Last Updated on November 24, 2025 by
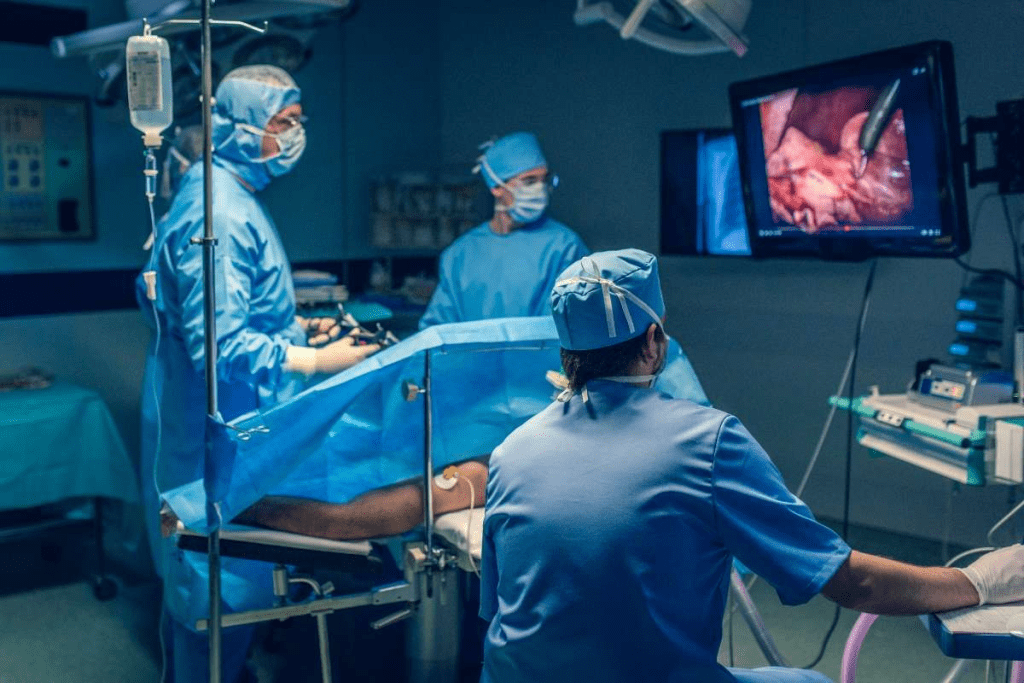
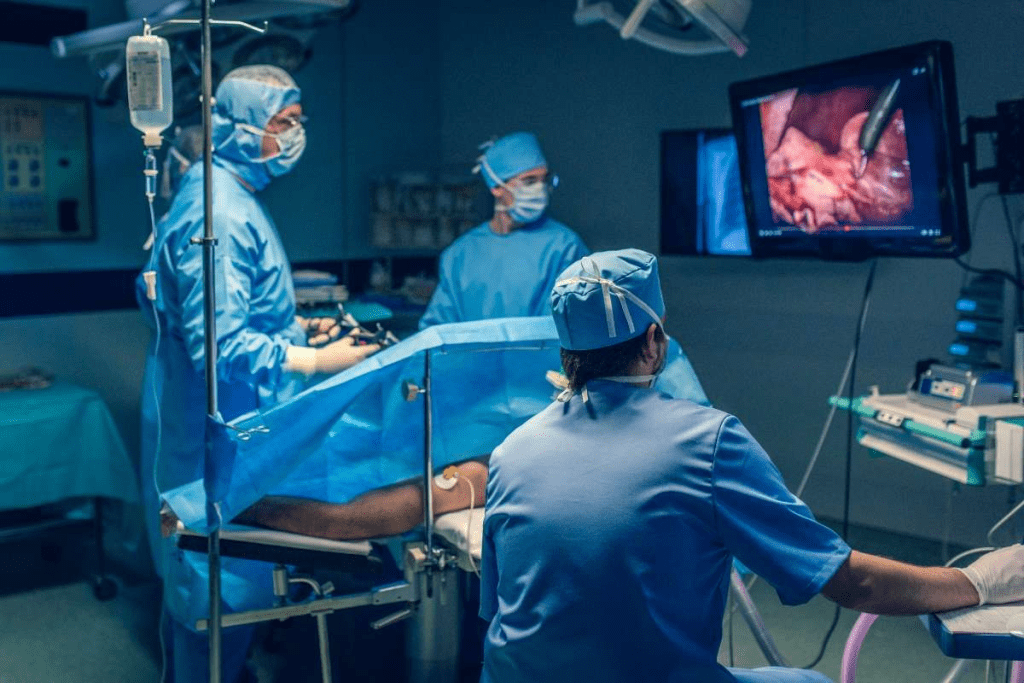
Bladder reconstruction is a complex surgery needed after severe bladder damage, birth defects, or bladder removal for cancer. At Liv Hospital, we use the latest techniques to help thousands of patients every year. This helps them live better lives.
Bladder reconstruction creates a new bladder or a system for urine flow. This lets patients use the bathroom like normal again. We know this big change can be tough. Our team is here to support and guide you every step of the way.
Bladder reconstruction is a complex surgery. It’s a key option for those who need their bladder removed or fixed. This surgery aims to improve life quality for those with severe bladder problems.
Bladder reconstruction rebuilds or replaces the bladder, often with intestinal parts. It’s a life-changing surgery for those with bladder cancer, birth defects, or severe damage. The goal is to make a neobladder or find a way to manage urine.
The term “neo-medical term” means new or rebuilt organs, like a new bladder. The surgery requires careful decisions and techniques, like neobladder creation and urinary diversion. The choice depends on the patient’s health and what they prefer.
The main reasons for bladder reconstruction are:
Each reason needs a different approach to bladder reconstruction. For example, bladder cancer patients might get a neobladder or an ileal conduit for urine diversion. The choice depends on the patient’s health and the extent of the problem.
It’s important for patients and their families to understand bladder reconstruction. Knowing the reasons and techniques helps them make informed decisions. It prepares them for the surgery’s challenges and benefits.
Bladder cancer is a major reason for neobladder surgery, with over 83,000 new cases in the U.S. each year. This shows how common bladder cancer is and its big impact on the need for bladder surgery.

Bladder cancer is among the top ten most common cancers in the U.S. Over 83,000 people are diagnosed with it every year. It affects not just the patients but also their families and the healthcare system.
Men are more likely to get bladder cancer than women, and it’s more common in older adults. Knowing this helps with prevention and treatment planning.
For many with muscle-invasive bladder cancer, radical cystectomy is the best treatment. This surgery removes the bladder and nearby tissues. It’s a complex operation that needs careful planning.
After a radical cystectomy, creating a new bladder is a big step in treating bladder cancer. It aims to remove the cancer and improve the patient’s quality of life. With the right medical team, patients can face this challenge.
Choosing bladder reconstruction after cancer diagnosis is a big decision. Patients must think about their cancer stage, health, and personal wishes. Getting advice from healthcare professionals is key.
A team of urologists, oncologists, and others helps make this decision. They work together to create a treatment plan that fits the patient’s needs. This team approach ensures patients get the best care.
People born with or developing neurological conditions that affect the bladder may find surgery a game-changer. These conditions can make it hard for the bladder to work properly, leading to the need for medical help to fix it.
Certain birth defects, like bladder exstrophy and spina bifida, can really mess with bladder development and function. These issues often need surgery early in life to fix or manage them.
For example, bladder exstrophy is a rare birth defect where the bladder is outside the belly. Surgery is needed to cover the bladder and fix any genital problems.
Neurogenic bladder is when someone has trouble controlling their bladder because of a brain, spinal cord, or nerve issue. This can happen due to spinal cord injuries, multiple sclerosis, or Parkinson’s disease.
Dealing with a neurogenic bladder might include medicine, lifestyle changes, and sometimes surgery. This could be urinary tract diversion or bladder reconstruction to help the bladder work better and avoid problems.
It’s very important to start treating congenital and neurological conditions that affect the bladder early. Early surgical intervention can greatly improve how well someone with these conditions does.
By using a complete and early treatment plan, we can make life better for people with these bladder issues.
When trauma leads to severe bladder damage, surgery is often needed. This surgery is called reconstruction. We will look at how trauma or severe damage can lead to the need for bladder reconstruction.
Severe bladder damage can happen from many injuries. These include:
The type of injury decides if the surgery is urgent or planned.
It’s important for surgeons and patients to understand these differences.
A thorough assessment is key to finding the right treatment for severe bladder damage. This includes:
By carefully looking at the situation and planning, doctors can help patients get the best results from bladder reconstruction.
Bladder reconstruction uses different neobladders and urinary diversion methods. Each has its own benefits. The choice depends on the patient’s health, the reason for the surgery, and the surgeon’s skills.
The ileal conduit is a top choice for urinary diversion. It makes a tube from the intestine to drain urine into a bag outside the body.
Key benefits of the ileal conduit include:
Continent urinary reservoirs use intestinal tissue to make a pouch for urine. Patients can use a catheter to empty it, avoiding an external bag.
Advantages of continent urinary reservoirs include:
Orthotopic neobladder reconstruction makes a new bladder from intestine and connects it to the urethra. This allows for more natural urination.
Benefits of orthotopic neobladder reconstruction include:
Living without a natural bladder needs big changes, but with the right help, people can live well. After surgery, they must get used to a new way of going to the bathroom. This could be through a neobladder or urinary diversion.
Getting used to a neobladder or urinary diversion means understanding new ways of urinating. People need to know how their new system works and how it’s different from the old one. A neobladder is made from intestine and connects to the urethra for more natural urination. Urinary diversion, on the other hand, sends urine out of the body through a stoma.
To manage their condition well, patients should follow their healthcare team’s advice. For those with a neobladder, this might include:
For those with urinary diversion, taking care of the stoma is key. This means:
Every day, managing and caring for oneself is important when living with a neobladder or urinary diversion. Patients need to be proactive to avoid problems and keep their quality of life good. This includes eating well, staying hydrated, and exercising regularly.
Adjusting mentally to life without a natural bladder can be tough. People might feel anxious, depressed, relieved, or grateful. It’s important for them to have support, like counseling, support groups, and online forums.
Support groups are great for sharing experiences and learning from others. Online resources also offer helpful information and emotional support.
With medical advice and emotional support, patients can handle the challenges of living without a natural bladder and live a fulfilling life.
Choosing the right medical team and facility is key to bladder reconstruction success. It’s a big decision that needs careful thought.
A team of specialists is vital for bladder reconstruction. This team includes urologists, oncologists, radiologists, and nurses. They work together to give you the best care. Liv Hospital believes in this team effort, making sure you get a treatment plan that fits your needs.
Benefits of Multidisciplinary Care:
It’s important to talk openly with your surgical team before surgery. Here are some questions to ask:
These questions help you understand what to expect and make a good decision.
Choosing a facility with the latest technology and specialized programs is important. Advanced centers often have better patient care and outcomes because of their high volume of procedures.
The role of specialized programs in bladder reconstruction is huge. These programs focus on giving you the best treatment for your condition.
By picking a team with the right skills and a facility with the latest tech, you get the best care for your bladder reconstruction.
Medical technology is getting better, and so is bladder reconstruction. Scientists are working hard on new ways to make a neo bladder that works like the real thing.
New surgical methods and materials are making bladder reconstruction better. This means patients can look forward to better results and a better life after surgery.
It’s important to know what happens after bladder surgery. For example, some people might see their pee turn neon yellow. This usually means they’re taking certain meds or vitamins. But, if you’re worried, always talk to a doctor.
We’re excited for the future of bladder reconstruction. We’re all about using the latest ideas to help our patients. We’re here to support you every step of the way.
Bladder reconstruction is a surgery to rebuild or replace the bladder. It’s needed for bladder cancer, birth defects, trauma, or diseases that harm bladder function.
Yes, living without a bladder is possible. You can have a neobladder, made from intestinal tissue, or urinary diversion. This means urine goes out through a stoma or in other ways.
A neobladder is a bladder made from intestine. It stores urine and helps with urination, but it’s not exactly like a natural bladder.
Reasons include bladder cancer, birth defects, neurogenic bladder, and severe damage from trauma or disease.
A team of healthcare experts makes the decision. They consider the condition, health, and personal choices.
Urinary diversion redirects urine out of the body, often through a stoma. It’s used when the bladder is removed or not working properly.
Challenges include adjusting to new urination, managing complications, and coping with the emotional changes.
Daily care involves learning to manage the neobladder or stoma, controlling urine, and dealing with issues like infections or leaks.
Support includes healthcare teams, support groups, and educational materials. They help manage the condition and adjust to changes.
A skilled team and reputable facility are key to the best results. They help avoid complications and provide full care.
Research is improving surgery, materials, and care after surgery. The goal is to achieve better outcomes and improve life for patients.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!