Last Updated on December 1, 2025 by Bilal Hasdemir
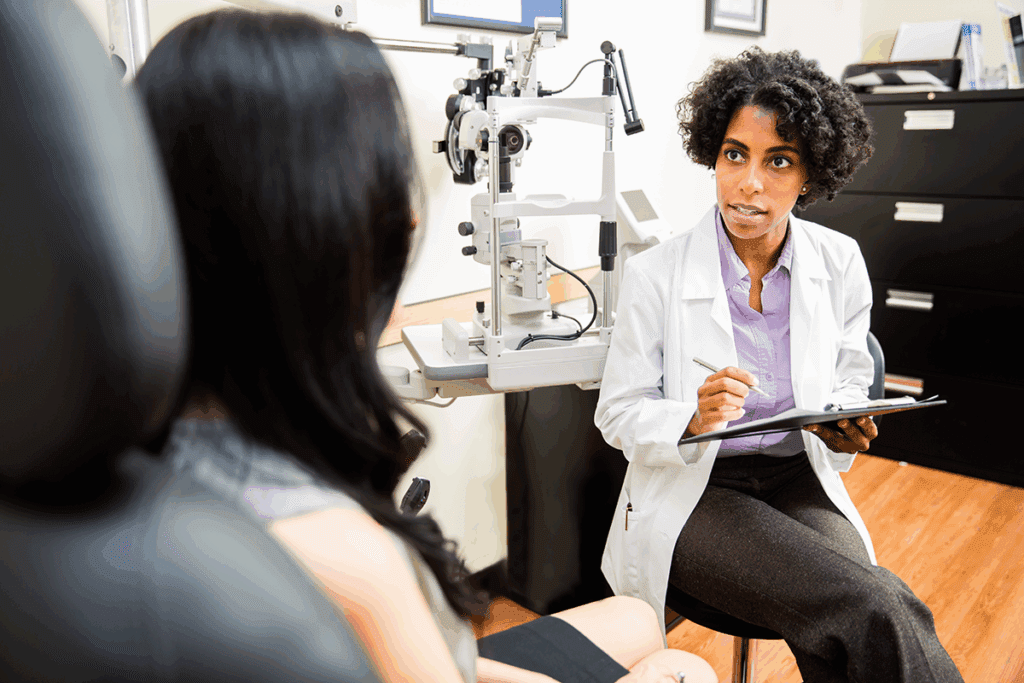
A neuro-ophthalmologist is a medical expert who focuses on eye and brain disorders. Did you know vision problems can signal deeper brain issues? This link between the eye and brain is key to solving many vision problems. What does a Neuro-ophthalmologist treat? Our amazing, critical guide covers vision loss, double vision, and other brain-related eye issues.
The field of neuro-ophthalmology is essential for eye health. It explores how the brain and eyes work together. A vision specialist in this field can diagnose and treat vision issues.
Key Takeaways
- A neuro-ophthalmologist diagnoses and treats disorders related to the eye and brain.
- The field of neuro-ophthalmology is vital in understanding the complex eye and brain connection.
- Vision problems can be a symptom of underlying neurological conditions.
- A vision specialist with expertise in neuro-ophthalmology can help manage vision health.
- Neuro-ophthalmology addresses the complex relationships between the visual pathway and the brain.
The Role of a Neuro-Ophthalmologist in Eye Care
Neuro-ophthalmologists play a key role in eye care. They diagnose and treat eye and brain disorders. Their expertise is vital for complex cases needing both neurology and ophthalmology knowledge.
Definition and Specialization Focus
Neuro-ophthalmologists are doctors trained in neurology and ophthalmology. They can handle visual problems from the eye to the brain. They focus on patients with vision issues due to stroke, multiple sclerosis, or brain tumors.
These specialists are more than eye doctors. They are vision specialists who understand the eye and nervous system connection. Their skills are essential for eye symptoms linked to neurological conditions.
The Intersection of Neurology and Ophthalmology
Neuro-ophthalmology combines neurology and ophthalmology. It offers complete care for complex visual disorders. This blend is vital because many eye issues have neurological roots, and vice versa.
| Condition | Neurological Aspect | Ophthalmological Aspect |
| Optic Neuritis | Inflammation of the optic nerve, often associated with multiple sclerosis | Vision loss, pain on eye movement |
| Ischemic Optic Neuropathy | Reduced blood flow to the optic nerve, linked to vascular risk factors | Sudden vision loss, often irreversible |
| Cranial Nerve Palsies | Paralysis of cranial nerves controlling eye movement, potentially due to diabetes, aneurysm, or tumor | Double vision, strabismus |
Understanding the connection between eye and brain conditions is essential. Neuro-ophthalmologists use this knowledge to manage complex cases. This helps in providing effective care.
Neuro-ophthalmologists bring together neurology and ophthalmology strengths. They offer a unique perspective on treating complex visual disorders. Their work shows the value of a team approach in eye care, highlighting the need for collaboration among specialties.
Educational Path and Training Requirements
To become a neuro-ophthalmologist, one must go through medical education and specialized training. This journey is long and challenging. It prepares future neuro-ophthalmologists to handle complex eye and brain conditions.
Medical Education and Residency
The first step is medical education, which takes four years to get an MD or DO degree. Students learn about human body functions and diseases. Then, they must do residency in neurology or ophthalmology.
This residency, lasting three to seven years, gives them practical experience. It deepens their knowledge in their chosen field.
Fellowship and Specialized Training
After residency, they enter fellowship programs in neuro-ophthalmology. These programs last one to two years. They focus on advanced training in complex eye and brain disorders.
Fellows work with experienced doctors. They learn to interpret tests, manage patient care, and do research. This training is key to becoming an expert in this field.
After finishing their fellowship, neuro-ophthalmologists are ready to care for patients with complex conditions. They can also contribute to research and education. This helps improve treatments for these disorders.
The Eye-Brain Connection: Foundation of Neuro-Ophthalmology
Neuro-ophthalmology studies how the eyes and brain work together. This connection is key to understanding how we see the world. It shows how light turns into what we see.
Visual Pathway Anatomy
The visual pathway is a complex system. It includes the eyes, optic nerves, and more. Each part is important for sending visual information to the brain.
The eyes start by catching light and turning it into signals. These signals then travel to the brain through the optic nerves. The optic chiasm is where the nerves cross over, combining information from both eyes.
How the Brain Processes Visual Information
The brain processes visual information in stages. The visual cortex first gets raw data from the eyes. Then, different brain areas work together to understand what we see.
This process is not just in the visual cortex. It involves a network of brain areas. Knowing this helps doctors diagnose and treat vision problems caused by neurological issues.
Common Optic Nerve Disorders Treated
It’s key to know about optic nerve disorders for good care in neuro-ophthalmology. The optic nerve is vital for our sight. Problems here can cause big vision issues.
Optic Neuritis
Optic neuritis is when the optic nerve gets inflamed. It can hurt and make vision worse. It’s often linked to multiple sclerosis, a disease of the brain and spinal cord. Doctors use corticosteroids to fight the inflammation.
Ischemic Optic Neuropathy
Ischemic optic neuropathy happens when the optic nerve doesn’t get enough blood. This leads to vision loss. It’s more common in older people and those at risk for heart disease. Doctors work to fix the blood flow issues.
Optic Nerve Compression
Optic nerve compression is when something presses on the optic nerve. This can cause vision to get worse over time. It might be due to tumors, aneurysms, or thyroid eye disease. Treatment depends on what’s causing it and might include surgery.
Understanding the optic nerve is vital for diagnosing and treating these issues. Neuro-ophthalmologists are key in managing these problems.
| Condition | Causes | Symptoms | Treatment |
| Optic Neuritis | Inflammation, often associated with multiple sclerosis | Pain, vision loss | Corticosteroids |
| Ischemic Optic Neuropathy | Insufficient blood flow, vascular risk factors | Vision loss | Managing vascular conditions |
| Optic Nerve Compression | Tumors, aneurysms, thyroid eye disease | Progressive vision loss | Surgery or other interventions based on cause |
Quick diagnosis and right treatment are key to handling optic nerve disorders. This helps avoid permanent vision loss.
Eye Movement Disorders in Neuro-Ophthalmology
Neuro-ophthalmology deals with many eye movement disorders. These need careful diagnosis and treatment. They can really affect a person’s life, making everyday tasks hard.
Eye movement disorders are complex. They involve many nerves and brain areas working together. Knowing about these disorders is key to managing them well.
Diplopia (Double Vision) Causes and Evaluation
Diplopia, or double vision, is a common issue. It happens when the eyes can’t line up right. This makes you see two images instead of one.
There are many reasons for diplopia. These include nerve problems, thyroid issues, and myasthenia gravis. Finding the cause is important.
Nystagmus and Other Abnormal Eye Movements
Nystagmus is when your eyes move on their own. It can start at birth or come on later due to brain issues.
Other eye movements like saccadic intrusions and opsoclonus can also show up. These might mean there’s a problem like multiple sclerosis or a brainstem issue.
Cranial Nerve Palsies Affecting Eye Movement
Cranial nerve palsies can really mess with eye movement. This is true for nerves like the oculomotor, trochlear, and abducens.
It’s important to figure out which nerve is affected. Then, you can plan the right treatment.
| Cranial Nerve | Function | Effect of Palsy |
| Oculomotor (III) | Controls most eye movements, eyelid opening | Ptosis, limited eye movement |
| Trochlear (IV) | Controls superior oblique muscle | Vertical diplopia |
| Abducens (VI) | Controls lateral rectus muscle | Horizontal diplopia, limited abduction |
Neuro-ophthalmologists need to understand eye movement disorders well. By treating these conditions right, patients can see big improvements in their lives.
Visual Field Defects and Their Neurological Origins
The visual pathway is complex. Defects in the visual field can come from many neurological sources. Visual field defects mean losing part or all of your normal vision. They can be caused by problems in the eye, optic nerve, or brain.
Types of Visual Field Loss
Visual field loss shows up in different ways. Each type gives clues about what might be wrong. Here are some common ones:
- Homonymous hemianopia: Half of your vision is lost on the same side in both eyes.
- Bitemporal hemianopia: You lose the outer half of your vision in both eyes. This is often due to a problem at the optic chiasm.
- Quadrantanopia: You lose a quarter of your vision, either the top or bottom part.
Diagnostic Significance of Field Patterns
The pattern of visual field loss helps doctors figure out what’s wrong. For example, homonymous hemianopia might mean there’s a problem after the optic chiasm. This could be in the optic tract, lateral geniculate nucleus, or visual cortex.
Bitemporal hemianopia usually means there’s a problem at the optic chiasm. This could be a tumor pressing on it.
Knowing how to read visual field defect patterns helps neuro-ophthalmologists find where the problem is. They use advanced tests like MRI to find the cause.
Pupil Abnormalities and Neurological Implications
Abnormalities in pupil size or reactivity can signal serious neurological conditions. Pupils are not just simple apertures that regulate light entry into the eye; their function is closely linked to the brain’s neurological status.
Anisocoria and Pupillary Light Reflex Disorders
Anisocoria refers to the condition where the pupils are of unequal sizes. This can be a benign condition, but it can also be indicative of serious neurological disorders. The pupillary light reflex, which controls the constriction and dilation of pupils in response to light, is a critical diagnostic tool. Disorders in this reflex can indicate issues such as third cranial nerve palsy or sympathetic pathway damage.
Evaluation of anisocoria involves assessing the pupillary light reflex and considering other symptoms such as ptosis (drooping eyelid) or extraocular muscle weakness. Diagnosing the cause of anisocoria requires a thorough neurological examination.
Horner’s Syndrome and Other Pupillary Conditions
Horner’s Syndrome is characterized by a triad of miosis (pupil constriction), ptosis, and anhidrosis (lack of sweating) on one side of the face. It results from disruption of the sympathetic nerves supplying the eye. Other pupillary conditions include Adie’s tonic pupil, where the pupil reacts slowly to light, and Argyll Robertson pupil, which accommodates but doesn’t react to light.
| Pupillary Condition | Characteristics | Neurological Implication |
| Anisocoria | Unequal pupil sizes | May indicate third cranial nerve palsy or sympathetic pathway damage |
| Horner’s Syndrome | Miosis, ptosis, anhidrosis | Disruption of sympathetic nerves |
| Adie’s Tonic Pupil | Slow reaction to light | Denervation of the ciliary ganglion |
Understanding these pupil abnormalities is key to diagnosing and managing neurological conditions. A detailed neuro-ophthalmological examination is vital for accurate diagnosis and treatment planning.
Headache Evaluation in Neuro-Ophthalmology
Headaches are a big deal in neuro-ophthalmology because they can point to vision problems. They can be caused by many things, like migraines or too much pressure inside the skull. So, it’s important to check them out carefully.
Migraine-Related Visual Disturbances
Migraines often lead to headaches and can cause weird vision stuff, like zigzag patterns or flashes. Migraine-related visual disturbances are usually short-lived but can really scare people.
“Migraine is a neurological condition that can cause a range of symptoms, including headache, nausea, and visual disturbances,” as noted by headache specialists. Knowing about these visual symptoms helps doctors diagnose and treat migraines better.
Papilledema and Increased Intracranial Pressure
Papilledema is when the optic disc swells, often due to too much pressure inside the skull. This can happen for many reasons, like tumors or other brain issues. Increased intracranial pressure is serious and needs quick action to avoid vision problems.
If papilledema is found, doctors will do tests like scans and maybe a lumbar puncture. This helps figure out why it’s happening and how to fix it. Timely diagnosis is key to saving vision.
- Headache characteristics can provide clues to the underlying cause.
- Visual disturbances associated with migraines are typically transient.
- Papilledema is a sign of potentially increased intracranial pressure.
In conclusion, checking headaches in neuro-ophthalmology is complex. It involves looking at things like migraine vision problems and signs of too much pressure inside the skull. By understanding these, doctors can give the right care and help patients manage their conditions.
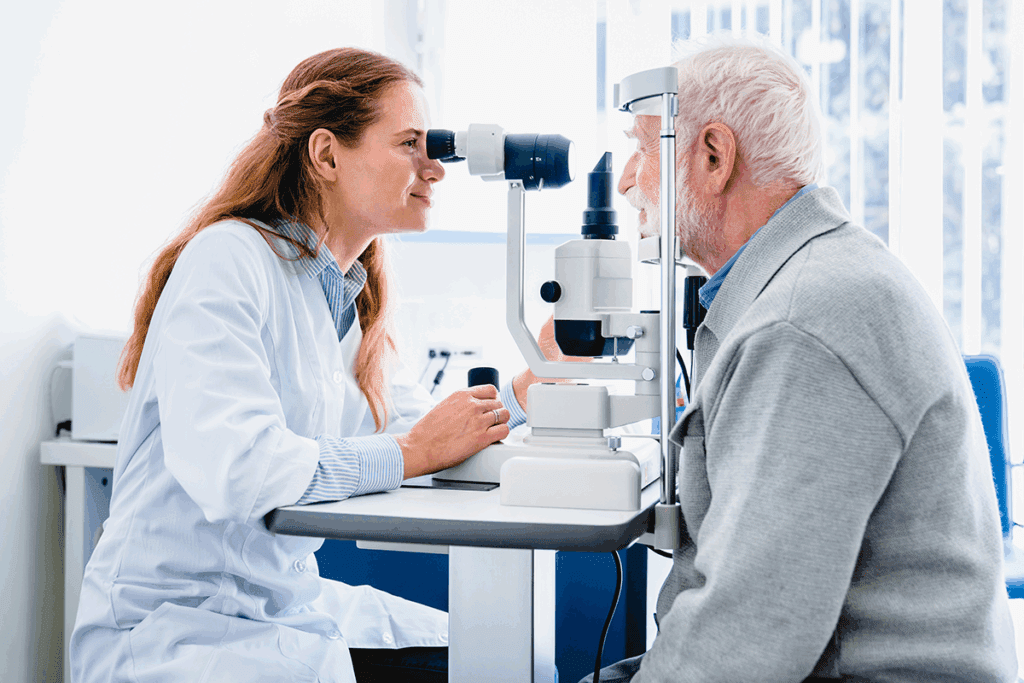
Diagnostic Procedures Used by Neuro-Ophthalmologists
Diagnosing neuro-ophthalmic conditions needs a detailed approach. Neuro-ophthalmologists use many tools to check patients with complex eye issues.
Comprehensive Neuro-Ophthalmic Examination
A detailed neuro-ophthalmic exam is key. It checks visual acuity, fields, and how the eyes move. It also looks at the pupils, eyelids, and orbits.
Key components include looking at the patient’s medical history. A detailed eye check and cranial nerve function tests are also done.
Advanced Imaging Techniques
Advanced imaging is vital for diagnosing. Magnetic Resonance Imaging (MRI) and Computed Tomography (CT) scans are used. They show the brain and orbit’s structure.
Specialized Diagnostic Tests
Special tests are needed for certain conditions. These include visual field tests, OCT, and VEP. They help understand the visual pathway’s function.
Visual field testing is great for spotting and tracking field issues. OCT checks the retinal nerve layer’s thickness. It helps diagnose optic neuritis.
Neurological Conditions Affecting Vision
The link between neurological conditions and vision is complex. Many neurological disorders can harm vision, causing different problems. It’s key to know these conditions to offer the right care.
Stroke-Related Vision Issues
A stroke can lead to vision issues, depending on the brain area hit. Visual field defects are common, causing vision loss on one side. Damage can also cause double vision, as the brain struggles to move eyes together.
Multiple Sclerosis and Vision
Multiple sclerosis (MS) affects the central nervous system, including the optic nerve. Optic neuritis, inflammation of the optic nerve, is a common symptom. It causes vision loss and pain when moving the eyes.
- MS can lead to blurred vision, double vision, and vision loss.
- Regular eye exams are vital for MS patients to track vision changes.
Neurodegenerative Diseases and Visual Changes
Neurodegenerative diseases like Alzheimer’s and Parkinson’s can cause visual issues. These include trouble processing visual info, eye movement problems, and perception issues.
| Disease | Common Visual Symptoms |
| Alzheimer’s | Visual processing difficulties, hallucinations |
| Parkinson’s | Double vision, difficulty with eye movements |
Knowing the visual symptoms of neurological conditions is key for diagnosis and care. Regular visits to a neuro-ophthalmologist can help manage these vision problems.
Treatment Approaches in Neuro-Ophthalmology
Managing neuro-ophthalmic disorders needs a detailed plan. These conditions mix neurological and ophthalmological aspects. So, a treatment plan must fit each patient’s unique needs.
Medical Interventions
Medical treatments are key for neuro-ophthalmic conditions. They include using corticosteroids to lessen inflammation in optic neuritis. Medications also help manage symptoms in multiple sclerosis and other diseases.
For example, corticosteroids can help in acute optic neuritis. This might improve vision. Immunosuppressive or immunomodulatory therapies are used for autoimmune conditions affecting the visual pathway. The right medication and treatment plan depend on the condition, its severity, and the patient’s health.
Surgical Options
Surgery is needed for some neuro-ophthalmic conditions. For instance, decompression surgery relieves pressure on the optic nerve from tumors or other lesions. Surgery is also considered for severe or complicated cases of thyroid eye disease.
New surgical techniques, like minimally invasive procedures, have better outcomes. Deciding on surgery involves weighing benefits and risks. It also considers other treatment options.
Vision Rehabilitation Strategies
Vision rehabilitation is vital for patients with neuro-ophthalmic disorders. It helps them use their vision to the fullest and adapt to any impairments. This includes using low vision aids and learning adaptive techniques for daily tasks.
Rehabilitation programs are customized for each patient. They may include occupational therapy, mobility training, and counseling. The aim is to improve the patient’s quality of life and independence.
When to Seek a Neuro-Ophthalmology Consultation
Seeing a neuro-ophthalmologist is key for diagnosing and treating eye and brain issues. This care is vital for complex vision problems. It’s not just for general eye or brain doctors.
Warning Signs and Symptoms
Some symptoms mean you should see a neuro-ophthalmologist. These include:
- Sudden vision loss or double vision
- Severe eye pain or headache
- Unusual pupil reactions or irregularities
- Visual disturbances linked to migraines or other brain issues
Spotting these signs early is important. For example, sudden vision loss might be a sign of a serious issue. It could be optic neuritis or ischemic optic neuropathy, needing quick medical help.
Referral Process from Other Specialists
The first step is usually a visit to a primary care doctor or an eye specialist. If they can’t handle it, they’ll send you to a neuro-ophthalmologist. Here’s how it usually works:
| Initial Specialist | Reason for Referral | Typical Symptoms |
| Primary Care Physician | Unexplained vision problems | Blurred vision, double vision |
| Ophthalmologist | Complex eye disorders | Severe eye pain, vision loss |
| Neurologist | Neurological conditions affecting vision | Migraine-related visual disturbances, optic neuritis |
Knowing how referrals work can help you get the right care. It makes navigating the healthcare system easier.
Conclusion
Neuro-ophthalmology is key in linking the eye and brain. It helps with complex vision and brain issues. Knowing about neuro-ophthalmologists and their work shows how important they are for eye health.
Managing vision problems linked to the brain needs a detailed plan. This includes new tests and treatments made just for each person. As neuro-ophthalmology grows, it will keep being a big part of health care. It helps people keep their vision and stay healthy.
If you have vision issues or think you might have a brain problem, see an eye specialist or neuro-ophthalmologist. They can give you the right diagnosis and treatment. This can really improve your life.
FAQ
What is neuro-ophthalmology, and why is it important?
Neuro-ophthalmology is a field that combines neurology and ophthalmology. It helps diagnose and treat eye and brain conditions. It’s key in understanding how the eye and brain work together, which is important when vision problems are linked to brain issues.
What kind of training does a neuro-ophthalmologist receive?
Neuro-ophthalmologists get a lot of education and training. They do residency in either neurology or ophthalmology. Then, they get specialized training through fellowship programs.
What are some common conditions treated by neuro-ophthalmologists?
They treat many conditions, like optic neuritis and ischemic optic neuropathy. They also handle optic nerve compression, diplopia, nystagmus, and cranial nerve palsies.
How do neuro-ophthalmologists diagnose conditions?
They use many diagnostic tools. This includes detailed exams, MRI and CT scans, and special tests.
What is the significance of visual field defects in neuro-ophthalmology?
Visual field defects can show problems in the visual pathway. Neuro-ophthalmologists need to understand this to diagnose and manage conditions.
Can pupil abnormalities be indicative of neurological conditions?
Yes, issues like anisocoria and Horner’s Syndrome can point to neurological problems. They need careful evaluation.
How are headaches evaluated in neuro-ophthalmology?
Headaches can signal neuro-ophthalmic conditions like migraines or increased intracranial pressure. It’s important to evaluate them for diagnosis and treatment.
What are some neurological conditions that can affect vision?
Many conditions can harm vision, including stroke, multiple sclerosis, brain tumors, and neurodegenerative diseases.
What treatment approaches are used in neuro-ophthalmology?
Treatments vary based on the condition. They include medical treatments, surgery, and vision rehabilitation strategies.
When should someone seek a neuro-ophthalmology consultation?
Seek a consultation for sudden vision loss or double vision. Knowing how to get a referral from other specialists is also important for full care.