Last Updated on December 1, 2025 by Bilal Hasdemir
Nearly 70,000 new cases of brain and spinal cord tumors are diagnosed each year in the United States. This raises important questions about the role of neuro oncologists in surgery. Do neuro oncologists perform neuro oncologist surgery? Get the surprising, critical facts. Learn their essential role in the treatment team.
Neuro oncologists focus on treating brain and spinal cord tumors. They mainly use non-surgical methods like chemotherapy and radiation. But, they also play a big part in brain tumor surgery.
Working together, neuro oncologists and neurosurgeons decide the best treatment for patients. It’s important for patients to know about neuro oncologists’ role in surgical procedures.
Key Takeaways
- Neuro oncologists are key in diagnosing and treating brain and spinal cord tumors.
- They are important in surgery, adding to patient care.
- Working with neurosurgeons helps find the best treatment.
- Knowing what neuro oncologists do is important for patients.
- They mainly use non-surgical treatments like chemotherapy and radiation.
Understanding the Role of Neuro-Oncologists
Neuro-oncologists are doctors who specialize in brain and spinal cord cancers. They are key in diagnosing, treating, and managing these cancers. Their work is vital for those with nervous system cancers.
Primary Responsibilities in Cancer Care
Neuro-oncologists diagnose and treat brain and spinal cord cancers. They do:
- Conduct thorough medical evaluations and diagnostic tests to find out the cancer type and extent.
- Make personalized treatment plans that might include chemotherapy, targeted therapy, or other non-surgical methods.
- Work with other specialists, like neurosurgeons and radiation oncologists, for a complete treatment plan.
| Responsibility | Description |
| Diagnosis | Conducting thorough evaluations and diagnostic tests. |
| Treatment Planning | Developing personalized treatment plans. |
| Care Coordination | Working with other specialists for complete care. |
Neuro-oncologists are key in fighting CNS cancers. They offer expert care and guidance to patients during their treatment.
Neuro-Oncologists vs. Neurosurgeons: Key Differences

Neuro-oncologists and neurosurgeons are key players in treating brain cancers. They work together but have different areas of focus. This teamwork is vital for a patient’s care.
Educational Pathways and Training
Neurosurgeons and neuro-oncologists have different paths to their careers. Neurosurgeons go through a long surgical training after medical school. This training can last six to seven years.
Neuro-oncologists, on the other hand, are medical oncologists with a focus on brain cancers. They get specialized training in neuro-oncology through fellowships.
This training shows their roles are different. Neurosurgeons do surgeries like tumor removals. Neuro-oncologists manage brain tumors with treatments like chemotherapy.
Clinical Focus and Expertise
Neurosurgeons focus on surgeries for brain and spinal issues, including tumors. They use various techniques, from open surgeries to minimally invasive ones.
Neuro-oncologists handle non-surgical treatments for brain tumors. They interpret tests, plan treatments, and manage symptoms.
Collaborative Relationship in Patient Care
Neuro-oncologists and neurosurgeons work together for brain tumor patients. They decide on the best treatment plan together. This plan often includes surgery and other treatments.
They discuss surgery options based on the patient’s health and the tumor’s type and location. This teamwork ensures patients get the best care.
The Truth About Neuro Oncologist Surgery Involvement
It’s important to know how neuro-oncologists help with brain tumor surgeries. They are key in the care team for brain tumor patients. They help plan and decide on the best treatment, including surgery.
Direct Surgical Participation
Neuro-oncologists don’t usually do the surgery themselves. But, they are very important in managing brain tumor patients. They help decide the best treatment, which can be surgery, chemo, radiation, or a mix.
Neuro-oncologists don’t usually do the surgery. They focus on the medical side of brain tumors. Neurosurgeons do the actual surgery, like removing tumors.
Collaborative Surgical Planning
Neuro-oncologists work with neurosurgeons and others to plan the best treatment. This team approach makes sure all parts of the patient’s care are considered. It helps make the best treatment plan.
“The collaboration between neuro-oncologists and neurosurgeons is critical in optimizing patient outcomes. By working together, we can develop a treatment plan that addresses both the surgical and medical needs of our patients.”
In brain tumor surgery, neuro-oncologists help plan by knowing about the tumor. They know how it might react to chemo or radiation. This helps decide the best surgical approach.
Decision-Making Authority in Treatment
Neuro-oncologists have a big say in the treatment plan for brain tumor patients. They work with a team to decide on treatments. This includes if surgery is needed and how it fits with other treatments.
| Treatment Modality | Role of Neuro-Oncologist | Collaborating Specialists |
| Surgery | Planning and decision-making | Neurosurgeons, Radiologists |
| Chemotherapy | Administration and monitoring | Oncology Nurses, Pharmacists |
| Radiation Therapy | Planning and coordination | Radiation Oncologists, Radiologists |
The table shows how neuro-oncologists work in different treatments. It also shows they work with other experts.
The Multidisciplinary Approach to Brain Tumor Treatment
Brain tumors need a team effort from many doctors. A good plan involves experts from different fields. This team works together to treat brain cancer well.
Coordination of Care Across Specialties
Good teamwork is vital for patient care. Doctors talk often, make decisions together, and focus on the patient. They aim to integrate all care aspects well.
- Regular team meetings to discuss patient cases
- Collaborative development of treatment plans
- Continuous monitoring of patient progress
Tumor Board Conferences and Treatment Planning
Tumor board meetings are key. They bring the team together to talk about tough cases. Here, the team’s knowledge helps make treatment plans that fit each patient.
In summary, teamwork is key in treating brain tumors. The neuro-oncology team works together. This leads to better care and a better life for patients.
Common Types of Brain Tumors Requiring Surgical Intervention
Many brain tumors need surgery as part of their treatment. These tumors differ in how they grow and affect health.
Gliomas and Glioblastomas
Gliomas start from the brain’s glial cells. Glioblastomas, a type of glioma, grow fast and are serious. Surgery is often the first step to remove as much of the tumor as possible.
Meningiomas
Meningiomas are usually not cancerous and grow slowly. They start from the meninges, which protect the brain and spinal cord. But, big or bothersome tumors might need to be surgically removed.
Metastatic Brain Tumors
Metastatic brain tumors come from cancer spreading to the brain. Surgery might be an option for those with a few tumors, if the main cancer is under control.
Pituitary Adenomas
Pituitary adenomas grow in the pituitary gland at the brain’s base. Most are not cancerous but can cause problems. Surgery, often through the nose, is a common treatment.
| Tumor Type | Nature | Typical Treatment Approach |
| Gliomas/Glioblastomas | Malignant | Surgery, followed by radiation and chemotherapy |
| Meningiomas | Usually benign | Surgery, possibly followed by radiation for atypical or malignant types |
| Metastatic Brain Tumors | Malignant | Surgery, radiation therapy, and systemic therapy for the primary cancer |
| Pituitary Adenomas | Usually benign | Surgery, medical management, or radiation therapy based on tumor characteristics |
Choosing surgery for these tumors depends on many things. These include the tumor’s type, size, where it is, and the patient’s health.
Spinal Tumor Surgery and Neuro-Oncology Care
Managing spinal tumors is a complex task. It requires both surgery and neuro-oncology care. Spinal tumors are hard to diagnose and treat. They need a care plan that includes surgery and other treatments.
Types of Spinal Tumors
Spinal tumors can be benign or malignant. Benign tumors grow slowly and might not need surgery right away. Malignant tumors, like chordomas, grow fast and need quick treatment.
Common Types of Spinal Tumors:
- Schwannomas
- Meningiomas
- Chordomas
- Sarcomas
- Metastatic tumors
Knowing the type of tumor is key to choosing the right treatment. Treatments can include surgery, radiation, or both.
Surgical Approaches to Spinal Tumors
Surgery for spinal tumors aims to remove the tumor while keeping nerves safe. The surgery type depends on the tumor’s location, size, and type, and the patient’s health.
“The goal of surgery is to achieve a balance between tumor removal and preservation of spinal stability and neurological function.”
There are different surgical techniques:
- Posterior approach, used for tumors in the spine’s back part.
- Anterior approach, for tumors in the vertebral body.
- Combined approach, for complex tumors across multiple segments.
Post-Surgical Management
After surgery, care is vital. It includes watching for complications, managing pain, and starting rehabilitation. These steps help patients recover and improve their quality of life.
“Effective post-surgical management requires a multidisciplinary team approach, involving neurosurgeons, oncologists, rehabilitation specialists, and other healthcare professionals.”
Key post-surgical care aspects include:
| Aspect | Description |
| Pain Management | Using medicines and other methods to control pain. |
| Rehabilitation | Starting physical therapy and other strategies to improve function. |
| Monitoring for Complications | Watching for signs of infection, nerve problems, or other issues. |
Brain Tumor Surgery Techniques and Procedures
Medical technology has changed brain tumor surgery a lot. It now offers hope to those with tough tumors. Neurosurgery has made big steps forward, making patients’ lives better and recovery times shorter.
Craniotomy and Open Resection
A craniotomy means taking part of the skull off to get to the tumor. This open resection lets surgeons see and take out the tumor. It’s a big surgery, but new ways have made it safer and more effective.
Minimally Invasive Approaches
There are now smaller ways to do brain tumor surgery. These methods use tiny cuts and disturb less brain tissue. This can mean patients heal faster and face fewer problems. Endoscopic surgery is one, using special tools and cameras through small openings.
Awake Brain Surgery
Awake brain surgery keeps the patient awake during surgery. This lets the surgeon check brain functions as they work. It’s a team effort to keep the patient safe and comfortable.
Laser Interstitial Thermal Therapy
Laser interstitial thermal therapy (LITT) uses laser heat to kill tumor cells. A laser probe is put into the tumor, guided by MRI. It’s good for tumors that are hard to reach or in sensitive spots.
Choosing the right brain tumor surgery depends on many things. Like where the tumor is, how big it is, and the patient’s health. Neurosurgery keeps getting better, giving patients more options and better chances.
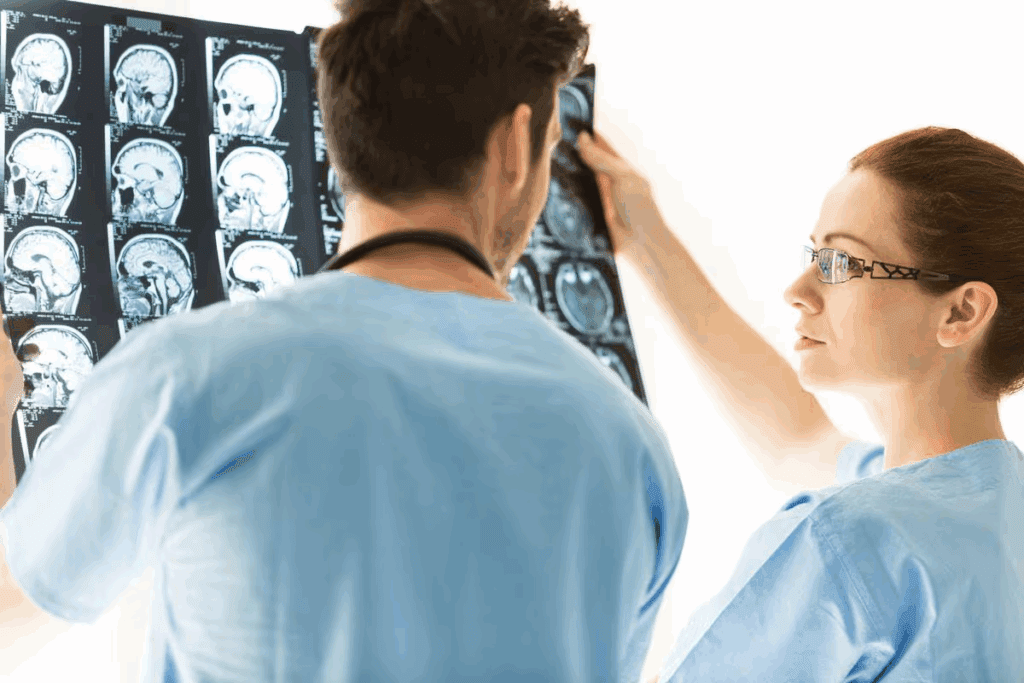
Diagnostic Procedures in Neuro-Oncology
Getting a correct diagnosis is key to treating neurological cancers. This involves using advanced diagnostic methods.
These methods help find out what kind of cancer it is, how serious it is, and how far it has spread. This information helps doctors decide the best treatment plan.
Biopsy Techniques
Biopsy is a main tool in diagnosing brain cancers. It takes tissue samples for lab tests.
Types of Biopsy:
- Stereotactic biopsy: Uses a special frame and imaging to get tissue from specific brain spots.
- Open biopsy: Requires opening the skull to get a sample, often done during surgery.
- Needle biopsy: A less invasive method using a needle to collect tissue or fluid.
Advanced Imaging Methods
Modern imaging is essential for diagnosing and understanding brain cancers.
Imaging Modalities:
| Modality | Description | Application in Neuro-Oncology |
| MRI | Magnetic Resonance Imaging | Shows detailed brain images, helping locate and understand tumors. |
| CT Scan | Computed Tomography Scan | Fast checks for complications like bleeding or fluid buildup in the brain. |
| PET Scan | Positron Emission Tomography Scan | Looks at how active tumors are, helping gauge their grade and how well they respond to treatment. |
Molecular and Genetic Testing
Molecular and genetic tests are now vital in neuro-oncology. They reveal the genetic makeup of tumors.
Key Tests:
- IDH mutation testing: Finds mutations in the isocitrate dehydrogenase genes, which affect prognosis.
- MGMT promoter methylation testing: Shows how the MGMT gene promoter is methylated, which helps predict chemotherapy response.
- 1p/19q codeletion testing: Looks for codeletions on chromosomes 1p and 19q, linked to better prognosis and treatment response.
Non-Surgical Treatments Coordinated by Neuro-Oncologists
Neuro-oncologists lead the fight against brain tumors with non-surgical treatments. These treatments help patients get better care. They work with surgery to give patients the best treatment.
Chemotherapy Protocols
Chemotherapy is also a big part of treating brain tumors. Neuro-oncologists create special plans for each patient. Temozolomide is often used for glioblastoma, along with radiation.
- Adjuvant chemotherapy: given after surgery to kill cancer cells left behind.
- Neoadjuvant chemotherapy: used before surgery to shrink the tumor.
Targeted Therapies and Immunotherapy
Targeted therapies and immunotherapy are new ways to fight brain tumors. They aim at specific tumor traits for better treatment. Bevacizumab is used for glioblastoma.
Immunotherapy uses the body’s immune system to fight cancer. It’s being tested in clinical trials. This includes checkpoint inhibitors and CAR-T cell therapy.
When Is Neuro Oncologist Surgery Recommended?
Deciding on surgery in neuro oncology involves many factors. It looks at the patient’s health, the tumor’s type and location, and the surgery’s benefits and risks.
Indicators for Surgical Intervention
Some signs point to the need for surgery in neuro oncology. These include:
- Tumor type and location
- Symptoms caused by the tumor
- Potential for significant improvement in quality of life
- Diagnostic uncertainty requiring biopsy
These signs lead to a detailed check to see if surgery is right.
Risk-Benefit Analysis
Doing a thorough risk-benefit analysis is key. It compares the surgery’s benefits, like removing the tumor, to its risks, like complications.
Important things to think about are:
- The patient’s overall health and comorbidities
- The tumor’s characteristics and behavior
- Other treatment options and their outcomes
Patient-Specific Considerations
Each patient’s situation is unique when it comes to surgery. Factors like age, health, and personal choices matter a lot.
A personalized approach makes sure the treatment fits the patient’s needs.
Healthcare providers use these factors to decide if surgery is right.
Post-Surgical Care and Monitoring
Patients who have had neurosurgical oncology surgery need careful care after surgery. This care is key for a good recovery. It involves looking after the patient’s health in many ways.
Immediate Recovery Protocols
Right after surgery, doctors watch the patient very closely. They keep them in an intensive care unit (ICU). This way, they can quickly handle any problems.
“The first 24 to 48 hours after surgery are very important,” say top neurosurgical oncologists. They look for signs of bleeding, infection, or brain problems.
Doctors also give pain management drugs to help the patient feel better. They keep an eye on the patient’s vital signs and brain function. This helps catch any bad effects early.
Long-term Surveillance
Keeping an eye on the patient over time is also important. This helps see how they’re doing and if the tumor is coming back. They have regular check-ups with their doctors and may have scans like MRI or CT.
Doctors also tell patients about lifestyle changes that can help them get better. This includes eating right, staying active, and managing stress. The goal is to help the patient stay healthy and live well.
Managing Surgical Complications
Handling problems after surgery is a big part of care. These problems can be infections or brain issues. Doctors need to work together to fix these problems.
‘Finding and treating problems quickly is very important. It helps the patient recover better and stay healthy longer.’
This might mean more surgery, medicine, or other treatments. Each patient’s needs are different.
Advanced Technologies in Neurosurgical Oncology
Technology has changed neurosurgical oncology, bringing new hope to patients with brain tumors. New tools have made diagnosis and surgery better, leading to better results for patients.
Intraoperative Mapping and Monitoring
Intraoperative mapping and monitoring are key in neurosurgical oncology. They help surgeons avoid harming important brain parts during surgery. Tools like electrocorticography and subcortical mapping help find tumor edges and safe areas.
Monitoring during surgery gives surgeons instant feedback. This lets them make changes on the fly. It helps remove more tumor and lowers the chance of brain damage after surgery.
Fluorescence-Guided Surgery
Fluorescence-guided surgery is a big step forward in neurosurgical oncology. It uses special dyes that light up tumors, making them stand out. 5-aminolevulinic acid (5-ALA) is a dye that helps surgeons see tumor edges better.
This method helps surgeons remove tumors more effectively. It could lead to better results for patients.
Robotic and Computer-Assisted Navigation
Robotic and computer-assisted systems have changed neurosurgery. They give surgeons precise, real-time guidance during tough surgeries. Robotic systems make tumor removal more accurate and safer.
Computer systems help with planning before surgery and guide during it. This makes neurosurgical procedures more precise.
Patient Experience: From Diagnosis Through Treatment
The journey of a patient with a brain tumor is complex. It involves many stages from diagnosis to treatment. Healthcare providers need to understand this journey to give the best care.
Initial Consultation Process
The first step is the initial consultation. Here, the diagnosis is discussed, and treatment options are explored. Patients get a thorough evaluation, including their medical history and test results.
Key aspects of the initial consultation include:
- Discussion of diagnosis and prognosis
- Exploration of treatment options, including surgery, radiation, and chemotherapy
- Addressing patient questions and concerns
Preparing for Brain Tumor Surgery
Preparing for surgery is both physical and emotional. Patients must follow pre-operative instructions from their healthcare team. This includes guidelines on medication, nutrition, and lifestyle.
Pre-operative preparations may involve:
- Stopping certain medications that may interfere with surgery
- Undergoing additional diagnostic tests to assess overall health
- Arranging for post-operative care and support
Recovery and Rehabilitation Expectations
Recovery from surgery varies. It depends on the individual, the surgery type, and the tumor’s characteristics. Patients may feel tired, uncomfortable, and experience cognitive changes.
A good recovery plan includes:
| Recovery Aspect | Description | Timeline |
| Immediate Post-Surgery | Monitoring in ICU, pain management | First few days |
| Short-term Recovery | Gradual return to normal activities, rehabilitation therapy | Several weeks |
| Long-term Recovery | Full recovery, follow-up appointments, long-term effects management | Months to years |
During recovery, patients are supported by a team of healthcare professionals. This team includes neurosurgeons, neuro-oncologists, rehabilitation specialists, and nurses. They work together to meet the patient’s physical, emotional, and cognitive needs.
Specialized Training for Neuro-Oncology Professionals
Neuro-oncology professionals need a lot of training and learning. They must go through tough education and training to be experts in their field.
Fellowship Requirements
To be good at neuro-oncology, one must do a fellowship program. This program gives advanced training in brain and spinal tumors. It’s usually in special cancer centers and hospitals.
This training covers many topics. It includes:
- Advanced diagnostic techniques
- Treatment methods like surgery, radiation, and chemotherapy
- Managing clinical trials
- Palliative care
Continuing Education
Neuro-oncology professionals must keep learning. They do this by going to conferences, workshops, and online courses.
They focus on many areas. These include:
| Topic | Description | Frequency |
| New Treatment Modalities | Updates on latest treatments and therapies | Annual |
| Clinical Trial Updates | Reviews of ongoing and completed clinical trials | Quarterly |
| Advances in Diagnostic Techniques | New methods and technologies in diagnosis | Bi-annually |
Certification and Expertise Development
Certification is key for neuro-oncology professionals. It shows they are experts and care about quality. They need to be certified in medical oncology, radiation oncology, or neurological surgery.
To keep their certification, they must:
- Complete continuing education
- Do peer review and quality improvement
- Keep up with new guidelines
By getting fellowship training, continuing education, and certification, neuro-oncology professionals become top-notch. They can give the best care to their patients.
Emerging Trends in Neuro-Oncology Treatment
Neuro-oncology is seeing big changes in how we treat brain tumors. New treatments and technologies are coming along. They bring hope for better results for patients.
Precision Medicine Applications
Precision medicine is changing neuro-oncology. It makes treatments fit each patient’s needs. This means:
- Genetic tests to find out what’s in the tumor
- Therapies that target those specific traits
- Treatment plans made just for each patient
Precision medicine makes treatments work better and have fewer side effects. It focuses on the tumor’s genetic makeup. This way, doctors can offer treatments that are more effective and less harsh.
Novel Therapeutic Approaches
New ways to treat neuro-oncology are being looked into. Some of these include:
- Immunotherapy, which uses the body’s immune system to fight cancer
- Gene therapy, to fix genetic problems that cause tumors
- Oncolytic virus therapy, which uses viruses to kill cancer cells
These new therapies are showing great promise in trials. They are set to be big players in neuro-oncology’s future.
Future Directions in Surgical Techniques
The future of surgery in neuro-oncology is all about being more precise and less invasive. We’re seeing:
- Robot-assisted surgery, for better control and accuracy
- Intraoperative imaging and mapping, for adjustments during surgery
- Laser interstitial thermal therapy, a new way to treat tumors
These advancements aim to make surgery better and faster for patients. They could lead to quicker recoveries.
Conclusion: The Collaborative Nature of Neuro-Oncology Care
Caring for patients with brain and spinal cord tumors is a team effort. Neuro-oncology care brings together many healthcare experts. They work as one to offer complete treatment plans.
This team approach helps patients get the best care. Neuro-oncologists, neurosurgeons, and others create treatment plans tailored to each patient. Their combined skills make treatment more effective.
The role of a multidisciplinary team in neuro-oncology is huge. They use the latest treatments and technologies. This teamwork boosts patients’ chances of a good outcome.
Neuro-oncology care works best when all specialties work together. This teamwork helps meet the complex needs of patients. It improves care and results for those with brain and spinal cord tumors.
FAQ
What is the role of a neuro-oncologist in cancer care?
Neuro-oncologists focus on treating nervous system cancers. This includes brain and spinal tumors. They help plan and coordinate care for patients.
Do neuro-oncologists perform surgery?
No, neuro-oncologists are not surgeons. But they work with neurosurgeons to plan the best treatment. They decide if surgery is needed.
What is the difference between a neuro-oncologist and a neurosurgeon?
Neuro-oncologists manage medical treatment for brain cancers. Neurosurgeons do surgery for brain tumors. They have different training and skills.
What types of brain tumors require surgical intervention?
Some brain tumors need surgery. These include gliomas, meningiomas, and metastatic tumors. Each type has its own treatment plan.
What is the role of tumor board conferences in treatment planning?
Tumor board conferences are key. They bring together experts to plan treatment. This includes neuro-oncologists, neurosurgeons, and others.
What are the latest developments in radiation therapy for brain tumors?
New radiation therapy methods are available. These include stereotactic radiosurgery and intensity-modulated radiation therapy. Neuro-oncologists help choose the best option.
How do neuro-oncologists coordinate non-surgical treatments?
Neuro-oncologists create personalized treatment plans. They use chemotherapy, targeted therapies, and more. They also coordinate radiation therapy.
What are the indicators for surgical intervention in brain tumor treatment?
Surgery is considered based on tumor size and location. Patient health and symptoms are also important. A risk-benefit analysis is done.
What is the importance of post-surgical care and monitoring?
Post-surgery care is vital. It includes recovery, long-term monitoring, and managing complications. Patients get full support during treatment.
How do advanced technologies enhance neurosurgical oncology?
New technologies improve surgery for brain tumors. They include intraoperative mapping and robotic navigation. These make surgery safer and more effective.
What can patients expect during the initial consultation process?
Patients get a thorough evaluation at the first meeting. This includes tests and talks with the healthcare team. They find the best treatment for their condition.
What specialized training do neuro-oncology professionals require?
Professionals in neuro-oncology get a lot of training. They go through fellowship programs and get certified. This helps them provide top-notch care.
What emerging trends are shaping the future of neuro-oncology treatment?
New trends are changing neuro-oncology. These include precision medicine and new treatments. They offer hope for patients with brain and spinal tumors.
References
New England Journal of Medicine. Evidence-Based Medical Insight. Retrieved from https://www.nejm.org/doi/full/10.1056/NEJMra0708126