Last Updated on October 21, 2025 by mcelik
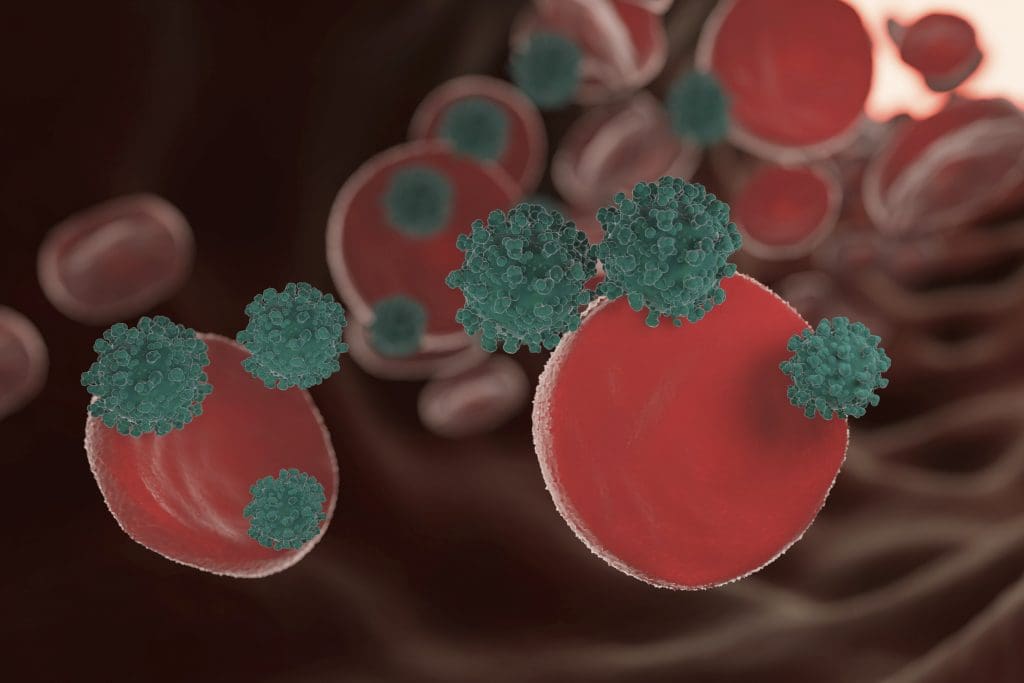
Myelodysplastic syndrome (MDS) is a group of disorders caused by poorly formed or dysfunctional blood cells. It’s a type of blood cancer that can lead to leukemia. The risk of developing MDS goes up with age, mainly in older adults.
Knowing when people usually get MDS is key for early treatment. As more people get older, the number of MDS cases will likely go up. It’s important to spread the word about this condition.
Myelodysplastic syndrome (MDS) is a complex group of disorders. It affects the body’s ability to make blood cells properly. This can lead to various health problems.
MDS is marked by the poor production of blood cells. This is due to ineffective hematopoiesis. The World Health Organization (WHO) has a widely used classification system for MDS.
This system looks at the cell’s shape, genetic changes, and symptoms. It helps sort MDS into different types.
Knowing the exact type of MDS is key. It helps doctors predict how the disease will progress. The International Prognostic Scoring System (IPSS) is a tool used for this purpose.
The biology of MDS involves genetics and environment. Genetic mutations are a big part of it. These mutations disrupt normal blood cell production.
This can lead to bone marrow failure. It also increases the risk of turning into acute myeloid leukemia (AML).
Grasping the molecular basis of MDS is vital. It helps in creating targeted treatments. This can improve patient outcomes.
MDS is different from other blood cancers like AML. The main difference is the number of blasts in the bone marrow and blood. MDS has dysplastic changes, while AML has more than 20% blasts.
Knowing the difference is important. It helps doctors choose the right treatment. It also helps predict how the disease will progress.
To diagnose MDS, doctors look at many factors. They consider clinical, morphological, and genetic features. This ensures accurate diagnosis and management.
The age when people get myelodysplastic syndrome (MDS) is key to understanding this blood disorder. MDS mostly affects older adults. This shows a clear link between age and the chance of getting the disease.
Research shows that the median age of MDS diagnosis is about 70 years. This means MDS is mostly a disease of the elderly. The risk of getting MDS grows a lot after 60.
The rates of MDS vary a lot with age. It’s rare in people under 40, but it gets much more common with age. Here’s what studies have found:
| Age Group | Incidence Rate (per 100,000) |
| 20-39 | 0.5-1.0 |
| 40-59 | 2-5 |
| 60-69 | 10-20 |
| 70+ | 30-50 |
This table shows how MDS cases jump up with age. It shows how important age is as a risk factor.
Looking at statistical trends and patterns in MDS can help us understand it better. The data shows more MDS cases in older adults. This is because more people are getting older and because doctors can diagnose it better now.
Knowing these trends is key for planning healthcare and resources. As the world’s population gets older, MDS cases will likely go up. This means we need to make doctors and hospitals better at spotting and treating it.
Myelodysplastic syndrome (MDS) mainly hits older adults. This is due to several aging-related factors. As we get older, our bodies undergo changes that raise the risk of MDS.
Cellular aging causes cells to wear out over time. This makes them more prone to DNA damage. Such damage can cause mutations, leading to MDS.
As we age, our cells gather more DNA damage. This damage comes from the environment and mistakes in DNA copying.
Older adults face more time with risk factors for MDS. These include chemicals, radiation, and past chemotherapy. All these add up, raising the risk of MDS.
The age-related decline in bone marrow function is another key factor. As we age, our bone marrow makes fewer healthy blood cells. This decline can lead to MDS, as the bone marrow struggles to function.
The mix of cellular aging, exposure to risk factors, and bone marrow decline makes older adults more at risk for MDS. Knowing these factors helps in finding ways to prevent and treat MDS.
Older adults, aged 65 and above, face a higher risk of myelodysplastic syndrome (MDS). This condition is caused by blood cells that don’t form right or work well.
They are more at risk because of aging cells, past exposures, and a decline in bone marrow function with age.
MDS is more common in older adults. Studies show the risk goes up with age.
Older adults with MDS often face a higher chance of the disease getting worse. It can turn into acute myeloid leukemia (AML).
It’s key to understand these traits to create effective treatment plans for older adults.
Elderly patients with MDS need special care. They often have other health issues like heart disease, diabetes, and chronic conditions. These can make treatment harder.
A detailed geriatric assessment is needed. It helps decide the best treatment, considering the patient’s health and ability to function.
Comorbidities in older adults with MDS make treatment tough.
They need a care plan that fits their health, avoiding complications and focusing on supportive care.
Managing MDS in older adults requires a team effort. Hematologists, geriatricians, and other experts work together to meet their complex needs.
Myelodysplastic syndrome (MDS) affects not just older adults but also those in their 40s to 65. It’s a condition where the bone marrow can’t make healthy blood cells. This leads to various health problems.
MDS is less common in middle-aged people than in the elderly. Yet, it’s a significant concern for those between 40 and 65. As people get older in this age group, the risk of getting MDS goes up.
Key statistics on MDS incidence in middle-aged adults include:
The outlook for middle-aged adults with MDS is often better than for the elderly. Younger patients usually have better health and fewer other health issues. This can help them respond better to treatment.
Prognostic factors for MDS in middle-aged adults include:
MDS in middle-aged adults can greatly affect their work and lifestyle. The condition and its treatment can cause fatigue and increase the risk of infections. These issues can make it hard to work and do daily activities.
Some of the lifestyle impacts include:
Understanding these aspects is key to managing MDS well in middle-aged adults. It helps improve their quality of life.
Myelodysplastic syndrome (MDS) is rare in kids and young adults. It’s often caused by genetics. We need to understand the causes and how they differ from older adults.
Pediatric MDS is different from adult MDS. Kids often have more aggressive disease. They need quick and effective treatments.
Research shows early diagnosis and tailored treatments are key. Genetic mutations play a big role in MDS in kids. This affects treatment and outlook.
Genetics are key in MDS in young people. Certain mutations can lead to MDS. These are often part of inherited syndromes.
Finding these genetic factors is important. It helps us understand and treat MDS better. Genetic sequencing has made finding these mutations easier.
Inherited bone marrow failure syndromes (IBMFS) affect blood cell production. Conditions like Fanconi anemia and Dyskeratosis congenita increase MDS risk.
It’s important to understand the link between IBMFS and MDS. Regular checks and early action can improve outcomes for those at risk.
| Condition | Characteristics | Risk of MDS |
| Fanconi Anemia | Congenital aplastic anemia, physical anomalies | High |
| Dyskeratosis Congenita | Nail dystrophy, oral leukoplakia, reticulated skin hyperpigmentation | Moderate to High |
| Shwachman-Diamond Syndrome | Exocrine pancreatic insufficiency, skeletal abnormalities | Moderate |
The table shows some inherited syndromes and their MDS risk. Knowing these risks helps manage affected individuals.
Knowing the risk factors for myelodysplastic syndrome is key to catching it early. Many things can lead to MDS, like age, environmental exposures, past cancer treatments, and genetics.
Age is a big risk factor for MDS, with most cases found in people over 65. The risk goes up with age, hinting at bone marrow changes.
Key age-related factors include genetic mutations and bone marrow decline with age.
Some environmental and job hazards raise MDS risk. These include:
People in jobs with these exposures should get checked often.
Having had cancer treatments, like chemotherapy and radiation, ups MDS risk. This is called therapy-related MDS (t-MDS).
Those treated with alkylating agents and those who got radiation therapy are at higher risk.
Genetics also matter in MDS. Certain genetic syndromes, like Fanconi anemia and Dyskeratosis congenita, raise the risk.
Genetic testing can spot these risks early, helping to act fast.
It’s important to know the early signs of MDS to get help quickly. Myelodysplastic syndrome (MDS) shows different symptoms in different people.
The first signs of MDS include feeling very tired, getting sick often, and bleeding easily. Fatigue happens because the bone marrow can’t make enough healthy red blood cells. Not having enough white blood cells leads to infections, and low platelet counts cause bleeding problems.
“The symptoms of MDS can be quite non-specific, making it essential to be aware of any persistent or unusual changes in your body,” says a hematologist specializing in MDS.
People of different ages show MDS symptoms in different ways. Older adults often feel very tired and get sick more easily because their immune system weakens with age. Younger people might have MDS because of their genes, which can change how they feel.
If you have symptoms that last a long time or are very bad, you should see a doctor. Getting diagnosed and treated early can really help.
“Prompt evaluation is key. If you’re experiencing symptoms like persistent fatigue, frequent infections, or unusual bleeding, don’t hesitate to consult a healthcare professional,” advises an expert in hematology.
Knowing about MDS symptoms is the first step to managing it well. By recognizing early signs and how they change with age, patients can get the help they need sooner.
Diagnosing myelodysplastic syndrome (MDS) requires various tests and procedures. These tests are more challenging for elderly patients. The diagnostic process must consider the patient’s age and health. It must also account for MDS’s unique characteristics at different life stages.
The diagnosis of MDS involves several steps:
Elderly patients face unique challenges in diagnosing MDS. For example:
The way MDS is diagnosed changes with age. It’s important to understand the patient’s age and health. For instance:
Knowing these differences helps doctors develop better diagnostic plans for MDS at all ages.
Understanding MDS progression is key to managing the disease well. MDS makes it hard for the bone marrow to create healthy blood cells. This leads to various problems.
MDS goes through several stages, from diagnosis to more serious forms. The timeline varies, with some patients seeing slow progress and others facing quick decline.
Early-stage MDS might not show many symptoms. But as it gets worse, patients may feel more tired, get infections, and bleed more. This is because the bone marrow can’t make enough healthy blood cells.
Age is a big factor in MDS progression. Older people are more likely to get MDS and have it progress faster. This is because they’ve been exposed to more risks over time and their bone marrow function declines with age.
It’s important to understand how age affects MDS. This helps in creating treatments that fit the needs of people of different ages.
One big worry with MDS is turning into Acute Myeloid Leukemia (AML). AML is much more serious and can be deadly. The chance of turning into AML depends on the type of MDS, genetic changes, and other health issues.
It’s vital to watch patients closely for signs of MDS getting worse or turning into AML. This way, we can act fast and help them live longer.
Effective treatment for MDS combines standard protocols, age-adapted strategies, and supportive care. The aim is to manage symptoms, improve quality of life, and possibly slow disease progression.
Standard treatments for MDS depend on the patient’s risk category, health, and disease specifics. These treatments include:
Treatment strategies for MDS vary with age. Older patients often need more conservative treatments due to comorbidities and lower tolerance to aggressive therapies. Younger patients might be eligible for more intensive treatments, like stem cell transplantation.
| Age Group | Common Treatment Approaches |
| Younger Adults | Intensive chemotherapy, stem cell transplantation |
| Older Adults | Supportive care, hypomethylating agents, lenalidomide |
Supportive care is key in managing MDS, focusing on symptom relief and improving quality of life. This includes:
By customizing treatments to meet individual MDS patient needs, healthcare providers can enhance outcomes and quality of life.
For MDS patients, stem cell transplantation is a possible cure. But, its success depends a lot on the patient’s age. This treatment replaces damaged bone marrow with healthy stem cells. It’s a complex process.
Age is key in deciding if someone can get a stem cell transplant. Younger patients are often better candidates because they have fewer health problems. But, advanced age alone is not a complete no-go for transplantation.
When deciding on a transplant for older adults, doctors look at their overall health. They check for other health issues and how well the patient can handle the treatment.
To help older patients get stem cell transplants, doctors use reduced-intensity conditioning (RIC). RIC cuts down the harm from traditional conditioning. This makes it easier for older adults to handle.
RIC works by using the immune system to fight MDS. It doesn’t need as strong conditioning to get rid of cancer cells. This gives older MDS patients a chance at a cure.
Stem cell transplant results vary by age. Younger patients usually do better because they have fewer health issues. But, older patients can also get good results with the right care and RIC.
Research shows that with the right choice of patients and treatment, older patients can do as well as younger ones. But, they face higher risks of problems.
Learning how to live with myelodysplastic syndrome (MDS) is key for patients to keep a good quality of life. MDS affects not just the body but also a person’s overall happiness.
People with MDS often struggle with tiredness, infections, and bleeding. These issues can make everyday tasks hard. It’s important to find ways to manage these symptoms to improve quality of life.
Having a good treatment plan and making lifestyle changes can help a lot. Regular doctor visits, eating right, and staying active are important for staying healthy.
The effects of MDS differ by age. Older adults might face more problems because of other health issues and aging.
| Age Group | Common Challenges | Considerations |
| Younger Adults | Maintaining employment, family responsibilities | Balancing treatment with lifestyle demands |
| Older Adults | Comorbid conditions, physical decline | Managing multiple health issues, supportive care |
It’s important for MDS patients to find ways to cope. This includes getting support from loved ones and joining support groups. Also, trying stress-reducing activities like meditation or yoga can help.
Knowing about MDS, its treatments, and how to handle symptoms can help patients feel more in control. This can lead to a better overall well-being.
Age is a key factor in how well MDS patients do. Knowing how age affects prognosis helps patients and doctors make better choices about treatment.
Age greatly changes the outlook for MDS patients. Older people usually face a tougher time than younger ones. This is because of health issues, overall well-being, and the disease itself.
Age-related factors that affect MDS prognosis include:
Prognostic scoring systems are important for predicting MDS outcomes. They look at age and other factors to guide treatment.
The Revised International Prognostic Scoring System (IPSS-R) is widely used. It considers:
| Prognostic Factor | Description | Impact on Prognosis |
| Cytogenetic Abnormalities | Genetic changes in bone marrow cells | Poor prognosis with complex abnormalities |
| Bone Marrow Blast Percentage | Percentage of immature cells in bone marrow | Higher percentage indicates poorer prognosis |
| Severity of Cytopenias | Low blood cell counts | More severe cytopenias indicate poorer prognosis |
| Age | Patient’s age at diagnosis | Older age associated with poorer prognosis |
Life expectancy for MDS patients depends on age, disease characteristics, and health. Prognostic scoring systems help estimate life expectancy and guide treatment planning.
For example, a younger patient with fewer health issues may live longer than an older patient with more problems.
Understanding the impact of age on MDS prognosis and survival rates is key to improving treatment plans and patient outcomes.
Myelodysplastic syndrome (MDS) research is moving forward fast. New therapies and precision medicine are leading to better patient results. These advances are making it easier to manage MDS.
Several new treatments are being explored for MDS, including:
Age-targeted therapies are being developed for MDS patients of all ages. For older adults, treatments with fewer side effects are being focused on.
Precision medicine is changing MDS treatment. It tailors therapies to each patient’s genetic makeup and disease specifics.
The mix of precision medicine and age-targeted therapies is expected to greatly improve MDS patient outcomes. Key points include:
As research keeps moving forward, the future of MDS treatment looks bright. It aims to enhance quality of life and survival rates for all ages.
Myelodysplastic syndrome (MDS) is a complex condition that affects people of all ages. But it’s more common in older adults. Knowing how age affects MDS is key to better management and care.
We’ve looked at MDS from different angles in this article. This includes what it is, how it’s classified, and the science behind it. We’ve also talked about how age changes how MDS is seen, diagnosed, and treated. We’ve highlighted the challenges faced by people of different ages with MDS.
As we wrap up this summary on MDS, it’s clear that being aware, getting an early diagnosis, and the right treatment are vital. Understanding how age impacts MDS helps healthcare teams create better care plans. This leads to better outcomes and a better quality of life for patients.
Myelodysplastic syndrome (MDS) is a group of disorders. They are caused by poorly formed or dysfunctional blood cells. These disorders mainly affect older adults.
People usually get diagnosed with MDS in their 70s or 75s. Most cases happen in those over 65.
Yes, though rare, MDS can happen in younger adults and children. It’s often linked to genetic factors or inherited bone marrow failure syndromes.
Risk factors include age, environmental and occupational exposures, and cancer treatments. Genetic predispositions also play a role.
MDS can progress at different rates. Some people may see slow progression, while others may quickly move to AML, a more aggressive blood cancer.
Symptoms include fatigue, infections, and bleeding disorders. These symptoms can vary in severity and presentation across different age groups.
Diagnosis involves blood tests, bone marrow biopsies, and other procedures. Elderly patients face challenges like comorbidities and age-related changes.
Treatments include standard protocols and age-adapted strategies. Supportive care is also important. Considerations for stem cell transplantation and age factors are taken into account.
MDS is not curable with conventional treatments. But, stem cell transplantation offers a chance for cure. Outcomes vary by age and other factors.
MDS can greatly impact quality of life. Age-specific challenges include managing comorbidities, coping with treatment side effects, and maintaining independence.
Recent advances include new treatments and age-targeted therapies. Precision medicine approaches offer hope for better outcomes for MDS patients.
Age is a big factor in determining prognosis and survival rates. Older patients generally have poorer outcomes due to comorbidities and age-related decline.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!