approach focuses on targeting suspicious areas for tissue sampling.
Understanding Prostate Biopsy: Purpose and Importance

Patients need to understand the purpose and importance of a prostate biopsy. This procedure helps doctors find prostate cancer, a common issue for many men. We’ll look at what this procedure is, why it matters, and when it’s needed.
What Is a Prostate Biopsy?
A prostate biopsy is a way for doctors to check for cancer in the prostate gland. A urologist takes small tissue samples from the prostate. These samples are then looked at under a microscope for any signs of cancer.
When Is a Prostate Biopsy Necessary?
A biopsy is usually suggested when there’s a chance of prostate cancer. This includes an unusual digital rectal exam (DRE) or high prostate-specific antigen (PSA) levels. The choice to have a biopsy depends on several things, like your health history and test results.
Whether or not you need a biopsy depends on your personal risk factors and test results. For example, men with a family history of prostate cancer or very high PSA levels might need a biopsy of the prostate to check for cancer.
Evolution of Prostate Biopsy Techniques
Prostate biopsy methods have greatly improved over time, leading to better patient care. The shift from old methods to new, like MRI-guided prostate biopsy, has been key.
Traditional Biopsy Methods
For years, the transrectal ultrasound-guided (TRUS) biopsy was the main way to find prostate cancer. But it has its downsides. It can miss cancer spots because of sampling errors.
These old methods often use a random sampling approach. This might not hit the right spots, leading to missed cancers.
The Emergence of Advanced Imaging Approaches
New imaging tech, like MRI, has changed the prostate biopsy process. MRI-guided biopsies are now more accurate and reliable. They help find prostate cancer better.
Now, there are many types of prostate biopsies to choose from. Options include MRI-ultrasound fusion biopsy and in-bore direct MRI-guided biopsy. Each has its own benefits and fits different needs. We’ll look at these options in more detail later.
The MRI Prostate Biopsy Process and Technology
MRI technology has changed how we do prostate biopsies. Now, we can find and check suspicious spots better. This makes our cancer diagnosis more accurate.
Enhancing Detection with Magnetic Resonance Imaging
MRI is key in finding prostate cancer. It shows detailed pictures of the prostate. This helps us spot cancer early, which can lead to better treatment.
Key benefits of MRI in prostate biopsy include:
- Improved detection of clinically significant prostate cancer
- Enhanced visualization of the prostate gland and surrounding structures
- More accurate targeting of suspicious lesions
Target Identification and Precision Sampling
MRI-guided biopsies let us target specific spots. We use MRI images and biopsy data together. This way, we get tissue samples from the right places, reducing cancer misses.
| Feature | Traditional Biopsy | MRI-Guided Biopsy |
| Visualization | Limited detail | High-resolution imaging |
| Targeting | Systematic sampling | Precision targeting of suspicious lesions |
| Detection Rate | Variable | Improved detection of clinically significant cancer |
We’re always improving the MRI prostate biopsy method. By combining new imaging and biopsy tech, we aim to get even better at diagnosing prostate cancer. This will help us give our patients the best care possible.
Method 1: MRI-Ultrasound Fusion Biopsy
The MRI-ultrasound fusion biopsy is a big step forward in finding prostate cancer. It uses the best of MRI and ultrasound to spot cancer. This method is great for finding cancer in men with suspicious spots on MRI.
Fusion Technology Process
This biopsy method combines MRI images with ultrasound during the procedure. It starts with an MRI scan to find and mark cancerous areas. Then, during the biopsy, a special device uses both MRI and ultrasound to find these spots.
Accuracy and Detection Rates
This biopsy method makes finding prostate cancer more accurate. Studies show it can find serious cancer better than old methods. It lets doctors target specific areas with more precision, missing less cancer.
The main advantages of MRI-ultrasound fusion biopsy are:
- Improved accuracy in targeting suspicious lesions
- Enhanced detection of clinically significant prostate cancer
- Reduced need for repeat biopsies
- Better characterization of cancer aggressiveness
This method combines MRI and ultrasound to diagnose prostate cancer more accurately. It helps find cancer early and plan better treatments. This could lead to better patient outcomes.
Method 2: In-Bore Direct MRI Guided Prostate Biopsy
We use In-Bore Direct MRI Guided Prostate Biopsy to find advanced prostate cancer. This method lets us target prostate lesions with great accuracy. It uses real-time MRI images.
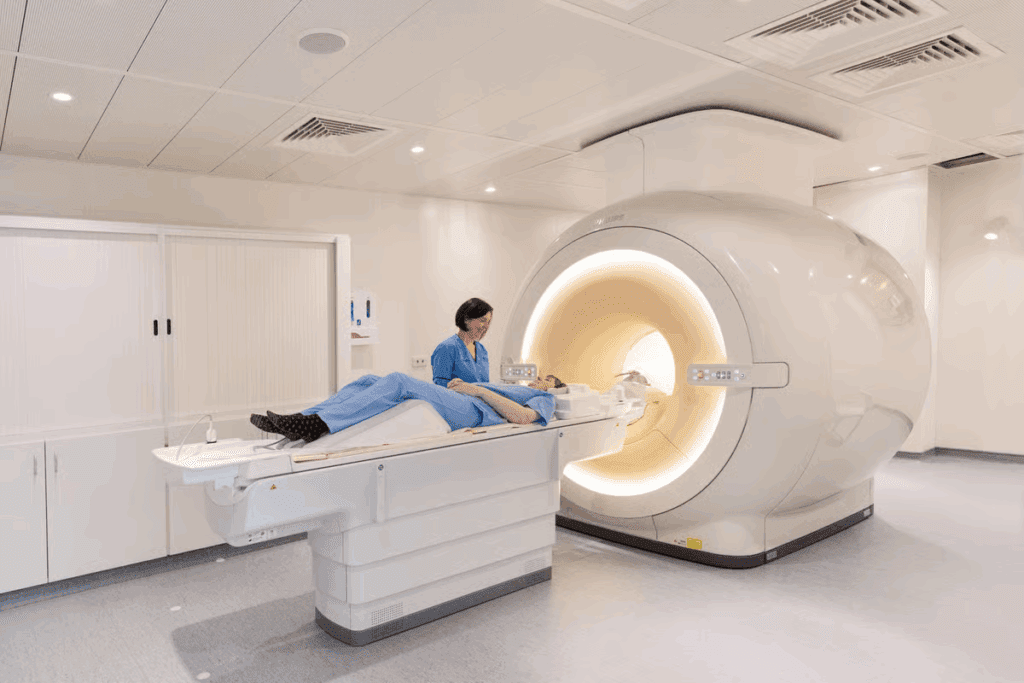
Real-Time MRI Visualization Technique
The In-Bore Direct MRI Guided Prostate Biopsy is done inside the MRI scanner. This real-time visualization helps us find hard-to-spot lesions. It’s a big improvement over other methods.
With the MRI’s clear images, we can precisely guide the biopsy needle. This makes the tissue sampling much more accurate.
Advantages for Difficult-to-Access Lesions
In-Bore Direct MRI Guided Prostate Biopsy is great for hard-to-reach lesions. It can find and biopsy lesions that are tricky to get to. This is a big plus.
This method is super helpful for patients who keep showing signs of cancer after negative biopsies. The precision of In-Bore MRI Guided Biopsy leads to better diagnoses. This means better treatment plans for patients.
Method 3: Transrectal Ultrasound Guided (TRUS) Prostate Biopsy
The TRUS prostate biopsy uses ultrasound to guide the needle into the prostate. It’s a key method for finding prostate cancer. It’s effective and doesn’t hurt much.
Standard TRUS Procedure
For a TRUS biopsy, the patient lies on their side with knees up. Ultrasound imaging shows the prostate gland. This helps the doctor place the needle correctly.
The procedure is done under local anesthesia to keep the patient comfortable.
The steps for a standard TRUS biopsy are:
- Preparation: The patient is ready for the procedure, with local anesthesia.
- Ultrasound Imaging: The doctor uses a probe to see the prostate.
- Biopsy Sampling: The needle is guided to take tissue samples.
Systematic Sampling Protocols
Systematic sampling is key in TRUS biopsy. It makes sure the samples are from all parts of the prostate. Typically, a 12-core biopsy is used, taking samples from different areas.
This method helps find prostate cancer better.
The benefits of TRUS biopsy are:
- It’s widely used and known by urologists.
- Ultrasound guides the needle accurately.
- It’s not invasive, and recovery is quick.
In summary, TRUS prostate biopsy is a key tool for finding prostate cancer. Its systematic approach and ultrasound guidance make it reliable for detecting cancer.
Method 4: Transperineal Prostate Biopsy Approach
Transperineal prostate biopsy is a new way to check for prostate cancer. It goes through the perineum, the space between the scrotum and anus. This method is different from older ways of doing biopsies.
Procedure and Technical Considerations
The biopsy starts with the patient in a special position. This makes it easy to reach the perineum. Next, we use ultrasound to see the prostate gland and pick the right spots for the biopsy.
Technical considerations include using a grid or template. This helps guide the biopsy needle into the prostate. It’s important for getting accurate samples of prostate tissue.
Infection Risk Reduction Benefits
This method might lower the chance of getting an infection compared to other biopsies. It avoids the rectal wall, which cuts down on bacteria getting into the prostate.
Studies have shown that it can greatly reduce infection risks. This makes it safer for patients, even those at higher risk of problems.
In summary, the transperineal prostate biopsy is a good choice for diagnosing prostate cancer. It’s precise and has less risk of infection.
Methods 5-7: Specialized Biopsy Approaches
Specialized biopsy techniques like cognitive fusion, saturation, and focal saturation biopsies offer advanced diagnostic tools. They aim to improve prostate cancer detection accuracy. These methods also provide more focused ways to diagnose.
Cognitive Fusion Biopsy
Cognitive fusion biopsy combines MRI and ultrasound imaging without complex software. It relies on the urologist’s skill to merge MRI images with ultrasound data. This allows for precise targeting of suspicious areas.
This approach is useful because it uses MRI’s strengths to spot cancerous lesions and ultrasound for guiding the biopsy needle. It boosts the accuracy of tissue sampling.
Saturation biopsy takes many tissue samples from the prostate gland. It’s used for patients with high PSA levels or signs of cancer despite negative biopsies.
This technique is good for finding cancer in patients with a high suspicion. Sampling more areas raises the chance of finding cancer if it’s there.
Focal Saturation Biopsy
Focal saturation biopsy is a version of saturation biopsy that focuses on high-risk areas seen on MRI. It aims to balance thorough sampling with minimizing unnecessary tissue sampling.
By focusing on the most suspicious regions, focal saturation biopsy can improve diagnostic results. It may also lower the risk of complications from more extensive sampling.
| Biopsy Method | Description | Key Benefits |
| Cognitive Fusion Biopsy | Mentally fuses MRI and ultrasound images for targeted sampling | Precise targeting without fusion software |
| Saturation Biopsy | Takes a large number of tissue samples from the prostate | Increased cancer detection in high-risk patients |
| Focal Saturation Biopsy | Targets high-risk areas identified on MRI | Balances thoroughness with reduced sampling |
Preparing for Your Prostate Biopsy Procedure
Getting ready for a prostate biopsy is important. We’re here to help you understand what to do. A prostate biopsy is a big deal, and being prepared can make a big difference.
Pre-Procedure Instructions
Before your prostate biopsy, you need to follow some steps. Your healthcare provider will give you detailed guidance on how to get ready. This might include:
- Dietary restrictions or recommendations
- Instructions on whether to stop taking certain medications
- Guidance on bowel preparation
- Information on any necessary tests or examinations before the biopsy
It’s very important to follow these instructions carefully. This will help make the procedure go smoothly.
Medication Considerations
Some medications can affect your prostate biopsy. It’s vital to inform your healthcare provider about all medications you’re currently taking. This includes blood thinners, antibiotics, and any other prescription or over-the-counter drugs. Your healthcare provider will tell you if you should keep taking these medications or stop before the biopsy.
What to Expect During the Procedure
Knowing what happens during a prostate biopsy can help you feel less anxious. You’ll be positioned on your side or back, and the area around your prostate will be cleaned and prepared. The biopsy procedure involves taking tissue samples from your prostate gland, which will then be examined for any abnormalities.
Your healthcare team will watch over you during the procedure. They want to make sure you’re comfortable and safe. The whole process usually takes 30 to 60 minutes, depending on the technique used.
Recovery and Aftercare Following Prostate Biopsy
Recovering from a prostate biopsy needs careful aftercare. This ensures a smooth healing process. We’re here to guide you through the necessary steps.
Managing Common Side Effects
After a prostate biopsy, some men may feel discomfort, bleed, or have trouble urinating. Managing these side effects effectively is key to a comfortable recovery.
- Resting adequately and avoiding strenuous activities
- Using prescribed medications to manage pain or discomfort
- Monitoring for signs of infection, such as fever or increased redness
It’s essential to follow the specific aftercare instructions provided by your healthcare provider, as they are tailored to your individual needs.
When to Seek Medical Attention
While most men recover without major issues, it’s vital to know when to seek medical attention. If you experience severe pain, heavy bleeding, or difficulty urinating, you should contact your healthcare provider immediately.
| Symptom | Action |
| Severe pain or discomfort | Contact your healthcare provider |
| Heavy bleeding or clots | Seek immediate medical attention |
| Difficulty urinating or painful urination | Consult your healthcare provider |
Follow-up Care and Results Interpretation
Follow-up care is a critical part of the prostate biopsy process. Your healthcare provider will schedule a follow-up appointment to discuss the biopsy results and any necessary next steps.
Understanding your biopsy results is vital. Your healthcare provider will explain the findings, whether they indicate cancer, and if so, the stage and grade of the cancer. This information will guide further treatment decisions.
We are committed to supporting you throughout your recovery and aftercare. By following these guidelines and maintaining open communication with your healthcare provider, you can ensure the best possible outcome following your prostate biopsy.
Conclusion
We’ve looked into MRI-guided prostate biopsy methods that have changed how we find prostate cancer. MRI helps doctors get better at finding cancer, leading to better care for patients.
MRI prostate biopsy is a big step forward in fighting prostate cancer. It lets doctors target and take samples from specific areas. This makes it easier to avoid missing cancer and over-treating it.
There are many benefits to these biopsy methods. They help find cancer more accurately and lower the chance of infections. As these methods get better, we’ll see even more effective ways to diagnose and treat prostate cancer.
Understanding MRI prostate biopsy helps us see how important these tools are. They help doctors make better choices for their patients. As we keep improving, we’re excited for the future of prostate cancer diagnosis.
FAQ
What is an MRI prostate biopsy?
An MRI prostate biopsy is a procedure that uses MRI to find and take tissue samples from the prostate gland. It’s a minimally invasive method.
Why is a prostate biopsy necessary?
A prostate biopsy is key to diagnosing prostate cancer. It’s often needed when PSA tests or digital rectal exams show abnormal results.
What is the difference between MRI-ultrasound fusion biopsy and TRUS biopsy?
MRI-ultrasound fusion biopsy uses MRI and ultrasound together to guide the biopsy needle. TRUS biopsy uses ultrasound alone.
What are the benefits of MRI-guided prostate biopsy?
MRI-guided prostate biopsy is more accurate and reduces unnecessary biopsies. It targets specific areas with high precision.
How do I prepare for a prostate biopsy?
To prepare, follow pre-procedure instructions. This includes stopping certain medications and understanding what to expect during the procedure.
What are the common side effects of a prostate biopsy?
Common side effects include discomfort, bleeding, and infection. Managing these is key to a smooth recovery.
How is the transperineal prostate biopsy approach different from TRUS biopsy?
The transperineal approach goes through the perineum, lowering infection risk. TRUS biopsy goes through the rectum.
What is the role of MRI in prostate cancer diagnosis?
MRI enhances biopsy accuracy and improves detection rates. It provides detailed images of the prostate gland.
What are the advantages of in-bore direct MRI guided prostate biopsy?
In-bore direct MRI guided biopsy offers real-time visualization. This allows for precise targeting of difficult-to-access lesions.
How are biopsy results interpreted?
A pathologist interprets biopsy results. They indicate if cancer is present and its grade and extent.
What is the significance of prostate biopsy in prostate cancer management?
Prostate biopsy is vital for diagnosing prostate cancer. Understanding MRI-guided biopsy methods is key for informed decisions.
What are the different types of prostate biopsies?
Types include MRI-ultrasound fusion biopsy, in-bore direct MRI guided biopsy, TRUS biopsy, and transperineal biopsy. There are also specialized approaches like cognitive fusion biopsy and saturation biopsy.
References
- Cool, D. W., Zhang, X., Romagnoli, C., Izawa, J. I., Romano, W. M., & Fenster, A. (2015). Evaluation of MRI-TRUS fusion versus cognitive registration accuracy for MRI-targeted, TRUS-guided prostate biopsy. AJR American Journal of Roentgenology, 204(1), 83-91. https://ajronline.org/doi/10.2214/AJR.21.26154






