Last Updated on December 1, 2025 by Bilal Hasdemir

Did you know that millions worldwide suffer from neurological conditions like stroke and traumatic brain injury? These conditions often need immediate, specialized care. Our comprehensive support helps patients with critical neurological conditions. We aim to improve their outcomes through our neurocritical care teams.neurocritical care functionsArteriovenous Malformation Brain Surgery: 7 Key Steps in AVM Removal and Recovery
Our teams offer specialized medical support. We use the latest in critical care of neurological patients to help them recover. By understanding neuro icu roles and neuro icu management, we can give targeted care. This care makes a big difference in how well patients recover.
Key Takeaways
- Neurocritical care teams provide specialized medical support for patients with critical neurological conditions.
- Comprehensive neurocritical care functions optimize patient outcomes.
- Neuro ICU roles are key in managing critical neurological patients.
- Effective neuro ICU management is vital for better patient recovery.
- Our teams use the latest advancements in critical care to support patients.
The Scope and Purpose of Neurocritical Care
Neurocritical care is where neurology and critical care meet. It offers special treatment for serious brain issues. This field has grown to meet the needs of patients with severe brain injuries and other urgent neurological problems.
This field relies on advanced medical knowledge and technology. It helps healthcare experts give the best care to patients with severe neurological illnesses. We will look at how this field started, its growth, and why it’s so important for treating things like traumatic brain injury and stroke.
History and Evolution of Neurocritical Care
Neurocritical care began in early intensive care units (ICUs). There, critical care specialists saw the need for focused neurological care. With new medical tech and a better understanding of brain conditions, this specialty has grown.
The history of neurocritical care is filled with key moments. These include:
- The creation of dedicated neuro ICUs
- Improvements in monitoring intracranial pressure
- Development of special treatment plans for stroke and traumatic brain injury
The Need for Specialized Neurological Critical Care
Handling emergencies like traumatic brain injury and stroke needs special care. Monitoring intracranial pressure is key. It helps manage patients at risk of getting worse.
There are many reasons why specialized care is needed:
- Complex brain conditions need careful handling.
- Tools like intracranial pressure monitoring are vital for patient care.
- A team approach ensures each patient gets a treatment plan that fits their needs.
With specialized care, we can greatly improve outcomes for patients with severe brain injuries. The teamwork between intensivists, neurosurgeons, and others is essential. It helps make decisions, like starting intracranial pressure monitoring, to give the best care.
Essential Neurocritical Care Functions in Modern Medicine
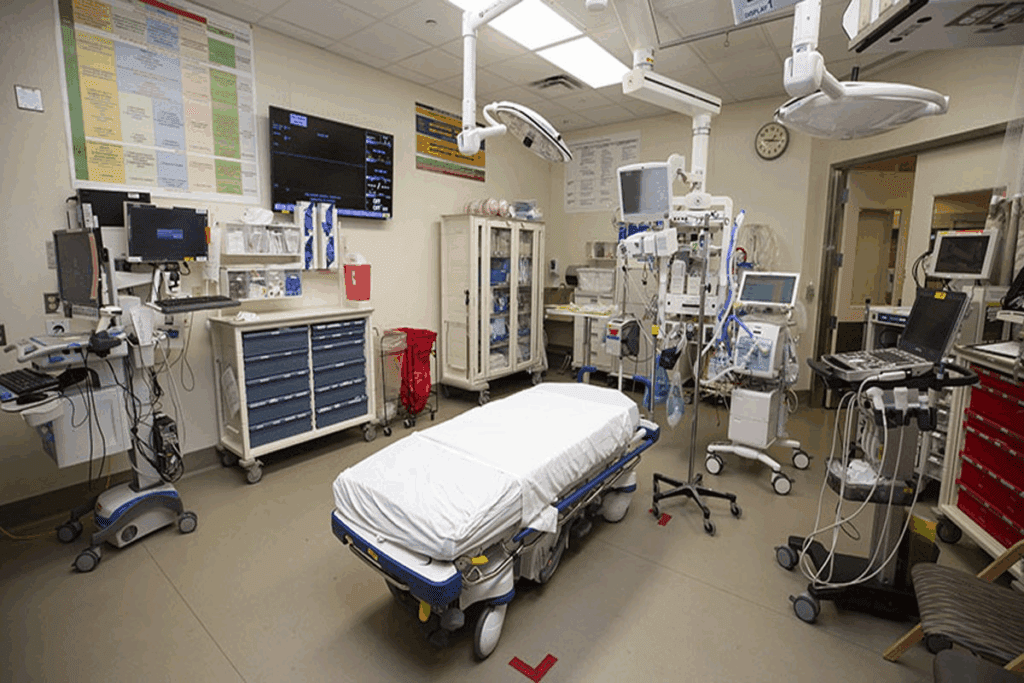
In today’s medicine, neurocritical care is key for complex brain cases. We give special care to those with severe brain issues. We use the latest medical tools and methods.
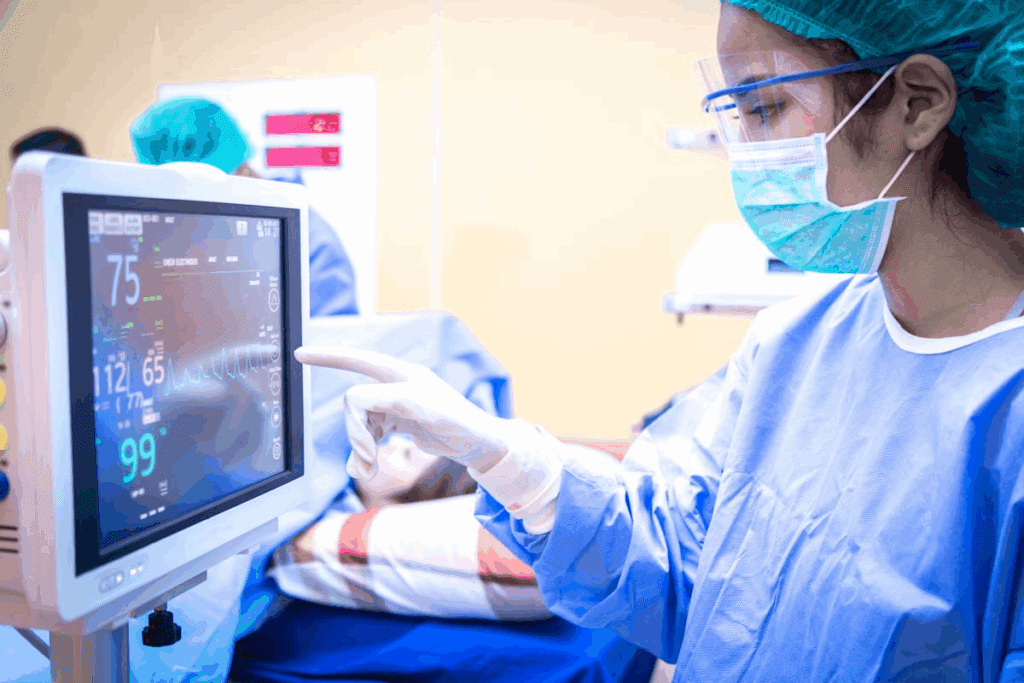
Primary Responsibilities in the Neuro ICU
In the Neuro ICU, our main jobs are seizure control and cerebral edema treatment. We also provide ventilator support for brain injuries or illnesses. Stopping seizures is vital to avoid more brain harm.
Managing swelling in the brain is also important. It helps keep the brain well-oxygenated. Ventilator support is needed for those who can’t breathe on their own. We use specialized ventilation strategies to protect the lungs.
Distinguishing Features from General Critical Care
Neurocritical care is different because it focuses on hemodynamic stability and electrolyte balance. Keeping the blood flow right is key for the brain. Electrolytes help neurons work right.
We watch patients’ blood flow and electrolytes closely. We adjust as needed to keep them stable. This requires a deep understanding of brain function and how different systems work together.
We use the latest in brain monitoring and proven practices. Our team approach ensures the best care for neurological patients. This helps them recover and get back to their lives.
The Neurocritical Care Team: Multidisciplinary Approach
Effective neurocritical care needs a team effort. We know that handling complex brain issues requires teamwork from many healthcare experts.
Key Team Members and Their Roles
The neurocritical care team has several important roles. Neurologist intensivists manage serious brain conditions. They work with neurosurgeons for full care.
Critical care nurses watch over patients and give them treatments. They are key in using continuous EEG monitoring to catch any brain changes.
- Neurologists: Diagnose and manage neurological conditions.
- Intensivists: Oversee critical care, ensuring hemodynamic stability.
- Nurses: Provide round-the-clock care, monitoring patients’ status.
- Rehabilitation specialists: Begin early intervention to maximize recovery.
Collaboration Models for Optimal Patient Care
Working together is essential for the best patient care. The TIMING-ICP study showed how important it is for intensivists and neurosurgeons to work together. We use different ways to work together for complete care.
We have regular multidisciplinary team meetings to talk about patient plans. We also offer family support services to help with emotional and psychological needs.
- Daily rounds involving all team members to discuss patient status.
- Utilization of continuous EEG monitoring for real-time neurological assessment.
- Family meetings to update on patient condition and involve them in care decisions.
By working together and using everyone’s skills, we improve patient care and results in the neurocritical care unit.
Brain Injury Management in the Neurocritical Care Unit
Managing brain injuries in neurocritical care units is complex. It involves many steps to help patients recover. Whether the injury is from trauma or not, quick and effective treatment is key.
Traumatic Brain Injury Protocols
Traumatic brain injuries (TBI) are a big problem worldwide. In our unit, we use special protocols to treat TBI. One important part is ICP monitoring, which uses an ICP bolt or ventriculostomy to check pressure.
Our TBI management includes:
- Initial assessment and stabilization
- ICP monitoring and management
- Ventriculostomy procedures to relieve pressure
- Hypothermia therapy to reduce metabolic demands
- Continuous monitoring of neurological status
| TBI Management Strategy | Description | Benefits |
| ICP Monitoring | Measures intracranial pressure | Early detection of elevated ICP |
| Ventriculostomy | Drains CSF to relieve pressure | Reduces ICP, improves cerebral perfusion |
| Hypothermia Therapy | Lowers body temperature | Reduces metabolic demands, potentially improving outcomes |
Non-Traumatic Brain Injury Care
Non-traumatic brain injuries, like those from stroke or cerebral hemorrhage, need special care. Our team is skilled in handling these cases. We use strategies that fit the injury’s cause and severity.
For non-traumatic brain injuries, we focus on:
- Prompt diagnosis and treatment
- Ventriculostomy procedures to manage hydrocephalus
- Supportive care to maintain optimal cerebral perfusion
- Rehabilitation planning to maximize recovery
We aim to improve patient outcomes and quality of life through detailed brain injury management. Our team works with patients and families to offer personalized care and support during recovery.
Stroke Patient Care: Comprehensive Management Approaches
Comprehensive stroke care includes many treatment paths, like those for ischemic and hemorrhagic strokes. It needs a team effort, with quick actions and specialized care.
Ischemic Stroke Treatment Pathways
Ischemic stroke treatment aims to get blood flowing again to the brain. This is done with tPA through an IV or mechanical thrombectomy in some cases. Giving tPA within 4.5 hours of symptoms is key to better outcomes.
New endovascular methods have widened the treatment window for some. Choosing the right treatment depends on the patient’s imaging results.
Hemorrhagic Stroke Interventions
Hemorrhagic strokes, like ICH and SAH, need quick medical help. The goal is to stop bleeding, lower brain pressure, and avoid complications like vasospasm.
For ICH, managing blood pressure is vital. SAH patients need their aneurysm fixed, then watched for vasospasm.
| Stroke Type | Primary Intervention | Key Considerations |
| Ischemic Stroke | Intravenous tPA, Mechanical Thrombectomy | Time-sensitive, Imaging-based selection |
| Hemorrhagic Stroke (ICH) | Blood Pressure Management, ICP Control | Blood pressure targets, ICP monitoring |
| Hemorrhagic Stroke (SAH) | Aneurysm Securing (Clipping/Coiling), Vasospasm Management | Early aneurysm treatment, Nimodipine use |
Knowing how to manage ischemic and hemorrhagic strokes helps doctors give better care. This leads to better patient results and less risk of problems.
Intracranial Pressure Monitoring and Management
Managing intracranial pressure (ICP) is key in neurocritical care. It uses many monitoring methods and treatments. Keeping ICP under control is vital to prevent brain damage in severe cases.
ICP Monitoring Techniques and Devices
There are several ways to monitor ICP, each with its own benefits and drawbacks. The most trusted method is using an intraventricular catheter.
Other methods include:
- Intraparenchymal monitoring: This places a sensor in the brain tissue.
- Subdural monitoring: A sensor is placed under the dura mater, the brain’s outer layer.
- Epidural monitoring: Sensors are placed between the dura mater and the skull.
| Monitoring Technique | Advantages | Limitations |
| Intraventricular | High accuracy, allows for CSF drainage | Invasive, risk of infection |
| Intraparenchymal | Less invasive than intraventricular, accurate | Limited to a single location, drift over time |
| Subdural | Less invasive, can be used in certain cases where intraventricular is not feasible | May not be as accurate as intraventricular |
| Epidural | Least invasive, easy to place | May not accurately reflect ICP |
Interventions for Elevated Intracranial Pressure
Managing high ICP is critical and involves several steps. First, treatments include:
- Head elevation: Elevating the head of the bed to improve venous drainage.
- Osmodiarrhea management: Using osmotic agents like mannitol to reduce ICP.
- Hyperventilation: Temporarily reducing PaCO2 to decrease ICP.
For cases that don’t respond, more aggressive treatments are needed, such as:
- Barbiturate coma induction: Administering barbiturates to reduce cerebral metabolic rate and ICP.
- Decompressive craniectomy: Surgically removing a portion of the skull to allow the brain to expand.
We use a variety of methods to manage ICP, based on each patient’s needs. Monitoring and adjusting treatments are essential for the best care in neurocritical care.
Seizure Control and Management in Neurocritical Care
Effective seizure control is key in neurocritical care. It needs a mix of strategies to manage seizures and avoid long-term brain damage. We focus on quick and right actions in the neurocritical care unit.
Seizures can greatly affect patient results. So, it’s vital to have strong plans for handling seizure activity. Knowing the different types of seizures and their effects on neurocritical care is important.
Status Epilepticus Protocols
Status epilepticus is a serious condition with long or repeated seizures without breaks. Quick treatment is needed to avoid brain damage and other health issues.
Our way to handle status epilepticus includes:
- Quick check and diagnosis with clinical checks and EEG monitoring
- First treatment with benzodiazepines, then other drugs if needed
- Keeping a close eye on the patient’s brain health and changing treatment as needed
Status Epilepticus Treatment Algorithm
| Treatment Stage | Intervention | Objective |
| Initial | Benzodiazepines | Stop seizure activity |
| Second-line | Antiepileptic drugs (e.g., phenytoin, levetiracetam) | Stop seizures from coming back |
| Refractory | Anesthetic agents (e.g., propofol, midazolam) | Control seizures when other treatments don’t work |
Continuous EEG Monitoring Applications
Continuous EEG monitoring is very important in the neurocritical care unit. It helps us spot seizures and see if treatments are working right away. This is key for patients at risk of non-convulsive seizures or status epilepticus.
The good things about continuous EEG monitoring are:
- Finding seizure activity early, so we can act fast
- Seeing if treatments are working and making changes as needed
- Checking on patients who are very sick or can’t move
By using continuous EEG monitoring in our seizure management plans, we can help patients get better and lower the chance of brain problems.
Cerebral Edema Treatment Strategies
Cerebral edema is a serious condition where the brain has too much fluid. We will look at how to treat it, using both medicine and surgery.
Medical Management Approaches
Doctors use several ways to manage cerebral edema. They focus on fluid resuscitation to keep the brain well-perfused. Osmotherapy agents like mannitol help by pulling water out of the brain.
Corticosteroids are sometimes used, but only for certain reasons like tumors. The right treatment depends on why the edema happened and how the patient is doing.
Surgical Interventions When Necessary
Surgery is needed in some cases to treat cerebral edema. Decompressive craniectomy removes part of the skull to let the brain expand. This lowers the pressure inside the skull.
Ventricular drainage involves putting in a drain to remove cerebrospinal fluid. This is key for severe cases of cerebral edema.
Treating cerebral edema needs a mix of medicine and surgery. Knowing and using these methods helps doctors improve patient care.
Ventilator Support and Respiratory Management in Neurological Patients
Neurological patients often need special ventilator support for their breathing. Good respiratory care is key in neurocritical care. This is because brain injuries can cause breathing failure. We will talk about the need for ventilator support, special breathing strategies, and how to avoid breathing problems linked to the ventilator.
Specialized Ventilation Strategies
For neurological patients with breathing issues, special ventilation strategies are vital. These include:
- Lung-protective ventilation: This method uses smaller breaths to avoid lung damage.
- Positive end-expiratory pressure (PEEP): PEEP keeps lung volume up and boosts oxygen levels.
- Recruitment maneuvers: These help open up closed lung areas, improving gas exchange.
Using these strategies can lead to better patient outcomes and lower the risk of breathing problems.
Preventing Ventilator-Associated Complications
Stopping ventilator-related problems is a big part of caring for neurological patients’ breathing. We use several strategies, including:
| Complication | Prevention Strategy |
| Ventilator-associated pneumonia (VAP) | Regular suctioning, elevating the head of the bed, and using oral care protocols |
| Ventilator-induced lung injury (VILI) | Using lung-protective ventilation strategies |
| Deep vein thrombosis (DVT) | Using pharmacological prophylaxis and mechanical compression devices |
Nutrition support is also key in the ICU. It helps with healing and keeps muscles strong. We make sure our patients get enough nutrition, either through food or IV, based on their needs.
By combining special ventilation strategies with full care, including nutrition, we can help neurological patients on ventilators do better.
Hemodynamic Stability and Cerebral Perfusion Optimization
Keeping the blood flow stable is key for brain health in critical care. We’ll talk about how managing blood pressure and monitoring blood flow help achieve this.
Blood Pressure Management Protocols
Managing blood pressure is vital in neurocritical care. Both high and low blood pressure can harm brain blood flow.
We use special plans to control blood pressure. This includes medicines and careful fluid use.
Cerebral Blood Flow Monitoring Techniques
Monitoring brain blood flow is critical to check if the brain is getting enough blood. We use methods like transcranial Doppler ultrasonography and cerebral oximetry.
| Technique | Description | Advantages |
| Transcranial Doppler Ultrasonography | Measures blood flow velocity in cerebral arteries | Non-invasive, provides real-time data |
| Cerebral Oximetry | Monitors cerebral tissue oxygen saturation | Continuous monitoring, reflects cerebral oxygenation |
Specialized Treatment Protocols for Complex Neurological Conditions
Neurocritical care units are ready to handle complex neurological conditions. They use special treatment plans made for each patient. These plans often need a team effort, using the newest in neurocritical care for the best results.
Subarachnoid Hemorrhage and Vasospasm Management
Subarachnoid hemorrhage (SAH) is a serious condition that needs quick and effective care. Vasospasm, a common SAH complication, can cause big problems if not treated right. We have a detailed plan for SAH and vasospasm, including:
- Early detection and monitoring of vasospasm using transcranial Doppler ultrasonography
- Administration of nimodipine to prevent vasospasm
- Aggressive management of vasospasm with hypertensive therapy and endovascular interventions when necessary
Our SAH management also includes watching for complications and acting fast to avoid risks.
Guillain-Barré Syndrome and Myasthenia Gravis Crisis
Guillain-Barré Syndrome (GBS) and myasthenia gravis crisis are urgent neurological cases. We offer detailed care for these conditions, focusing on:
- Plasmapheresis and intravenous immunoglobulin (IVIG) therapy for GBS
- Intensive care unit (ICU) admission for close monitoring and respiratory support
- Adjustment of immunosuppressive therapy for myasthenia gravis crisis
Our team works closely with patients and their families. We provide supportive care and manage symptoms well.
Spinal Cord Injury Care
Spinal cord injuries (SCI) need a team effort for acute care and long-term rehab. We focus on:
- Early surgical intervention when necessary to stabilize the spine
- Comprehensive rehabilitation planning to maximize functional recovery
- Ongoing support for patients and their families throughout the recovery process
We aim to give holistic care for SCI patients. Our goal is to improve their quality of life and help them recover fully.
Rehabilitation planning is key for these complex conditions. We work with a team to create personalized plans. This ensures the best outcomes for each patient.
Neuropharmacology in Critical Care Settings
Neuropharmacology has changed how we care for patients with brain issues in critical care. We need to know a lot about it to give the best care. This means using the right medicines and treatment plans.
Sedation and Analgesia Considerations
It’s very important to manage pain and sedation well in brain injury patients. Sedation protocols must fit each patient’s needs. We aim for comfort without losing track of their brain health.
We pick different medicines for sedation and pain. Each one works in its own way to help the patient feel better.
Neuroprotective Medication Strategies
Using medicines to protect the brain is a big part of neuropharmacology in critical care. Neuroprotective medications help prevent more brain damage. This can lead to better outcomes for patients.
Managing pain is also key in brain injury care. Good pain management makes patients more comfortable. It can also help their brain health. We look at many things when planning pain care, like the cause of pain and how medicines might affect the brain.
Advanced Neuromonitoring Technologies
Neurocritical care has made big strides with new neuromonitoring tech. These tools change how we watch and care for patients with serious brain issues.
These advanced tools use various devices and methods to keep a close eye on patients. They include multimodality monitoring approaches. This means using different ways to monitor a patient’s brain health all at once.
Multimodality Monitoring Approaches
Multimodality monitoring uses many techniques at once. This includes checking intracranial pressure (ICP), cerebral blood flow (CBF), and electroencephalography (EEG). It gives us a full picture of a patient’s brain health, helping us make quick and smart choices.
By combining data from different monitors, we spot problems early. For example, watching ICP and CBF together helps us keep the brain’s blood flow right. This helps avoid more brain damage.
Data Integration and Clinical Decision Support
It’s key to mix data from different monitors for better decision-making. Advanced neuromonitoring tech lets us gather and study lots of data. This gives us deep insights into a patient’s health.
Clinical decision support systems (CDSS) are important in making sense of this data. They help us see patterns, find oddities, and make the best treatment plans. With CDSS, we can give better care and improve results in neurocritical care.
The use of advanced neuromonitoring tech, along with good data mixing and decision support, is a big leap in neurocritical care. As we keep improving these tools, we’ll see even better results for patients in the future.
Ethical Considerations and End-of-Life Care in Neurocritical Care
In neurocritical care, ethics play a big role. This field deals with saving lives and making tough decisions that affect patients’ futures and quality of life.
Prognostication Challenges
One big challenge is guessing how patients will do. Knowing the outcome helps doctors decide what treatments to keep or stop. But, it’s hard to predict because many things can affect it, like the injury’s severity and the patient’s health.
Prognostication tools and models try to help doctors guess better. But, brain injuries are complex, and patients can react differently to treatments. This makes it hard to be very sure.
Palliative Care Integration in Neurocritical Settings
Adding palliative care to neurocritical care is key. Palliative care helps with symptoms, pain, and stress, no matter the patient’s future. It makes patients more comfortable and helps families make choices.
Palliative care teams work with neurocritical care teams to create care plans. These plans cover physical, emotional, and spiritual needs of patients and their families. This teamwork makes sure care is focused on the patient’s values and wishes.
Palliative care’s effect on long-term outcomes is big. It improves the care experience and can lead to better results for patients with severe brain injuries.
Future Directions in Neurocritical Care
Neurocritical care is set for big changes thanks to new research and tech. The field is growing fast, with new discoveries aiming to better patient care and results.
Emerging Research and Technologies
New research in neurocritical care is all about finding new treatments and understanding complex brain issues. Technologies like artificial intelligence and machine learning are being used to improve diagnosis and tailor treatments.
One exciting area is neuroprotection. Scientists are working on ways to shield the brain from harm and disease. They’re looking at new medicines and advanced monitoring tools to spot early brain problems.
Training and Certification Advancements
As neurocritical care grows, so does the need for special training and certifications. Training programs are being set up to teach healthcare pros the skills needed for top-notch neurocritical care.
Certification in neurocritical care is getting more important. Professional organizations are now giving special certifications to show who’s an expert. These programs boost individual skills and help the whole field grow.
By following these paths, we can keep making neurocritical care better. This will lead to better care for those with serious brain illnesses.
Conclusion: The Evolving Impact of Neurocritical Care
Neurocritical care is changing fast, making a big difference in how we handle serious brain and nervous system problems. We’ve seen big steps forward in how we care for these patients, thanks to new technologies and treatments. Now, doctors all over the world are using these new methods to help patients get better faster.
Specialized units for neurocritical care are key. They use the newest tools and treatments to help patients with complex brain issues. As we keep improving, we also need to think about how to do it without breaking the bank.
By making care better and using resources wisely, we can help more patients and save money. The future looks bright with new technologies and research on the horizon. Neurocritical care will keep playing a vital role in modern medicine.
FAQ
What is neurocritical care, and why is it important?
Neurocritical care is a special field of medicine. It deals with patients who have serious brain injuries or conditions. This care is vital because it helps these patients recover.
What are the primary responsibilities of a neuro ICU team?
A neuro ICU team’s main job is to control seizures and treat swelling in the brain. They also support breathing and keep the body’s fluids and electrolytes balanced. Their work ensures patients get the best care possible.
How is intracranial pressure (ICP) monitored and managed?
Doctors use different methods to check ICP, like ICP bolts and ventriculostomy. If ICP is too high, they use treatments like barbiturate coma and cooling the body. These methods help manage the pressure.
What is the role of continuous EEG monitoring in neurocritical care?
Continuous EEG monitoring helps spot and manage seizures in patients. It lets doctors quickly see and act on changes in brain activity. This is key for the best care.
How are stroke patients managed in a neurocritical care unit?
Stroke patients get a detailed treatment plan based on their type of stroke. Ischemic stroke patients might get clot-busting drugs. Hemorrhagic stroke patients might need treatments for blood vessel spasms and aneurysms.
What is the importance of neuropharmacology in critical care settings?
Neuropharmacology is vital in critical care. It involves using medicines to treat neurological issues like seizures and swelling. It also includes managing pain and using medications to protect the brain.
How is cerebral edema treated?
Doctors treat cerebral edema with medicine and surgery. They use osmotic therapy and sometimes perform a surgery to relieve pressure. Giving fluids is also important for brain injury care.
What is the role of ventilator support in neurological patients?
Ventilator support is essential for patients who can’t breathe on their own. Special ventilation techniques help avoid complications. These patients also get nutrition support.
How are complex neurological conditions, such as subarachnoid hemorrhage and spinal cord injury, managed?
Complex conditions are treated with specific plans made by a team of healthcare experts. These plans might include surgery, medicine, and planning for rehabilitation.
What are the future directions in neurocritical care?
Neurocritical care is evolving with new research and technologies. Advances in training and certification will also improve patient care. These changes will help patients with serious brain conditions even more.
References
New England Journal of Medicine. Evidence-Based Medical Insight. Retrieved from https://www.nejm.org/doi/full/10.1056/NEJMra1208628





