Last Updated on December 1, 2025 by Bilal Hasdemir

Every year, thousands of people get diagnosed with brain tumors and other nervous system cancers. This shows how important it is to have specialized care in neuro-oncology.
The field of neuro-oncology focuses on diagnosing, treating, and managing cancers of the brain and nervous system. To become a neuro-oncologist, one needs to go through a lot of education and training.
The care for nervous system cancer is very important. It greatly affects how well a patient does and their quality of life.
Key Takeaways
- The field of neuro-oncology is key for treating brain tumors and nervous system cancers.
- To become a neuro-oncologist, one needs special education and training.
- New advances in brain tumor treatment are helping patients more.
- Caring for nervous system cancer is a complex and team effort.
- It’s vital to have neuro-oncologist education for top-notch care.
Understanding Neuro-Oncology as a Medical Specialty

Neuro-oncology is a special field that deals with brain and spinal cord cancers. It needs a deep understanding of both brain disorders and cancer treatment.
Definition and Scope of Neuro-Oncology
Neuro-oncology focuses on tumors in the brain and spinal cord. It covers both primary tumors and cancer that spreads to the brain. The field also manages side effects of cancer treatments.
This area of medicine brings together many experts. Neurologists, oncologists, and surgeons work together. They aim to give the best care to patients.
Historical Development of the Field
Neuro-oncology has grown a lot over time. New imaging, surgery, and treatments have helped a lot. In the past, treatments mainly focused on easing symptoms, not curing the disease.
New discoveries have changed neuro-oncology. Now, treatments are more effective and targeted. This shows the importance of training in both neurology and oncology.
Current Role in Modern Medicine
Today, neuro-oncology is key in fighting cancer. Specialists in this field are leading the way in cancer care. They not only treat brain tumors but also research new treatments.
Training programs in neuro-oncology are getting better. They cover medical oncology, neurology training, and the latest research. This prepares specialists to handle brain cancer’s challenges, following a clear cancer specialist pathway.
Educational Foundation: Preparing for a Neuro-Oncology Career
To become a neuro-oncologist, you need a solid education. This includes studying from undergrad to specialized training. You must understand neurology, oncology, and how cancer affects the nervous system.
Undergraduate Prerequisites
Starting your journey, you need a strong undergrad background. Focus on sciences like biology, chemistry, or physics. Your courses should include:
- Biology and biochemistry
- Chemistry and organic chemistry
- Physics and mathematics
- Psychology and neuroscience
These classes get you ready for medical school and future neuro-oncology training.
Early Clinical Exposure Opportunities
Getting early clinical experience is vital. It helps you learn patient care and cancer treatment complexities. You can:
- Volunteer at cancer centers or hospitals
- Shadow neuro-oncologists or oncologists
- Join research studies on neuro-oncology
These experiences boost your clinical skills. They also show the teamwork needed in neuro-oncology, working with neurosurgeons, radiation oncologists, and more.
Residency Training Options for Aspiring Neuro-Oncologists
For those interested in neuro-oncology, choosing the right residency training is key. Aspiring neuro-oncologists have several options, like neurology, medical oncology, and neurosurgery. Each path has its own benefits and challenges. It’s important to pick the right one to build a strong foundation in neuro-oncology.
Neurology Residency Path
A neurology residency gives a deep understanding of neurological disorders, including neuro-oncology. It trains you to diagnose and manage brain and nervous system conditions. A leading neurologist says, “Neurology residency is essential for grasping the complex relationship between the nervous system and cancer.”
Medical Oncology Residency Path
Medical oncology residency focuses on cancer treatment, including chemotherapy and immunotherapy. This path is key for understanding cancer treatment, including CNS cancers. It’s a vital part of neuro-oncology training, helping professionals manage cancer care well.
Neurosurgery Considerations
Neurosurgery is a critical part of neuro-oncology, dealing with brain tumors and other conditions through surgery. A neurosurgery residency offers hands-on experience in surgery and patient care. Neurosurgery’s complexity demands a deep understanding of both surgical and medical aspects of neuro-oncology.
Radiation Oncology Alternatives
Radiation oncology is also vital in neuro-oncology, focusing on radiation therapy for cancer treatment. While not a traditional residency path, knowing radiation oncology is essential for complete patient care.
“Radiation therapy is key in managing brain tumors, and combining it with other treatments is vital for the best patient outcomes.”
The Neuro-Oncology Pathway: From Resident to Specialist
Becoming a neuro-oncologist is a long and challenging journey. It requires a lot of hard work and determination. This path involves many educational, training, and clinical steps that help a person become a skilled specialist.
Timeline of Professional Development
The journey to becoming a neuro-oncologist takes over a decade after medical school. It starts with residency training. Here, future neuro-oncologists learn the basics and develop their clinical skills.
Residency training is a key part, lasting several years. During this time, they work under experienced doctors. They learn how to diagnose and treat patients.
Key Milestones in Training
There are important milestones on the way to becoming a neuro-oncologist. These include finishing residency, getting board certification, and sometimes doing fellowship programs.
- Completing a residency program in neurology, medical oncology, or a related field.
- Obtaining board certification, which shows a specialist’s expertise.
- Pursuing fellowship training in neuro-oncology for more advanced knowledge.
Building Clinical Competencies
Developing clinical competencies is key for a neuro-oncologist’s success. They need to know how to diagnose and treat brain and central nervous system tumors. They also have to manage symptoms and side effects.
Good communication skills are also important. Neuro-oncologists must work well with patients, families, and teams. This helps provide the best care possible.
Fellowship Training in Neuro-Oncology
Fellowship training in neuro-oncology is key for specialists in brain and spinal cord tumors. It gives them the skills to manage complex cases. This training is essential for top-notch care in this field.
Accredited Program Requirements
To become a neuro-oncologist, one needs fellowship training in an accredited program. These programs are checked to meet high standards. They offer a mix of clinical and research training.
- Clinical training in brain and spinal cord tumors
- Working with teams like neurosurgery and oncology
- Participating in clinical trials and research
Fellowship Application Process
The fellowship application process is tough and needs careful prep. You must show strong academics, clinical skills, and a passion for neuro-oncology. The application includes:
- A personal statement on your goals and interests
- Letters of recommendation from mentors
- A detailed CV of your experience
Core Clinical Rotations
Core clinical rotations are key in fellowship training. They give hands-on experience in treating brain and spinal cord tumors. Fellows learn from experts in the field.
Research Components
The research component boosts innovation in neuro-oncology. Fellows get involved in trials and research. This improves their skills and helps find new treatments.
In summary, fellowship training in neuro-oncology is vital. It prepares specialists for this complex field. With both clinical and research training, they can give the best care to patients.
Board Certification and Credentialing Process
Board certification in neuro-oncology shows a specialist’s skill in treating complex brain cancers. It’s key for credibility and top-notch patient care.
Examination Requirements
To get certified, neuro-oncologists must pass a tough exam. It checks their knowledge in neurology and oncology. The American Board of Psychiatry and Neurology (ABPN) and the American Board of Medical Oncology (ABMO) offer these certifications.
“Certification is not just about passing an exam; it’s about demonstrating a commitment to excellence in patient care.” –
A leader in the field of neuro-oncology
- Neurology and oncology knowledge assessment
- Clinical skills evaluation
- Understanding of current treatment guidelines
Maintenance of Certification
To keep certification, neuro-oncologists must keep learning. They need to stay current with new discoveries in their field. This involves attending conferences and taking courses.
Activity | Description | Frequency |
Continuing Medical Education (CME) | Participate in CME courses related to neuro-oncology | Annual |
Professional Conferences | Attend conferences such as the Society for Neuro-Oncology annual meeting | Annual |
Peer Review | Engage in peer review of clinical cases or research articles | Bi-annual |
Additional Specialized Certifications
Neuro-oncologists can also get extra certifications. These show they’re experts in areas like neuro-imaging or pain management.
Getting and keeping board certification shows neuro-oncologists’ dedication to their patients. It boosts their reputation and helps the field grow.
Clinical Practice Areas in Neuro-Oncology
Neuro-oncology deals with many areas, like primary brain tumors and cancer-related brain issues. Doctors in this field handle a wide range of conditions. They care for patients with common brain tumors and complex diseases.
Primary Brain Tumors
Primary brain tumors are a big part of neuro-oncology. These tumors can be harmless or very dangerous. Gliomas, like glioblastoma, are among the toughest to treat.
Doctors use MRI and biopsies to diagnose these tumors. Treatment plans vary, using surgery, radiation, and chemotherapy.
Metastatic Disease to the CNS
Metastatic disease in the brain is another key area. It often comes from cancers like lung or breast. Doctors use a team effort to treat it, with radiation, surgery, and medicine.
The treatment depends on the tumor’s size and location. It also looks at the patient’s overall health.
Neurological Complications of Cancer
Cancer and its treatment can cause brain problems. These include nerve damage, seizures, and memory loss. Neuro-oncologists help manage these issues to improve patients’ lives.
They use medicines, therapy, and support to help patients. This makes a big difference in their quality of life.
Supportive Care in Neuro-Oncology
Supportive care is a big part of neuro-oncology. It focuses on easing symptoms and improving life quality. This includes mental, social, and spiritual support.
Neuro-oncologists work with a team to offer this care. They team up with palliative care specialists for a full support plan.
In conclusion, neuro-oncology is a complex field. It requires a lot of knowledge and teamwork. By understanding these challenges, doctors can give the best care to their patients.
Multidisciplinary Approach to Brain Tumor Management
Brain tumors are complex and need a team effort from healthcare experts. A good plan for managing brain tumors involves many medical fields working together. This ensures the best care for patients.
Collaboration with Neurosurgery
Neurosurgery is vital in treating brain tumors, mainly through surgery. Neuro-oncologists and neurosurgeons must work together. They decide the best surgery and plan for after the operation.
Working with Radiation Oncology
Radiation oncology is also key in treating brain tumors, often with radiation therapy. Neuro-oncologists and radiation oncologists team up. They create plans that fight the tumor well but protect the brain.
Treatment Modalities in Modern Neuro-Oncology
Today, neuro-oncology uses many treatment methods to help patients with brain tumors. These methods are needed because brain cancers are complex. They combine different treatments to get the best results.
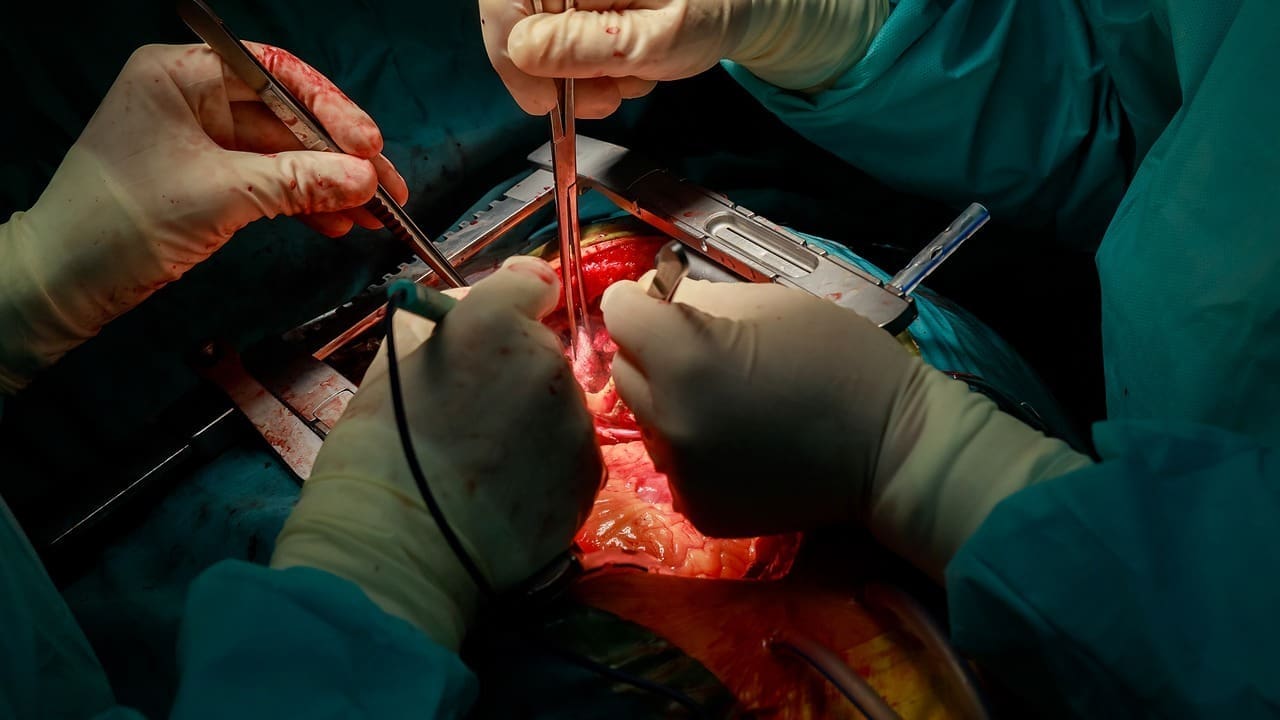
Surgical Interventions
Surgery is key in treating brain tumors. New techniques like awake craniotomy and intraoperative MRI make surgery safer and more precise. The goal is to remove as much tumor as possible without harming the brain.
Radiation Therapy Approaches
Radiation therapy is also vital in treating brain tumors. It uses different methods based on the tumor’s type and location. Stereotactic radiosurgery (SRS) and fractionated stereotactic radiotherapy aim to target tumors accurately, protecting the brain.
Systemic Therapies and Chemotherapy
Chemotherapy and targeted therapy are important in treating brain tumors. New drugs can cross the blood-brain barrier, making chemotherapy more effective. Researchers are working on new targets and treatments.
Emerging Treatments and Clinical Trials
New treatments are being developed in neuro-oncology. Immunotherapy and precision medicine are being tested in trials. These include vaccines and gene therapy, showing great promise.
Using all these treatments requires a team effort. Neurosurgeons, radiation oncologists, and medical oncologists work together. This teamwork helps create personalized treatment plans for better patient outcomes.
Personalized Treatment Plans for Brain Cancer Patients
The move towards personalized treatment in neuro-oncology is changing how we care for patients. Tailoring treatments to each patient’s needs can greatly improve brain cancer care.
Tumor Genetics Testing
Tumor genetics testing is key in making personalized plans. It helps doctors understand a tumor’s genetic makeup. This lets them pick treatments that are more likely to work.
Genetic testing finds mutations in genes like IDH1 or IDH2 in brain tumors. Patients with these mutations might do well with targeted therapies that block the mutated gene.
Biomarker-Driven Therapy Selection
Biomarkers are important in choosing treatments. They show how well a patient might do with a certain treatment. This way, doctors can pick the best therapy for each patient.
- MGMT promoter methylation status can predict response to certain chemotherapies.
- IDH mutations can make tumors more susceptible to specific targeted therapies.
- 1p/19q codeletion status can influence the decision to use chemotherapy or radiation therapy.
Patient-Specific Considerations
Every patient’s situation is unique. Their health, age, and what they prefer should be considered. This ensures the treatment is both effective and easy to handle.
Patient-centered care looks at the whole person, not just the tumor. It aims to improve the patient’s life and meet their needs. This approach makes treatment plans fit each person’s life better.
Research Opportunities in Neuro-Oncology
Neuro-oncology research is key to better patient care. It’s moving fast, thanks to new ideas in basic science, clinical trials, and how we apply research to patients.
Advancing Basic Science
Basic science in neuro-oncology aims to understand brain tumors at a molecular and genetic level. This research is essential for finding new treatments. Studies show that knowing what genetic changes cause tumors can lead to better treatments.
Clinical Trial Development
Clinical trials are vital for turning research into real treatments. They test new treatments, like special drugs and therapies, to see if they work and are safe.
The process of clinical trial development involves:
- Identifying promising therapeutic agents
- Designing trials to assess safety and efficacy
- Collaborating with multi-disciplinary teams
Securing Funding and Grant Writing
Funding is essential for neuro-oncology research. Getting grants and writing strong proposals are important skills for researchers.
Effective grant writing involves:
Strategy | Description |
Clearly defining research objectives | Outlining the goals and significance of the research |
Demonstrating the potential impact | Showing how the research will advance the field |
By tapping into these research opportunities, neuro-oncologists can keep improving the field and helping patients.
Career Settings for Neuro-Oncologists
Neuro-oncologists have many career options. They can work in academic medical centers, industry roles, or private practice. This variety lets them pick a path that fits their interests and goals.
Academic Medical Centers
Academic medical centers mix clinical work, research, and teaching. Neuro-oncologists here treat complex cases, run clinical trials, and teach. They use the latest technology and work with experts from different fields.
Key Responsibilities:
- Clinical practice and patient care
- Research and clinical trials
- Teaching and mentoring students and residents
Comprehensive Cancer Centers
Comprehensive cancer centers focus on treating cancer patients. Neuro-oncologists in these centers work with neurosurgeons, radiation oncologists, and others. They help plan treatments for brain tumors and other cancers.
Center Type | Key Features | Neuro-Oncologist’s Role |
Academic Medical Centers | Research, education, complex patient care | Clinical practice, research, teaching |
Comprehensive Cancer Centers | Multidisciplinary care, treatment planning | Part of a multidisciplinary team, treatment planning |
Private Practice Opportunities
Private practice lets neuro-oncologists work on their own terms. They can choose their schedule and how to care for patients. They might work alone or with others.
Benefits of Private Practice:
- Autonomy in patient care decisions
- Potential for greater financial rewards
- Flexibility in scheduling
Industry and Pharmaceutical Roles
Neuro-oncologists can also work in industry and pharmaceuticals. They help develop new treatments and therapies. Their knowledge is key in drug development and clinical trials.
Knowing the different career paths helps neuro-oncologists choose the best fit. They can pick a setting that matches their skills and goals.
Professional Organizations and Networking
Neuro-oncologists gain a lot from joining professional groups. These groups offer chances to network, learn, and advocate. They are key in moving the field of neuro-oncology forward and supporting its doctors.
Society for Neuro-Oncology
The Society for Neuro-Oncology focuses on brain tumors and CNS cancers. Being a member gives you access to conferences, educational materials, and chances to meet other experts.
American Academy of Neurology Resources
The American Academy of Neurology (AAN) has lots for neurologists, including those in neuro-oncology. You can find educational programs, guidelines, and ways to make a difference.
International Collaborations
Working together across countries is key in neuro-oncology. It helps share knowledge and best practices. This leads to bigger, more varied clinical trials and global care standards.
By joining these organizations, neuro-oncologists can grow their skills, meet new people, and help their field advance.
Conclusion: The Rewarding Journey of a Neuro-Oncologist
Starting a career in neuro-oncology is tough but very rewarding. It takes a lot of dedication and a strong desire to help patients. You need to understand how to treat brain tumors and care for nervous system cancers well.
Working in neuro-oncology lets you change lives for the better. You help patients and their families dealing with brain and spinal cord tumors. You work with a team to create treatment plans that fit each patient’s needs.
Being a neuro-oncologist means always learning and growing. You must keep up with new research and treatments. This helps improve care for patients and grows the field of neuro-oncology.
If you’re interested in this field, it can be very rewarding. You get to use new treatments and help people with complex brain conditions. It’s a chance to make a big difference in someone’s life.
FAQ
What is neuro-oncology, and what does it entail?
Neuro-oncology is a medical field that deals with brain, spine, and nervous system tumors. It combines neurology, oncology, and neurosurgery for patient care. This approach ensures a complete treatment plan.
What are the educational requirements for becoming a neuro-oncologist?
To be a neuro-oncologist, you need a bachelor’s degree and medical school. Then, complete a residency in neurology, oncology, or neurosurgery. A fellowship in neuro-oncology is also recommended.
What is the role of a tumor board in brain tumor management?
A tumor board is a team of experts who plan treatment for patients. They include neurosurgeons, oncologists, and radiologists. This team ensures patients get the best care.
What are the different treatment modalities used in neuro-oncology?
Neuro-oncology uses surgery, radiation, chemotherapy, and new treatments. The choice depends on the tumor type, location, and the patient’s health.
How important is personalized treatment planning in brain cancer management?
Personalized planning is key in brain cancer treatment. It considers the patient’s needs and tumor specifics. This approach uses genetics and biomarkers for better results.
What are the career settings available to neuro-oncologists?
Neuro-oncologists work in hospitals, cancer centers, private practices, and industry. Each setting offers different opportunities and challenges. The choice depends on personal goals.
What is the significance of research in neuro-oncology?
Research is vital in neuro-oncology. It advances diagnosis, treatment, and care. It includes basic science, clinical trials, and funding.
How can neuro-oncologists stay current with the latest developments in their field?
Neuro-oncologists stay updated through professional organizations and continuing education. Attending conferences and collaborating with peers helps too.
What are the benefits of a multidisciplinary approach in brain tumor management?
A multidisciplinary approach ensures complete care from experts. It improves outcomes by fostering collaboration and communication.
What is the role of neuro-oncology fellowship training?
Fellowship training offers advanced education in brain and spinal cord tumors. It prepares neuro-oncologists and enhances their skills.
How does board certification impact a neuro-oncologist’s career?
Board certification shows expertise and commitment. It involves passing an exam and ongoing education to maintain certification.
References
New England Journal of Medicine. Evidence-Based Medical Insight. Retrieved from https://www.nejm.org/doi/full/10.1056/NEJMra0708126