Last Updated on November 17, 2025 by Ugurkan Demir
For those with multiple myeloma, a stem cell transplant is a key treatment. It can be a big help. But, it’s hard to understand all about it.
At Liv Hospital, we focus on you. We use the latest science to help you. Our team wants you to know all your options.
A stem cell transplant is often suggested for myeloma patients. It’s best for those who are young and healthy. The American Cancer Society says it can really help you live longer and stay in remission longer.

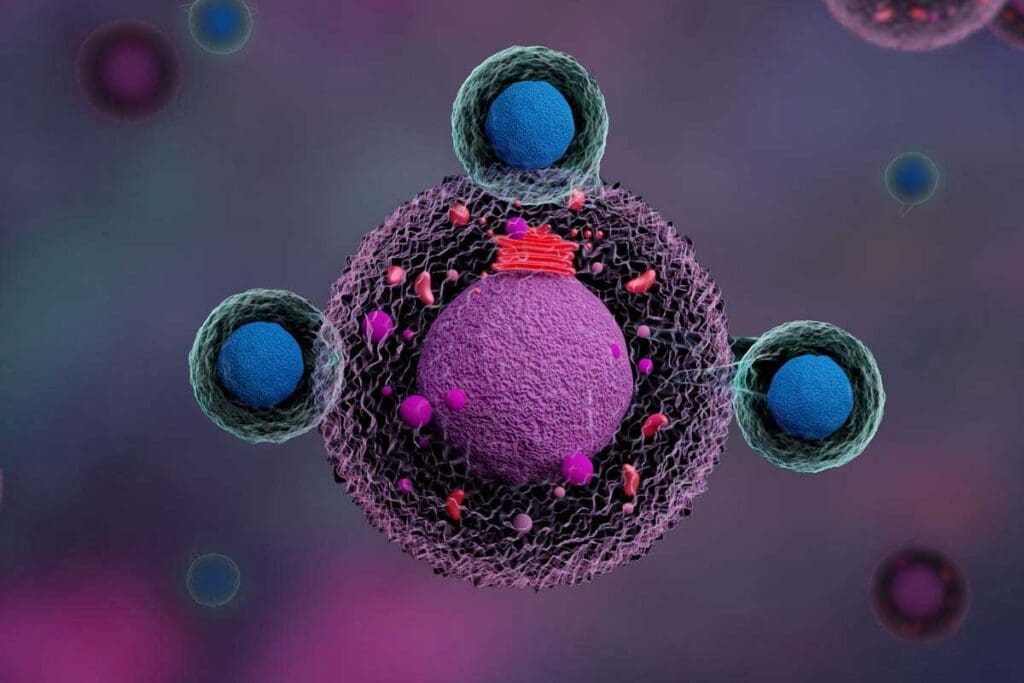
Multiple myeloma is a complex cancer that affects plasma cells in the bone marrow. It needs a detailed treatment plan. We will look into the disease, its treatments, and the key role of stem cell transplantation.
Multiple myeloma happens when plasma cells in the bone marrow turn bad and grow too much. They make bad proteins. This messes up the bone marrow, causing bone damage and anemia.
We don’t know what causes multiple myeloma. But, age, family history, and some chemicals can increase the risk. Knowing these helps in diagnosing and treating the disease.
Treatment for multiple myeloma includes several therapies to control the disease and ease symptoms. The main treatments are:
These treatments are often used together for the best results.
Stem cell transplantation, like autologous stem cell transplantation, is key in treating multiple myeloma. It uses high-dose chemotherapy and then gives back the patient’s stem cells. This helps the bone marrow work again.
Stem cell transplantation can lead to better survival rates and longer remission. But, whether to have it depends on the patient’s health and disease stage.
| Treatment Approach | Description | Benefits |
| Targeted Therapy | Targets specific cancer cells | Reduces harm to healthy cells |
| Chemotherapy | Kills cancer cells | Effective in reducing tumor size |
| Stem Cell Transplantation | Replaces damaged bone marrow | Improves survival rates and remission |

Stem cell transplantation has changed how we treat multiple myeloma. It’s now a key part of treatment for many patients. This approach helps improve their health and life quality.
During a stem cell transplant, patients get strong chemotherapy to kill cancer cells in their bone marrow. Then, they get healthy stem cells back. These can be their own or from a donor.
These stem cells help make new, healthy blood cells. This is how the bone marrow gets fixed.
Studies show stem cell transplants can greatly improve survival and remission rates for myeloma patients. The American Cancer Society notes that this treatment has greatly helped patient outcomes. It helps patients live longer without their disease getting worse, improving their quality.
Not every myeloma patient can get a stem cell transplant. Doctors look at age, health, and other conditions to decide. A team of myeloma experts must check if a patient is a good candidate. Usually, those under 65 with few health issues are best suited.
Knowing about stem cell transplants helps patients and their families make better choices. It lets them understand their treatment options better. This knowledge helps them feel more in control of their care.
The way we collect stem cells for myeloma treatment has changed a lot. At first, we took stem cells straight from the bone marrow. This was called bone marrow transplantation (BMT). But now, we use a newer, better method.
At the start, bone marrow transplants were the go-to for myeloma patients. We took stem cells from the bone marrow, usually from the hip bones, while the patient was asleep. It worked, but it had some downsides, like needing to stay in the hospital and being a more complex procedure.
Later, we started taking stem cells from the blood, called peripheral blood stem cell transplant (PBSCT). This change was because PBSCT is easier and faster. We use special drugs to move the stem cells from the bone marrow into the blood, making them easier to get.
The new way of getting stem cells has many key benefits. It’s less invasive than the old way, which means fewer risks and quicker healing. Also, PBSCT leads to faster recovery and less chance of myeloma cells getting in the way, as the American Cancer Society points out.
Also, using blood stem cells is now the top choice for autologous stem cell transplants in myeloma patients. This change has led to better results and a better life for patients while they recover.
In short, moving from bone marrow transplants to blood stem cell transplants is a big step forward in treating myeloma. As technology keeps getting better, we’ll see even more progress in how we do stem cell transplants, helping more patients.
The process of harvesting stem cells for myeloma treatment involves several stages. Each stage is key to the success of the stem cell transplant.
Before stem cells can be harvested, patients go through induction therapy. This therapy aims to lower the number of myeloma cells. It includes chemotherapy, targeted therapy, and corticosteroids.
The goal is to get the patient into remission or reduce myeloma cells significantly. This makes it safer to collect stem cells.
After induction therapy, the next step is to mobilize stem cells. This means getting them from the bone marrow into the bloodstream. Growth factors, like G-CSF, are used to do this.
In some cases, chemotherapy is also used. This is if the patient has a lot of myeloma cells in their bone marrow.
After mobilization, stem cells are collected through apheresis. This is a process where the patient’s blood is drawn into a machine. The machine separates the stem cells from other blood components.
The stem cells are then collected and stored. The remaining blood components are returned to the patient. This process can take hours and may need to be done over several days.
Once collected, the stem cells are frozen and stored for later use. This is done through cryopreservation, where the stem cells are cooled to very low temperatures. This keeps them viable.
The frozen stem cells are stored in a secure facility. They are kept there until needed for the stem cell transplant.
The stem cell harvesting process is complex but vital for myeloma treatment. Understanding these steps helps patients prepare for this important part of their treatment.
When it comes to treating multiple myeloma with stem cell transplantation, knowing the difference between autologous and allogeneic is key. Autologous stem cell transplant uses the patient’s own stem cells. This is the most common method for treating multiple myeloma. The process starts with removing the patient’s stem cells, followed by high-dose chemotherapy. Then, the stem cells are given back to rebuild the bone marrow.
Autologous transplantation uses the patient’s own stem cells. This is the most common type of stem cell transplant for multiple myeloma. The process includes harvesting the patient’s stem cells, followed by high-dose chemotherapy, and then reinfusing the stem cells to help restore the bone marrow’s function.
Benefits of Autologous Transplantation:
Allogeneic transplantation uses stem cells from a donor. This type is less common for multiple myeloma. It’s usually considered in specific situations, like in clinical trials or for patients with certain high-risk features.
Risks Associated with Allogeneic Transplantation:
The choice between autologous and allogeneic transplantation depends on several factors. These include the patient’s overall health, the stage of multiple myeloma, and the availability of a suitable donor.
| Transplant Type | Advantages | Risks |
| Autologous | Lower GVHD risk, faster recovery | Potential for reinfusing malignant cells |
| Allogeneic | Potential graft-versus-myeloma effect | Higher GVHD risk, higher infection risk |
We know that choosing between these two transplant types can be tough. Our team is here to provide personalized care and guidance. We help patients make informed decisions about their treatment.
Myeloma treatment includes a key step: high-dose chemotherapy followed by stem cell reinfusion. This method aims to get rid of myeloma cells.
The main aim of high-dose chemotherapy in a stem cell transplant is to kill myeloma cells. High-dose chemotherapy uses drugs like melphalan, which target myeloma cells well.
The conditioning regimen is the high-dose chemotherapy given before stem cell reinfusion. It’s vital for getting the body ready to accept the stem cells. It kills existing myeloma cells and makes room for new ones.
After the high-dose chemotherapy, the stored stem cells are put back into the patient’s blood through a vein. This is like a blood transfusion. The stem cells then go to the bone marrow to make new blood cells.
After reinfusion, the stem cells start making blood cells again. This includes red blood cells, white blood cells, and platelets. Recovery of blood cell production is a key time. The patient is watched closely for any signs of infection or other issues.
It’s key to know and handle the side effects of stem cell transplants to better patient results. This treatment is a big hope for myeloma patients, aiming for remission and longer life. But, it’s important to be ready for the side effects and problems that can happen during and after treatment.
The early side effects of a stem cell transplant are like those from chemotherapy but can be worse. Low blood counts are a big risk, leading to serious infections and bleeding. “Patients often feel tired, nauseous, and lose their hair,” the American Cancer Society says. It’s critical to manage these side effects well for the patient’s comfort and healing.
After a stem cell transplant, infections are a big worry because the immune system is weakened. We use antibiotics and isolation to lower this risk. “The risk of infection is highest when the neutrophil count is low,” showing the importance of careful watching and prevention.
Stem cell transplantation is a good treatment for myeloma, but it can have long-term side effects. These include secondary cancers, organ damage, and hormonal issues. It’s vital to have long-term care to watch for these problems and handle them well.
Medical tech and care practices are getting better, making stem cell transplants safer and more effective. We aim to lead in these advancements, using the newest safety steps to protect our patients and help them recover better. This includes custom care plans, better infection control, and full support services.
By knowing the side effects and complications of stem cell transplants and tackling them early, we can greatly improve treatment results for myeloma patients.
Outpatient stem cell transplantation is changing how we treat multiple myeloma. It’s becoming more common and offers many benefits over traditional inpatient methods.
The idea of outpatient stem cell transplantation has grown a lot. New medical tech and treatment plans let many patients get transplants without long hospital stays.
Now, treatments are more efficient and safe. This is thanks to better ways to collect stem cells, prepare patients, and care for them after the transplant.
Outpatient stem cell transplants have big advantages. One key benefit is lower risk of getting infections in the hospital. This makes recovery safer and more comfortable.
They also mean shorter hospital stays and lower costs. This helps patients and their families financially.
Other benefits include:
Not every myeloma patient can have an outpatient stem cell transplant. We carefully check if a patient is right for it. We look at their health, disease status, and support system.
We check if the patient can follow treatment, is physically able, and has the right care at home. These are key factors for choosing the right patients.
Home care is vital for patients getting outpatient stem cell transplants. They and their caregivers need to be ready for any side effects or problems.
We focus on teaching patients and their caregivers a lot. We teach them about managing medicines, preventing infections, and knowing when to seek urgent medical help.
By choosing the right patients and giving them good support, we make outpatient stem cell transplants a safe and effective option for many myeloma patients.
The journey doesn’t end with a stem cell transplant. For myeloma patients, it’s just the start of a new chapter. Understanding the recovery process, follow-up care, and maintenance therapy is key. It helps improve outcomes and quality of life.
The recovery time after a stem cell transplant varies among myeloma patients. It usually takes several months for the body to recover from the conditioning regimen. Blood counts need to return to normal during this time.
Patients may feel tired, get infections, and face other side effects. We closely watch and manage these issues.
We suggest a structured recovery plan for each patient. This includes rest, nutrition, and gradual return to normal activities. The plan is tailored to the individual’s needs and health status.
Follow-up care is vital after a transplant. We schedule regular appointments to check the patient’s condition. We look for signs of relapse and manage long-term side effects.
Our team works with the patient’s local healthcare provider for seamless care. We educate patients on the importance of adhering to their follow-up schedule. We also teach them to recognize warning signs that may need immediate medical attention.
Maintenance therapy is important after a stem cell transplant. It aims to keep the disease in remission and prevent relapse. Options include lenalidomide, bortezomib, or other targeted therapies, chosen based on the patient’s disease and health.
We discuss the benefits and side effects of each option with our patients. This ensures they are informed and involved in the decision-making process. The choice of therapy is personalized, based on the latest research and guidelines.
Improving and maintaining quality of life is a key focus after a transplant. We address physical, emotional, and social needs. We provide support and resources to help patients navigate the challenges of recovery and reintegrate into their daily lives.
Our team is dedicated to helping myeloma patients achieve the best outcomes and quality of life. By understanding the recovery timeline, following up, considering maintenance therapy, and focusing on well-being, patients can look forward to a brighter future.
Stem cell transplantation has changed how we treat multiple myeloma. It has led to better survival and remission rates for those who can get it. We’ve looked at how this treatment works, from collecting stem cells to dealing with side effects.
We’ve talked about the importance of knowing the different types of stem cell transplants. This includes autologous and allogeneic transplants, and the use of high-dose chemotherapy. We’ve also seen how outpatient stem cell transplantation is making treatment easier for patients.
Stem cell transplant is a key part of myeloma care. By sharing the 7 essential facts about it, we show its value in treating multiple myeloma. As research keeps moving forward, we hope to see even better care for those getting stem cell transplants.
Multiple myeloma is a blood cancer where bad plasma cells grow in the bone marrow. Doctors use chemotherapy, targeted therapy, and stem cell transplants to treat it. Stem cell transplant is key and has made treatment more effective.
Stem cell transplant is vital in treating multiple myeloma. It lets doctors give high-dose chemotherapy. Then, healthy stem cells are given back to the patient to fix the bone marrow.
First, healthy stem cells are taken from the patient. Then, the patient gets high-dose chemotherapy to kill cancer cells. After that, the stem cells are given back to the patient to make new blood cells.
Using peripheral blood stem cells has many benefits. Patients recover faster and have less chance of cancer cells coming back compared to bone marrow transplants.
The process starts with induction therapy to lower the tumor size. Then, mobilization techniques are used to get stem cells into the blood. These cells are collected through apheresis and kept for later use.
Autologous transplant uses the patient’s own stem cells. An allogeneic transplant uses stem cells from another person. Myeloma patients usually get autologous transplants to avoid graft-versus-host disease.
High-dose chemotherapy kills cancer cells in the bone marrow. Then, the patient’s stem cells are given back to help the bone marrow make healthy blood cells again.
Side effects include tiredness, nausea, and more infections. Complications can be short-term, like mouth sores, or long-term, like organ damage. New safety steps have made managing these risks better.
Yes, some patients can get stem cell transplants without staying in the hospital. This needs careful planning and the right patient selection.
Patients will see their blood counts and health get better over time. It’s important to follow up and get ongoing care to keep the disease under control.
A stem cell transplant can greatly improve a myeloma patient’s life by controlling the disease. But, it’s important to think about the side effects and plan for care after the transplant.
Maintenance therapy helps prevent myeloma from coming back after the transplant. It uses less intense treatments than the initial therapy.
Yes, long-term effects include fertility issues, a higher risk of other cancers, and organ damage. Patients should talk to their doctors about these risks and how to manage them.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!