Last Updated on December 1, 2025 by Bilal Hasdemir

Getting a brain tumor or neurological cancer diagnosis can be scary. Specialized care is key in these situations. That’s where a brain tumor specialist steps in.
A neuro-oncologist is a doctor who deals with brain and spinal cord cancers. They are essential for handling tough cases and giving personalized care.
If you’ve been sent to a neuro oncology doctor, it means you need special treatment. Knowing what this specialist does can ease your worries. It also helps you understand your treatment better.
Key Takeaways
- A neuro-oncologist specializes in cancers of the brain and spinal cord.
- Referral to a neuro-oncologist indicates the need for specialized care.
- These specialists provide tailored treatment plans for complex cases.
- Understanding the role of a neuro-oncologist can help patients navigate their diagnosis.
- Specialized care is vital for effective treatment and management.
What Is a Neuro Oncologist and Their Specialized Role
Neuro-oncologists are doctors who focus on brain and spinal cord cancers. They handle diagnosis, treatment, and management of these complex tumors.
Education and Training Requirements
To become a neuro-oncologist, one needs a lot of education and training. This includes medical school, residency in neurology or oncology, and sometimes a fellowship in neuro-oncology. This training prepares them to handle tough cases.
Key components of their training include:
- Understanding the pathology and molecular characteristics of brain and spinal cord tumors.
- Familiarity with advanced neuroimaging techniques.
- Knowledge of various treatment modalities, including surgery, radiation therapy, and chemotherapy.
How They Differ from General Neurologists and Oncologists
Neuro-oncologists are different from general neurologists and oncologists. They have specialized training in neurological cancers. While neurologists treat neurological disorders and oncologists manage cancers, neuro-oncologists focus on brain and spinal cord tumors.
“The complexity of brain tumors requires a multidisciplinary approach, and neuro-oncologists are at the forefront of this care, working closely with neurosurgeons, radiation oncologists, and other specialists.”
Areas of Expertise in Brain and Spinal Cord Tumors
Neuro-oncologists know a lot about brain and spinal cord tumors. They handle gliomas, meningiomas, and metastatic brain tumors. Their knowledge helps them give the best care to patients with rare and complex cancers.
Their areas of expertise include:
- Diagnosing and managing primary brain tumors.
- Treating metastatic brain tumors.
- Providing care for patients with rare neurological cancers.
Common Symptoms That Lead to a Neuro Oncologist Referral
Neurological symptoms like seizures, headaches, or changes in thinking can lead to a visit to a neuro oncologist. These signs often mean there’s a tumor in the brain or spinal cord. This calls for more tests.
Neurological Symptoms That Raise Concerns
Some neurological symptoms are very worrying and might mean you need to see a neuro oncologist. These include:
- Seizures or convulsions
- Persistent or worsening headaches
- Cognitive changes, such as memory loss or confusion
- Motor symptoms, like weakness or paralysis
- Visual disturbances, including blurred vision or loss of peripheral vision
Table 1: Common Neurological Symptoms
| Symptom | Description |
| Seizures | Uncontrolled electrical activity in the brain, potentially causing convulsions |
| Headaches | Frequent or severe headaches that may indicate increased intracranial pressure |
| Cognitive Changes | Memory loss, confusion, or difficulty concentrating |
Suspicious Findings on Brain Imaging
Abnormal results from brain scans, like MRI or CT scans, can also mean a visit to a neuro oncologist. These might show:
- Tumors or masses in the brain or spinal cord
- Abnormal enhancement or lesions
- Edema or swelling around a tumor
When Primary Care Physicians Make the Referral
Primary care doctors are key in spotting patients who need a neuro oncologist. They refer patients based on:
- The presence of concerning neurological symptoms
- Abnormal findings on diagnostic tests, such as brain imaging
- A patient’s medical history and risk factors for brain tumors
Knowing what symptoms and test results lead to a referral helps patients. It guides them through their care and ensures they get the right treatment.
Types of Brain Tumors That Require Neuro Oncology Care
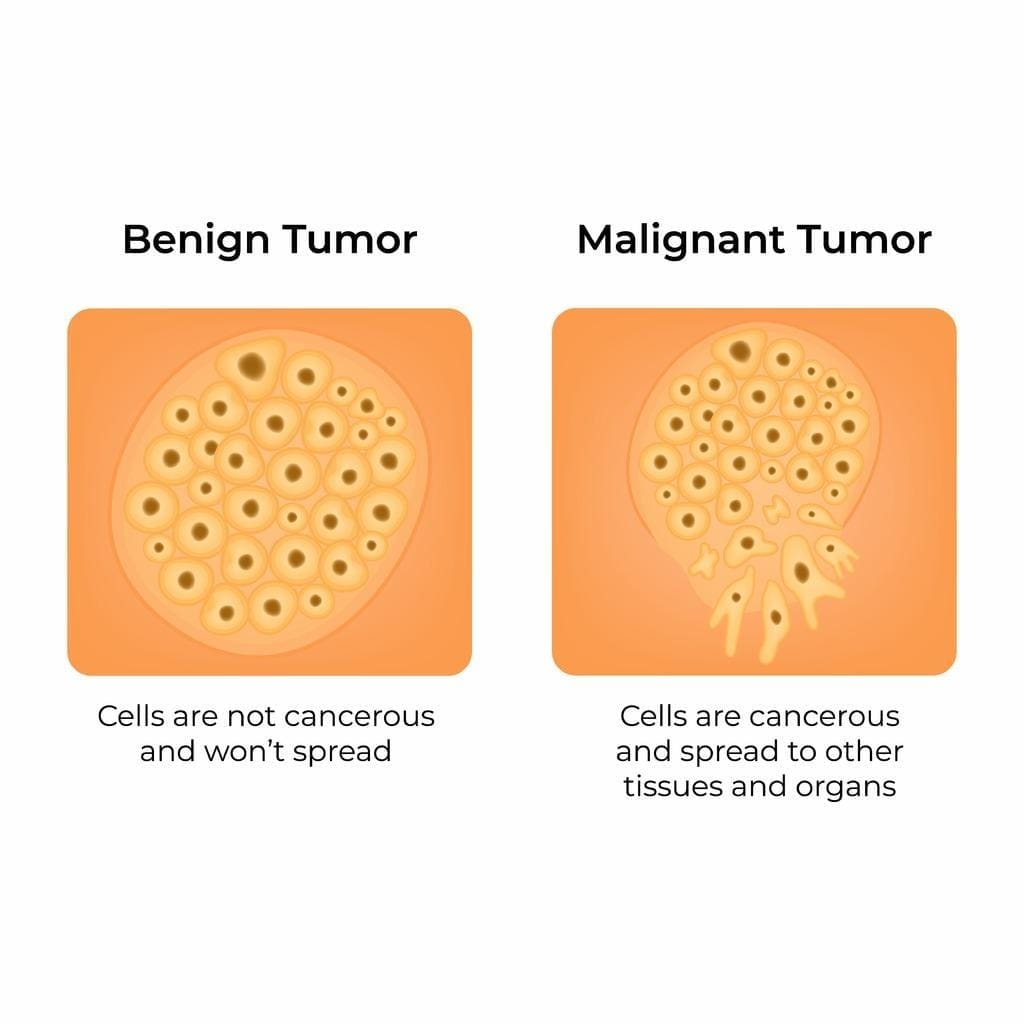
Brain tumors are divided into primary and metastatic types. Both need care from neuro oncologists. Knowing the types helps find the best treatment.
Primary Brain Tumors
Primary brain tumors start in the brain. They can be benign or malignant. The most common types are:
- Gliomas: These tumors come from brain cells and vary in severity.
- Meningiomas: Usually benign, these tumors grow in the brain’s protective membranes.
- Other types include ependymomas, medulloblastomas, and primitive neuroectodermal tumors (PNETs).
Metastatic Brain Tumors
Metastatic brain tumors come from cancer spreading to the brain. Common sources are:
- Lung cancer
- Breast cancer
- Melanoma
- Colon cancer
- Kidney cancer
These tumors are treated with surgery, radiation, and other treatments.
Rare and Complex Neurological Cancers
Some brain tumors are rare or complex. They can be hard to treat because of their location or behavior. Examples include:
- Pineal gland tumors: Near the brain’s center, these tumors are tough to treat.
- Pituitary adenomas: Though often benign, they can disrupt hormone balances.
- Skull base tumors: Close to important structures, these tumors are hard to treat.
Neuro oncologists team up with other experts to find effective treatments for these complex cases.
The Comprehensive Diagnostic Process
Getting a correct diagnosis is key in treating brain tumors. It uses top-notch imaging and detailed lab tests. When someone sees a neuro-oncologist, they start checking to find out what kind of tumor they have.
Initial Consultation and Medical History
The first step is the initial consultation. The neuro-oncologist looks at the patient’s health history. They check for symptoms, past illnesses, and family cancer history. This helps figure out what might have caused the tumor.
Patients talk about their symptoms in this meeting. They share when they started and any changes. This helps doctors understand how the disease might grow.
Advanced Neuroimaging Techniques
Advanced neuroimaging is very important for finding brain tumors. MRI and CT scans give clear pictures of the brain. They show where the tumor is, how big it is, and what kind it might be.
| Imaging Technique | Resolution | Use in Brain Tumors |
| MRI | High | Detailed tumor visualization |
| CT Scan | Moderate | Quick assessment, calcification detection |
| PET Scan | Functional | Metabolic activity assessment |
Treatment Approaches Offered by Neuro Oncologists
Neuro oncologists use many treatment methods for brain tumors. Each method is chosen based on the tumor’s type and stage. Often, a mix of treatments is needed.
Surgical Interventions and Their Goals
Surgery is a common first step for many brain tumors. The main goal is to remove as much tumor as possible. This is done while keeping the brain’s other parts safe.
New techniques like intraoperative MRI and awake craniotomy make surgery safer and more precise.
A study in the Journal of Neurosurgery found that removing more tumor tissue improves survival rates. This shows how important surgery is for better outcomes.
Radiation Therapy Options
Radiation therapy is also key for treating brain tumors. Neuro oncologists work with radiation experts to pick the best treatment plan. This might include:
- External beam radiation therapy (EBRT)
- Stereotactic radiosurgery (SRS)
- Stereotactic body radiation therapy (SBRT)
- Brachytherapy
These treatments can be used alone or with surgery and chemotherapy.
| Radiation Therapy Type | Description | Typical Use |
| EBRT | Delivers radiation from outside the body | Commonly used for gliomas and metastatic brain tumors |
| SRS | Delivers high-dose radiation to a precise target | Often used for small, well-defined tumors |
| SBRT | Delivers high-dose radiation to a precise target over several fractions | Used for larger tumors or those in sensitive areas |
Immunotherapy and Emerging Therapies
Immunotherapy uses the body’s immune system to fight cancer. It’s a growing area in neuro oncology. New therapies like checkpoint inhibitors and CAR-T cell therapy are showing promise.
As research grows, neuro oncologists are adding these new treatments to plans. This offers hope for better patient outcomes.
The Multidisciplinary Brain Tumor Team
Many doctors work together to treat brain tumors well. This team makes sure all parts of a patient’s care are covered. This way, patients get the best care possible.
Collaboration with Neurosurgeons
Neurosurgeons are key in treating brain tumors. They do surgeries to remove tumors or take samples. Their skills help decide the best surgery for each patient.
Key roles of neurosurgeons include:
- Performing surgical resections to remove as much of the tumor as possible
- Conducting biopsies to obtain tissue for pathological examination
- Collaborating with other specialists to plan a complete treatment
Working with Radiation Oncologists
Radiation oncologists plan and give radiation therapy for brain tumors. They work with others to make sure radiation hits the tumor right. This helps avoid harming healthy tissue.
The role of radiation oncologists involves:
- Designing radiation treatment plans tailored to the patient’s specific needs
- Delivering precise radiation therapy using advanced technologies
- Monitoring patient response and adjusting treatment as necessary
Role of Neuroradiologists and Neuropathologists
Neuroradiologists and neuropathologists are vital for diagnosis. Neuroradiologists look at scans to see the tumor’s details. Neuropathologists study samples to find out what kind of tumor it is.
| Specialist | Role |
| Neuroradiologists | Interpret imaging studies (MRI, CT scans) to assess tumor characteristics |
| Neuropathologists | Examine tissue samples to diagnose tumor type and grade |
Supportive Care Specialists
Supportive care specialists, like nurses and social workers, are very important. They help manage symptoms, offer emotional support, and help patients get back to normal. Their work greatly improves patients’ lives during treatment.
What to Expect at Your First Neuro Oncologist Appointment
Getting ready for your first neuro oncologist visit can reduce stress. It’s a key step to understand your diagnosis and treatment options.
Preparing for Your Visit
Before you go, collect all your medical records. This includes test results and imaging studies. Write down your symptoms, medications, and any questions you have. This helps your doctor understand your situation better.
Essential Questions to Ask Your Doctor
Don’t be shy to ask questions during your visit. Some important ones to ask include:
- What is the exact nature of my diagnosis?
- What are the available treatment options for my condition?
- What are the possible side effects of the treatments?
- Are there any clinical trials or new treatments I might be eligible for?
Asking the right questions helps you understand your treatment plan better.
Bringing a Support Person
Having someone with you during your appointment is very helpful. They can offer emotional support and help you remember important details. Feel free to bring a family member or friend. Their support can greatly help you understand the information given.
Non-Cancerous Conditions Treated by Neuro Oncologists
Neuro oncologists treat more than just brain tumors. They also handle non-cancerous conditions that affect the brain and nervous system. These conditions can greatly impact a patient’s life and need special care.
Benign Brain Tumors and Their Management
Neuro oncologists deal with benign brain tumors like meningiomas and acoustic neuromas. These tumors can press on important brain areas, causing symptoms. Treatment options include watching the tumor, surgery, or radiation, based on the tumor and patient’s health.
Skull Base Tumors
Skull base tumors are close to vital brain structures. Neuro oncologists team up with neurosurgeons to find the best treatment. They aim to treat the tumor effectively while keeping brain function intact.
Pituitary Adenomas and Other Endocrine Tumors
Pituitary adenomas are benign tumors in the pituitary gland. They can disrupt hormone levels, causing various disorders. Neuro oncologists, working with endocrinologists, use medicine, surgery, and radiation to manage these tumors.
Radiotherapy for Benign Tumors
Radiotherapy is used for benign tumors that can’t be treated with surgery or medicine. It helps control tumor growth and relieves symptoms. Neuro oncologists decide if radiotherapy is right and monitor its effects.
In summary, neuro oncologists treat many non-cancerous conditions. They use a team approach to manage complex cases and improve patient results.
Leading Neuro Oncology Centers in the United States
The United States has many top neuro oncology centers. They focus on treating brain and spinal cord tumors. These centers lead in research and treatment, giving patients new therapies and trials.
The Emotional Impact of Being Referred to a Neuro Oncologist
Getting referred to a neuro oncologist can stir up a lot of feelings. You might feel anxious or worried about what’s ahead. This moment can start a long and complex medical journey.
Coping with Fear and Uncertainty
When you get a diagnosis and a referral, you might feel scared, unsure, and anxious. It’s important to recognize these feelings and look for help.
Strategies for coping:
- Look for trustworthy sources to learn about your diagnosis and treatment options.
- Join support groups or online forums to connect with others and share experiences.
- Try stress-reducing activities like meditation or yoga to help manage your anxiety.
Support Resources for Patients and Families
Support is key for patients and their families when facing a brain tumor diagnosis. There are many resources available to offer emotional, informational, and practical help.
Available support resources include:
- Patient support groups, both in-person and online.
- Counseling services to help with emotional and psychological needs.
- Workshops and educational materials to learn about your condition and treatment.
“Support is not just about the patient; it’s about the entire family. Finding the right resources can make a significant difference in their journey.”
— A Neuro Oncologist
Communicating with Loved Ones About Your Diagnosis
Telling loved ones about your diagnosis can be tough but is very important. Being open and honest can help you build a strong support network.
Tips for effective communication:
- Be straightforward and clear about your diagnosis and what it means for you.
- Pick the right time and place for the talk, thinking about your feelings and theirs.
- Be ready to answer questions and share details about your treatment plan.
By understanding the emotional impact of a neuro oncologist referral and using available support, patients and their families can face this tough time better.
Living with a Brain Tumor: Long-term Care
Effective long-term care for brain tumor patients needs a team of healthcare experts. They work together to meet the patient’s needs.
Surveillance and Monitoring Protocols
Keeping an eye on brain tumors is key. This means regular imaging tests like MRI or CT scans. These tests check how the tumor is responding to treatment and if it’s changing.
Monitoring protocols include:
- Regular visits with the neuro oncologist
- Imaging tests at set times
- Checks on cognitive and physical health
Managing Treatment Side Effects
Treatment for brain tumors can cause side effects like fatigue and seizures. It’s important to manage these to keep quality of life high.
Ways to handle side effects include:
| Side Effect | Management Strategy |
| Fatigue | Save energy, exercise, and get enough sleep |
| Cognitive Changes | Rehabilitation, memory aids, and strategies to help |
| Seizures | Medicine and making lifestyle changes |
Rehabilitation and Quality of Life Considerations
Rehabilitation helps patients get back lost functions and adjust to changes. It includes physical, occupational, and speech therapy.
The goal of rehab is to improve quality of life. It helps patients do daily tasks and stay independent.
Survivorship Care Plans
A survivorship care plan outlines follow-up care for patients after treatment. It’s a guide for both patients and healthcare providers, ensuring ongoing care.
Parts of a survivorship care plan include:
- Summary of treatment
- Follow-up appointment and imaging study schedule
- Managing late treatment effects
- Healthy lifestyle tips
Pediatric Neuro Oncology: Special Considerations
Children with brain tumors face unique challenges. They need the help of pediatric neuro oncologists and a family-centered plan. Diagnosing and treating brain tumors in kids requires a caring and detailed approach.
Childhood Brain Tumors and Their Unique Challenges
Childhood brain tumors differ from adult ones in type, location, and behavior. Pediatric neuro oncologists are trained to handle these differences. They tailor care to each child’s needs.
Some common childhood brain tumors include:
- Medulloblastomas
- Gliomas
- Ependymomas
- Craniopharyngiomas
These tumors can cause headaches, nausea, vomiting, and neurological problems. Early diagnosis and treatment are key to better outcomes.
Family-Centered Treatment Approaches
Family-centered care is vital in pediatric neuro oncology. It involves the child and their family in treatment. Multidisciplinary teams create plans that meet the child’s medical, emotional, and social needs.
Key elements of family-centered care include:
- Clear communication between healthcare providers and families
- Families involved in decision-making
- Emotional and psychological support for the child and family
Long-term Follow-up and Educational Support
Children treated for brain tumors need ongoing care. Pediatric neuro oncologists monitor for late effects like cognitive or neurological problems. They work with specialists to provide full care.
Educational support is also vital for kids treated for brain tumors. Many need special educational services to reach their full abilities. Families and healthcare providers work together to create education plans tailored to each child.
Advances in Neuro Oncology Research and Treatment
Neuro oncology research is changing how we treat brain tumors. New discoveries about brain tumors’ genetics and molecules are leading to better treatments. These treatments are now more personalized.
Precision Medicine and Molecular Targeting
Precision medicine is key in neuro oncology. It means treatments are made just for each tumor’s unique traits. Molecular targeting focuses on specific genetic changes that help tumors grow.
Clinical Trials: Access and Eligibility
Clinical trials are vital for neuro oncology progress. They test new treatments. Patients get access to therapies not yet widely available. Knowing how to join these trials is important for those seeking the latest care.
Promising New Therapies on the Horizon
The future of neuro oncology looks bright. New therapies are coming, like immunotherapies and new ways to use chemotherapy and radiation.
Improving Survival Rates and Quality of Life
The main aim of neuro oncology advances is to help patients live longer and better. By finding better treatments and care, doctors are making big progress.
When to Seek a Second Opinion from Another Neuro Oncologist
Getting a second opinion from a neuro-oncologist is common for those looking at all treatment options for brain tumors. It’s very helpful when the diagnosis is tricky or rare, or when treatments face challenges.
Complex or Rare Diagnoses
Patients with unusual or hard-to-diagnose brain tumors can find clarity with a second opinion. Specialized neuro-oncologists often have experience with similar cases. They can offer insights that change treatment plans.
Treatment Challenges or Failures
If first treatments don’t work or cause big side effects, a second opinion can help. Neuro-oncologists can suggest new ways to tackle treatment-resistant tumors.
How to Request and Prepare for a Second Opinion
To ask for a second opinion, gather your medical records, like imaging studies and pathology reports. It’s key to be ready to talk about your medical history and current treatment with the new neuro-oncologist.
By getting a second opinion, patients can understand their condition better. They can also look into more treatment options. This helps them make better choices about their care.
Conclusion: Partnering with Your Neuro Oncologist for Optimal Care
Getting a brain tumor diagnosis can feel overwhelming. But, working with a neuro oncologist is key to getting the best care. They offer expert advice and treatment plans that fit your needs, helping to improve your chances of recovery.
When you team up with a neuro oncologist, you get access to the newest treatments for brain tumors. This team effort means you get care that covers everything from diagnosis to aftercare. It’s a full-circle approach to health.
Good communication is essential in this partnership. Patients should ask questions, share their worries, and ask for help when they need it. This way, they can feel supported and understood.
In the end, teaming up with a neuro oncologist can greatly improve your care. Together, you can tackle the challenges of brain tumor treatment and aim for the best results.
FAQ
What is a neuro oncologist, and what do they specialize in?
A neuro oncologist is a doctor who deals with brain and spinal cord tumors. They handle both cancerous and non-cancerous growths.
What are the symptoms that may lead to a referral to a neuro oncologist?
Signs like headaches, seizures, and weakness might lead you to see a neuro oncologist. Also, changes in vision, speech, or thinking can be a reason for a visit.
What types of brain tumors do neuro oncologists treat?
Neuro oncologists treat many brain tumors. This includes gliomas, meningiomas, and metastatic tumors. They also handle rare and complex cancers.
What is the role of a neuro oncologist in the treatment of brain tumors?
Neuro oncologists work with a team to plan treatments. This might include surgery, radiation, or chemotherapy. They tailor plans to each patient’s needs.
How do I prepare for my first appointment with a neuro oncologist?
For your first visit, collect your medical records and imaging studies. Make a list of questions. Bringing a support person is also helpful.
Can neuro oncologists treat non-cancerous conditions?
Yes, they can treat non-cancerous conditions too. This includes benign tumors and skull base tumors. They might use radiotherapy for these cases.
What is the difference between a neuro oncologist and a general neurologist or oncologist?
Neuro oncologists specialize in brain and spinal cord tumors. They have more training than general neurologists and oncologists.
How do I find a qualified neuro oncologist or neuro oncology center?
To find a good neuro oncologist, ask your doctor for a referral. Look for NCI-designated centers online. Check for professional certifications too.
What are the benefits of seeking a second opinion from another neuro oncologist?
Getting a second opinion can offer new insights. It might change your diagnosis or treatment plan. This is very helpful for complex cases.
What advancements are being made in neuro oncology research and treatment?
New treatments like precision medicine and immunotherapy are improving care. Clinical trials are exploring more options. This is helping patients live better lives.
References
National Center for Biotechnology Information. Provider-reported challenges and barriers to referring patients to neuro-oncology clinical trials: a report from the Society for Neuro-Oncology member survey. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC7104882/