Last Updated on December 1, 2025 by Bilal Hasdemir
Nearly 30% of cancer patients face neurological issues. This shows how important neurologists are in brain tumor management. The critical role of neurologists in Neuro-oncology care. Discover the amazing, essential support they provide for non-surgical symptoms.
Neurologists are key in diagnosing and treating central nervous system tumors. They work with oncologists to give full neuro-oncology care.
Brain and nervous system cancers are complex. Neurologists add their expertise to help patients get better.
Key Takeaways
- Neurologists are essential in managing neurological complications in cancer patients.
- A multidisciplinary approach is key in treating brain and nervous system cancers.
- Neurologists work closely with oncologists to provide full care.
- Central nervous system tumors need special diagnosis and treatment.
- Brain tumor management involves a team of healthcare professionals.
The role of neurologists in cancer care has evolved significantly over time.

The role of neurologists in cancer care has evolved significantly over time. They are now a key part of treating cancer, not just fixing problems.
Historical Perspective on Neurologists in Oncology
Before, neurologists mainly dealt with brain problems caused by cancer or treatment. They focused on brain tumors or nerve damage from chemo.
Current Integration in Cancer Treatment Teams
Now, neurologists are a big part of cancer teams. They help with oncologic neurology by managing brain issues, seizures, and thinking problems.
- They work with brain surgeons and radiation experts to plan treatments.
- They join tumor boards to talk about tough cases.
- They help manage side effects of cancer treatments.
Unique Expertise Neurologists Bring to Oncology
Neurologists have special skills for cancer care. They can read brain scans, handle complex symptoms, and manage patients with brain problems.
Research shows that having neurologists on cancer teams helps patients more. It shows how important they are in multidisciplinary care.
Understanding Neuro-Oncology: A Specialized Field
Neuro-oncology deals with many conditions, like brain tumors and cancer that spreads. It’s a complex field that needs a deep understanding of cancer and the nervous system. It also involves knowing how different treatments work.
Definition and Scope of Neuro-Oncology
Neuro-oncology is about studying and treating tumors in the brain and nervous system. It covers a wide range of cancers, from those that start in the brain to those that spread from other places.
Types of Central Nervous System Tumors
CNS tumors are divided into two main types: primary and metastatic. Primary tumors start in the brain or spinal cord. Metastatic tumors come from other parts of the body. Common primary tumors include gliomas, meningiomas, and medulloblastomas.
Systemic Cancers Affecting the Nervous System
Systemic cancers can harm the nervous system in different ways. This includes spreading to the brain, causing other symptoms, or being side effects of treatment. Cancers like lung, breast, and melanoma often spread to the brain. It’s important to understand these effects to give the best care to patients.
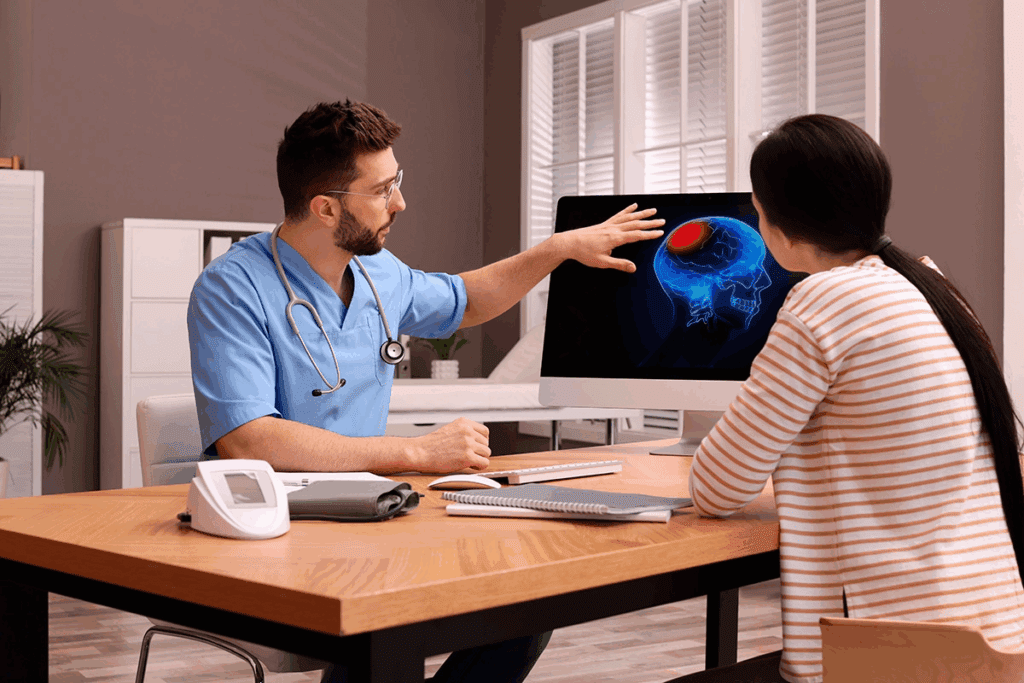
Diagnostic Contributions of Neurologists
Neurologists are key in finding brain tumors. They use clinical checks and advanced tests. Their skills help in spotting and treating brain tumors well.
Neurological Examination in Tumor Detection
First, neurologists do a detailed check-up. They look at brain functions like thinking, nerve work, and how muscles move. If something’s off, it might mean a tumor is there.
Clinical evaluation helps spot signs of a brain tumor. This leads to more tests to find out what’s wrong.
Interpretation of Neuroimaging Studies
Scans like MRI and CT are key for finding brain tumors. Neurologists know how to read these images. They figure out where the tumor is, how big it is, and how it affects the brain.
“The precision in diagnosing brain tumors largely depends on the accurate interpretation of neuroimaging studies.”
Neurophysiological Testing in Diagnosis
Tests like EEG and EMG give more details. They show how the brain and nerves work. Neurologists use this info to plan the best treatment.
Adding neurophysiological testing helps understand how the tumor affects the brain. This makes treatment planning better.
Comprehensive Neuro-Oncology Care: The Neurologist’s Approach
Neurologists take a complete approach to neuro-oncology care. They use patient-centered strategies and work with many healthcare teams. This way, patients get care that fits their needs, improving their life quality.
Patient-Centered Assessment Strategies
Neurologists focus on what each patient needs and wants. They do a detailed check-up, look at the patient’s health history, and check their symptoms and how they function.
Key components of patient-centered assessment include:
- Comprehensive neurological evaluation
- Assessment of cognitive and emotional status
- Evaluation of functional abilities and daily living activities
Continuity of Care Throughout the Disease Course
Neuro-oncology patients need ongoing care. Neurologists make sure care is smooth and continuous. They work with other doctors to meet the patient’s changing needs.
Coordination with Primary Oncology Teams
Working well with primary oncology teams is key for neuro-oncology patients. Neurologists team up with oncologists and others to plan treatments. They focus on both the brain and cancer aspects of the patient’s health.
| Coordination Aspect | Description | Benefits |
| Multidisciplinary Team Meetings | Regular meetings between neurologists, oncologists, and other specialists to discuss patient care. | Enhanced collaboration and coordinated care planning. |
| Shared Electronic Health Records | Use of shared electronic records to ensure all healthcare providers have access to patient information. | Improved communication and reduced errors. |
| Patient Care Conferences | Conferences involving patients and their families to discuss treatment options and care plans. | Increased patient satisfaction and empowerment. |
The role of neurologists in cancer care has evolved significantly over time.
Management of Brain Tumor-Related Epilepsy
Managing seizures is key in treating brain tumors. Brain tumor-related epilepsy is tough to handle. It needs a full plan for preventing seizures, picking the right drugs, and dealing with drug interactions with chemotherapy.
Seizure Prophylaxis in Brain Tumor Patients
Using drugs to prevent seizures in brain tumor patients is debated. Some studies show they might help, but others don’t. The choice to use these drugs depends on the tumor type, location, and the patient’s health.
Selection of Appropriate Antiepileptic Drugs
Choosing the right drugs for seizures in brain tumor patients is important. We look at how well the drug works, its side effects, and how it interacts with other medicines. Drugs with fewer side effects and interactions are usually better.
Managing Drug Interactions with Chemotherapy
It’s vital to manage how seizure drugs and chemotherapy interact. Some seizure drugs can change how chemotherapy works, affecting its effectiveness or safety.
| AED | Chemotherapy Interaction | Clinical Implication |
| Phenytoin | Induces metabolism of some chemotherapies | Potential reduction in chemotherapy efficacy |
| Valproate | Inhibits metabolism of some chemotherapies | Potential increase in chemotherapy toxicity |
| Levetiracetam | Fewer interactions with chemotherapy | Preferred in patients undergoing chemotherapy |
Surgical Considerations for Tumor-Related Epilepsy
In some cases, surgery might be an option for epilepsy linked to tumors. This could mean removing the tumor or the area causing seizures. A team of experts will decide if surgery is right, considering the patient’s chances and quality of life.
Addressing Neurological Complications of Brain Tumors
Brain tumors can cause serious neurological problems. These issues can really affect a person’s life quality. It’s important to manage them well.
Cognitive Dysfunction Management
Cognitive problems are common with brain tumors. They can mess with memory, attention, and how well you can make decisions. Early treatment is key to lessen these effects. Treatment options include cognitive therapy, medicine, and daily life support.
Headache and Intracranial Pressure Issues
Headaches and high pressure inside the skull are common problems. Corticosteroids help reduce swelling. Doctors also use pain relief and sometimes surgery to ease the pressure.
Motor and Sensory Deficits
Brain tumors can cause problems with movement and feeling. Physical and occupational therapy are very helpful. They help patients get back to normal and adapt to any lasting issues.
Speech and Language Disorders
Brain tumors can also affect how we speak and communicate. Speech-language pathology interventions are critical. They help improve communication and deal with problems like swallowing issues.
| Complication | Management Strategies |
| Cognitive Dysfunction | Cognitive rehabilitation, pharmacological interventions |
| Headache and Intracranial Pressure | Corticosteroids, pain management, surgical intervention |
| Motor and Sensory Deficits | Physical and occupational therapy |
| Speech and Language Disorders | Speech-language pathology interventions |
“The management of neurological complications in brain tumor patients requires a multidisciplinary approach, incorporating various specialties to address the complex needs of these patients.”
Neurological Side Effects of Cancer Treatments
Cancer treatments save lives but can also cause serious neurological side effects. These issues can come from treatments like radiation, chemotherapy, immunotherapy, and steroids.
Radiation-induced Neurotoxicity
Radiation therapy is a common cancer treatment. But it can harm the brain. This harm can show up as memory loss, brain damage, or even new tumors. How bad it gets depends on the dose, how it’s given, and how much brain is treated.
Table: Radiation-induced Neurotoxicity Effects
| Effect | Description | Timing |
| Cognitive Decline | Memory loss, attention deficits | Months to years post-treatment |
| Radiation Necrosis | Localized brain tissue death | Typically within 2 years |
| Secondary Tumors | New tumor formation | Years to decades post-treatment |
Chemotherapy-related Neuropathy
Chemotherapy is a key part of cancer treatment. It can cause nerve damage. This damage can lead to numbness, tingling, and pain in hands and feet. The risk depends on the type and amount of chemotherapy used.
Immunotherapy Neurological Complications
Immunotherapy uses the body’s immune system to fight cancer. It can cause brain and nerve problems. These can be mild, like headaches, or severe, like brain inflammation or nerve damage.
Steroid-related Neuropsychiatric Effects
Corticosteroids are used in cancer care for their anti-inflammatory effects. But they can also cause mood changes, sleep problems, and in rare cases, psychosis.
In conclusion, it’s important to understand and manage the brain and nerve problems caused by cancer treatments. By knowing these issues, doctors can help patients better and improve their care.
The Neurologist’s Role in Treatment Decision-Making
Neurologists are key in neuro-oncology, focusing on controlling tumors and improving patient well-being. They balance treatment effectiveness with keeping the patient’s quality of life high.
Balancing Tumor Control and Quality of Life
Neurologists aim to control tumors while keeping patients’ lives good. They weigh the benefits and risks of treatments carefully.
Treatment decisions depend on the patient’s health, tumor type and stage, and how it might affect their brain. Some treatments might stop tumors but could harm the brain.
Neurological Function Preservation Strategies
Keeping brain function intact is a big part of a neurologist’s job. They plan surgeries carefully, choose the right radiotherapy, and use neuroprotective agents when they can.
Here are some ways to protect brain function:
| Strategy | Description | Benefits |
| Surgical Planning | Careful planning to minimize damage to surrounding brain tissue | Reduced risk of neurological deficits |
| Radiotherapy Techniques | Use of advanced techniques such as stereotactic radiosurgery | Precise targeting of tumors with minimal damage to surrounding tissue |
| Neuroprotective Agents | Use of agents that may protect neurological function during treatment | Potential reduction in neurological side effects |
Risk-Benefit Analysis of Treatment Options
Neurologists analyze the risks and benefits of treatments. They look at how well treatments work, the chance of brain problems, and how they affect the patient’s life.
Patient Advocacy in Complex Cases
In tough cases, neurologists act as patient advocates. They make sure the patient’s wishes are heard. This means talking clearly with the patient and their family and working with other doctors.
By supporting patients and making smart treatment choices, neurologists are essential in neuro-oncology.
Multidisciplinary Tumor Board Participation
Neurologists, neurosurgeons, and radiation oncologists work together in multidisciplinary tumor boards. They aim to improve patient outcomes. This teamwork makes sure all parts of a patient’s health are considered when planning treatment.
Neurologists add important skills to these teams. They help with neurological risk assessment and managing possible complications.
Collaboration with Neurosurgeons and Radiation Oncologists
In multidisciplinary tumor boards, neurologists team up with neurosurgeons and radiation oncologists. Together, they create detailed treatment plans. This teamwork makes sure the brain’s health is considered in surgeries and treatments.
Input on Neurological Risk Assessment
Neurologists give key advice on neurological risk assessment. They help spot risks with different treatments. Their input is vital for finding ways to reduce these risks and improve patient results.
Case Presentation and Neurological Perspectives
At multidisciplinary tumor board meetings, complex cases are shared. Neurologists share their knowledge on the brain aspects of each case. This teamwork ensures treatment plans fit each patient’s unique needs.
Specialized Neuro-Oncology Care Services
Specialized neuro-oncology care has changed how we manage complex patient needs. The field of neuro-oncology keeps getting better. This makes it more important than ever to have complete and well-coordinated care.
Dedicated Neuro-Oncology Clinics
Dedicated neuro-oncology clinics are key for focused care on brain tumors and other neurological cancers. These clinics have a team of experts. They include neurologists, neurosurgeons, medical oncologists, and radiation oncologists. Together, they create treatment plans that fit each patient’s needs.
The benefits of these clinics are many:
- Comprehensive care in one place
- Easy communication among healthcare providers
- Access to the latest treatments and clinical trials
- Better patient satisfaction and results
Integrated Care Models
Integrated care models are vital in neuro-oncology. Patients often need surgery, medicine, and radiation. By working together, healthcare providers can give seamless care that meets the complex needs of neuro-oncology patients.
Key parts of integrated care models are:
- Teamwork among different specialties
- Treatment plans made just for each patient
- Continued care throughout the disease
- Support for patients and their families
Telehealth Applications in Neuro-Oncology
Telehealth is a big help in neuro-oncology care, helping patients who can’t easily get to special centers. It lets for remote consultations, follow-ups, and monitoring. This makes care more accessible and can lower costs.
Telehealth in neuro-oncology is growing. It could lead to better patient involvement, outcomes, and care efficiency.
Managing Paraneoplastic Neurological Syndromes
Understanding paraneoplastic neurological syndromes is key to caring for cancer patients. These rare disorders are linked to cancer and can harm the nervous system in many ways.
Recognition of Paraneoplastic Manifestations
Spotting paraneoplastic neurological syndromes early is vital. Doctors need to know about the many neurological symptoms they can cause. This includes encephalitis, neuropathy, and cerebellar degeneration. It’s important to be suspicious, mainly in those with cancer history or unusual neurological signs.
Diagnostic Workup and Antibody Testing
Diagnosing these syndromes involves several steps. This includes clinical checks, imaging, and lab tests. Antibody tests are also key, as they help identify the syndromes linked to specific cancers. Below is a table showing common antibodies and the syndromes they’re linked to.
| Antibody | Associated Syndrome | Cancer Type |
| Anti-Hu | Encephalomyelitis, sensory neuronopathy | Small cell lung cancer |
| Anti-Yo | Cerebellar degeneration | Ovarian, breast cancer |
| Anti-Ma2 | Limbic encephalitis | Testicular, other cancers |
Treatment Approaches for Paraneoplastic Disorders
Treating these syndromes requires a few steps. This includes treating the cancer, using immunotherapy, and managing symptoms. Early action can help some patients, but the outcome depends on the syndrome and cancer type.
Long-term Management Strategies
Managing these syndromes long-term means constant monitoring and support. This might include rehab, managing chronic symptoms, and watching for cancer return or spread.
In summary, managing paraneoplastic neurological syndromes needs a detailed and coordinated plan. This includes early detection, accurate diagnosis, and effective treatments.
Neuro-Rehabilitation in Cancer Patients
Neuro-rehabilitation is key for cancer patients to deal with neurological issues. With better cancer treatments, the need for good neuro-rehab programs has increased a lot.
Assessment of Rehabilitation Needs
It’s important to check what each patient needs for rehab. This means looking at their brain function, thinking skills, and physical abilities. This helps find out where they need help.
Coordination with Rehabilitation Specialists
Working with experts like physical and speech therapists is vital. Multidisciplinary teams make plans that fit each patient’s needs. This ensures they get the right care.
“Rehab isn’t just about getting over physical issues. It’s about helping patients be independent and live well again.”
Adaptive Strategies for Neurological Deficits
Adaptive strategies are key for dealing with brain problems from cancer. This includes brain exercises, physical activities, and speech therapy. These help patients overcome challenges.
Adding neuro-rehab to cancer care improves patient results and life quality. As said by
“Rehabilitation is a critical component of cancer care, helping patients adapt to and manage neurological deficits.”
Neurological Aspects of Palliative Care
Palliative care is key for those with advanced neurological conditions. It helps manage symptoms and improve quality of life. This care addresses the complex needs of those with serious illnesses.
Symptom Management in Advanced Disease
Managing symptoms is vital in palliative care. Neurologists work to reduce pain, seizures, and cognitive issues. This improves patient comfort and function. Symptom control comes from medicines, therapies, and lifestyle changes.
Quality of Life Considerations
Quality of life is a top priority in palliative care. Neurologists aim to keep patients independent and dignified. They address mobility, communication, and cognitive function. A team effort is needed to enhance quality of life.
End-of-Life Neurological Care
Neurological care at the end of life focuses on comfort and support. It’s important to manage symptoms like pain and agitation. Neurologists work with palliative care teams for complete end-of-life care.
Family Support and Education
Supporting families is a big part of palliative care. Neurologists educate on disease progression and symptom management. This helps families make informed decisions and cope with caregiving challenges.
| Description | Benefits | |||
| Symptom Management | Alleviating symptoms such as pain and seizures | Improved patient comfort and functionality | ||
| Quality of Life | Maintaining independence and dignity | Enhanced patient well-being | ||
| End-of-Life Care | Focusing on comfort and support | Compassionate care during the final stages | ||
Emerging Therapies and Clinical Trials in Neuro-Oncology
New treatments and clinical trials are changing neuro-oncology. Neurologists are key in these changes. They help develop and use these new methods.
Neurologist’s Role in Patient Selection
Neurologists pick the right patients for new treatments. They use their knowledge to match patients with the best treatments. This is based on the patient’s condition and health.
- Assessing neurological function and status
- Determining eligibility for specific clinical trials
- Monitoring patient response to new therapies
Monitoring Neurological Outcomes in Trials
Neurologists watch how patients do in trials. They check if new treatments work well and are safe. They make changes if needed.
Key aspects of monitoring include:
- Regular neurological examinations
- Imaging studies to assess tumor response
- Neurophysiological testing to evaluate treatment effects
Translational Research Contributions
Neurologists play a big part in research. They connect lab findings to real-world treatments. Their work finds new ways to treat and improves treatments.
“The collaboration between neurologists and researchers is essential for advancing neuro-oncology and improving patient outcomes.”
Novel Targeted Therapies with Neurological Implications
New targeted therapies are exciting in neuro-oncology. These treatments aim at specific parts of tumors. They might have fewer side effects on the brain.
As neuro-oncology grows, neurologists’ role is more important. Their skills are key to making sure new treatments are safe and work well for patients.
Special Considerations in Pediatric Neuro-Oncology
Pediatric neuro-oncology faces unique challenges because of the age of patients. Brain tumors in kids affect their growth, development, and long-term brain health.
Developmental Impact of Tumors and Treatments
Brain tumors and their treatments can change a child’s mind, emotions, and body. Neurologists must think about these impacts when treating kids. They adjust their care based on the child’s age and development.
Long-term Neurological Follow-up
Children treated for brain tumors need ongoing checks. This helps spot any late effects on their brain. It includes looking at their thinking skills, any brain problems, and side effects from treatment.
Educational and Social Support Coordination
Working with schools and social services is key for kids with brain tumors. Neurologists are important advocates for these children. They help make sure they get the right help and support.
Transition to Adult Care
When kids with brain tumors grow up, their care needs to switch to adult services. This planning ensures they keep getting the care they need. It also helps deal with any lasting effects from their treatment.
By focusing on these special needs, neurologists can give kids with brain tumors the best care. This helps improve their life quality and outcomes.
Conclusion: The Future of Neurological Care in Oncology
The role of neurologists in cancer care has evolved significantly over time.
Neurologists working with cancer teams will be key in fighting cancer’s brain effects. This teamwork helps give patients the best care possible. It makes their lives better and their treatment outcomes better too.
The role of neurologists in cancer care has evolved significantly over time.
FAQ
What is neuro-oncology, and why is it important?
Neuro-oncology is a field that focuses on cancers in the nervous system. This includes brain tumors and cancers that affect the brain. It’s important because it needs a team effort to handle complex cases well.
How do neurologists contribute to cancer care?
Neurologists are key in cancer care. They handle brain and cancer-related brain problems. They also help interpret tests and work with other teams for full care.
What are the common neurological complications of brain tumors?
Brain tumors can cause many problems. These include memory issues, seizures, headaches, and trouble with movement and speech. Neurologists work hard to manage these issues.
How are seizures managed in brain tumor patients?
Managing seizures means preventing them and choosing the right medicines. It also includes dealing with drug side effects and surgery for some cases.
What are the neurological side effects of cancer treatments?
Treatments can harm the brain and nervous system. This includes damage from radiation, nerve problems from chemotherapy, and issues from immunotherapy and steroids.
How do neurologists participate in treatment decision-making?
Neurologists help decide on treatments. They balance fighting the tumor with keeping the patient’s quality of life good. They also focus on keeping the brain and nervous system working well.
What is the role of multidisciplinary tumor boards in neuro-oncology?
Tumor boards bring together experts to discuss cases. They talk about risks and come up with treatment plans. This includes neurologists, surgeons, and radiation experts.
What are paraneoplastic neurological syndromes, and how are they managed?
These are rare disorders caused by the immune system reacting to cancer. Managing them means recognizing them, doing tests, and finding treatments. It also involves long-term care plans.
How does neuro-rehabilitation support cancer patients?
Neuro-rehabilitation helps patients by figuring out what they need. It works with other specialists and helps patients adapt to their brain and nervous system changes.
What are the neurological aspects of palliative care?
The role of neurologists in cancer care has evolved significantly over time.
What are the emerging therapies in neuro-oncology?
New treatments are being developed for brain cancers. Neurologists are key in choosing patients, tracking results, and helping research move forward.
What are the special considerations in pediatric neuro-oncology?
Kids with brain tumors need special care. This includes thinking about how the tumor and treatment might affect their development. They also need ongoing care and support as they grow up.
How can patients access specialized neuro-oncology care?
Patients can get specialized care through dedicated clinics and online services. These make it easier for them to get the help they need and improve their outcomes.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/34427324/





