Last Updated on December 1, 2025 by Bilal Hasdemir
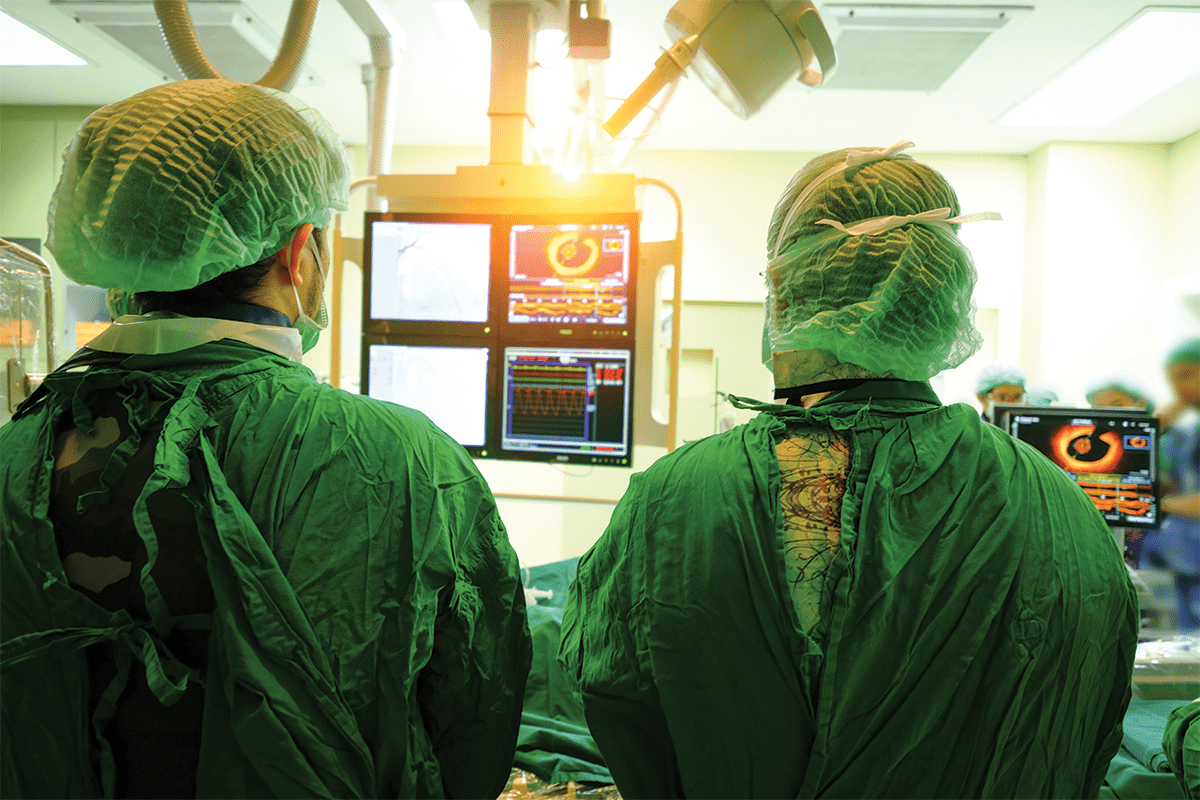
Our essential guide to Neurological surgical pain management. Get the best tips for a hopeful recovery and the surprising truth about pain. Did you know over 200,000 brain surgeries happen every year in the U.S.? These surgeries need careful planning. This includes physical checks, blood tests, and scans like MRIs and CT scans. This prep is key to make sure patients are ready for advanced anesthesia techniques and surgery.
Brain surgery pain worries many patients. But, thanks to comprehensive patient comfort strategies, managing this pain has gotten better. Knowing about these new ways can help ease worries about brain surgery pain.
Key Takeaways
- Brain surgery needs a lot of prep, like physical exams and imaging tests.
- Advanced anesthesia techniques are vital for pain control during surgery.
- There are now better ways to keep patients comfortable during surgery.
- Learning about pain management options can help calm patients’ fears.
- Managing pain during brain surgery is complex but very important.
The Reality of Pain Perception in Brain Surgery

Understanding pain during brain surgery is key for doctors and patients. The brain’s reaction to surgery is complex and involves many factors.
The Brain’s Unique Pain Sensitivity
The brain itself doesn’t feel pain because it lacks pain receptors. But, the tissues around it, nerves, and blood vessels are full of pain-sensitive nerve endings.
Why the Brain Itself Cannot Feel Pain
The brain doesn’t feel pain because it doesn’t have pain receptors. “The brain is a unique organ that does not have pain-sensitive nerve endings. This means some neurosurgical procedures can be done without hurting the brain.
Sources of Pain During Neurosurgery
Even though the brain doesn’t feel pain, other parts can during surgery. This includes:
- The scalp and other external tissues
- Cranial nerves
- Blood vessels
- The dura mater, a membrane surrounding the brain
Using advanced pain management is vital to reduce these pain sources. Effective pain management makes patients more comfortable and helps with better surgery results.
By knowing where pain comes from and using new pain management methods, neurosurgeons can greatly improve patient care.
Is Brain Surgery Painful? Understanding Neurological Surgical Pain Management
Brain surgery is a complex procedure. It needs careful planning. This includes physical exams, blood tests, and imaging tests like MRIs and CT scans. Advanced anesthesia techniques are key to keeping patients comfortable during surgery.
Did you know that despite the complexity of brain surgery, effective pain management strategies have significantly reduced patient discomfort? Before, during, and after surgery, there are many strategies to minimize brain surgery pain.
Key Takeaways
- Advanced anesthesia techniques are essential for reducing pain during brain surgery.
- Comprehensive patient comfort strategies are used before, during, and after surgery.
- Effective pain management is vital to reduce patient discomfort.
- Careful planning and preparation are key for successful brain surgery.
- Imaging tests like MRIs and CT scans ensure the patient’s safety during surgery.
The Reality of Pain Perception in Brain Surgery
Pain during brain surgery is more complex than many think. It’s not always as painful as people imagine. Knowing how pain works in this setting helps reduce worry and improves pain control.
The Brain’s Unique Pain Sensitivity
The brain itself doesn’t feel pain because it lacks pain receptors. But, the tissues, nerves, and blood vessels around it can cause pain during surgery.
Why the Brain Itself Cannot Feel Pain
The brain doesn’t have pain receptors, which is why it’s not sensitive to pain. This lets surgeons do some procedures without hurting the patient.
Sources of Pain During Neurosurgery
Even though the brain itself doesn’t feel pain, other parts can. This includes the scalp, bone, and nerves and blood vessels during surgery.
Common Misconceptions About Brain Surgery Pain
Many people think brain surgery is very painful. But, this is often because they don’t understand the surgery well.
Debunking Popular Myths
One myth is that brain surgery is always very painful. But, thanks to better pain control, it’s much less uncomfortable now.
Scientific Facts About Neurosurgical Discomfort
Research shows that with good pain management, brain surgery can be quite comfortable. New anesthesia and care after surgery help a lot.
| Source of Pain | Description | Management Strategy |
| Scalp Incision | Pain from the initial incision | Local anesthesia |
| Bone Removal | Discomfort during craniotomy | Advanced anesthesia protocols |
| Nerve Manipulation | Pain from nerve stimulation | Precise surgical techniques |
The key to effective pain management in brain surgery lies in understanding the sources of pain and applying advanced protocols to mitigate discomfort.
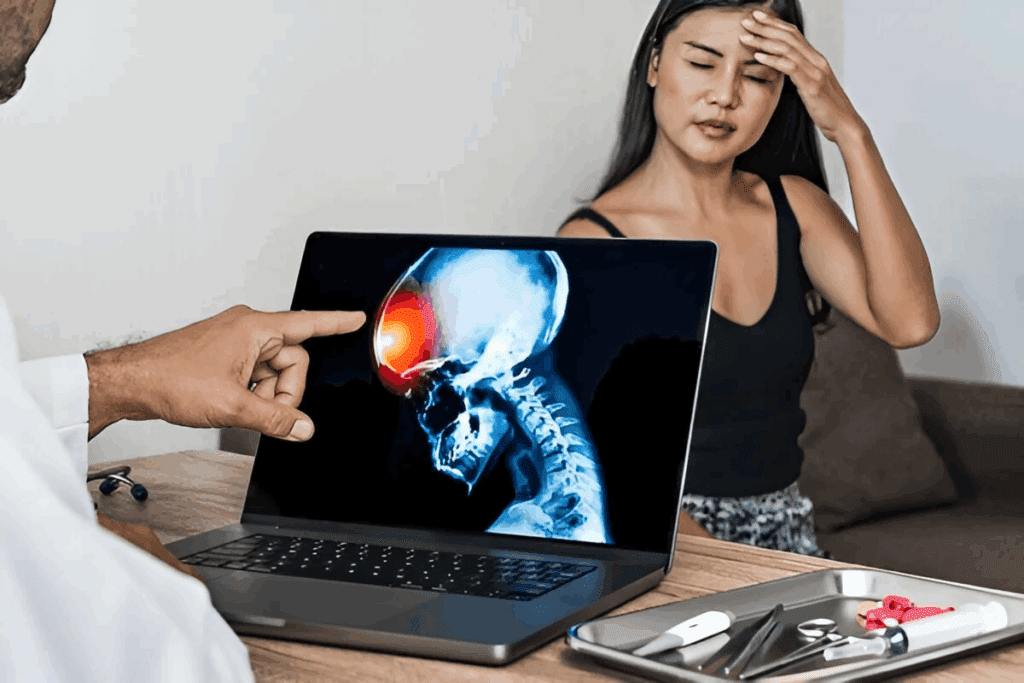
Pre-Surgical Pain Considerations
Pre-surgical pain is a big deal for patients getting brain surgery. It’s important to know what causes this pain. This helps manage it better.
Conditions Leading to Brain Surgery
Brain surgery is needed for things like brain tumors and certain neurological disorders. These can cause a lot of pain.
Pain Associated with Brain Tumors
Brain tumors can lead to pain in different ways. This includes increased pressure inside the skull and irritation of pain-sensitive areas.
Headache Patterns in Neurological Disorders
Neurological disorders can cause headaches that change in intensity and frequency. This can really affect a patient’s life quality.
Pre-existing Pain Before Surgery
Patients getting brain surgery might already have pain. It’s important to check this pain carefully.
Comprehensive Pain Evaluation
Doing a detailed pain check before surgery is key. It helps understand the patient’s pain situation.
Setting Realistic Expectations
By looking at pre-existing pain, doctors can set clear goals for pain control after surgery.
| Condition | Pain Characteristics | Management Approach |
| Brain Tumors | Increased intracranial pressure, localized pain | Corticosteroids, pain medication |
| Neurological Disorders | Varying headache patterns, neuralgia | Specific medication for disorder, pain management protocols |
Anesthesia Protocols in Neurosurgery
Anesthesia protocols are key in neurosurgery. They ensure patients are comfortable and safe during complex surgeries. The choice of anesthesia depends on the surgery type, patient condition, and the neurosurgeon’s preference.
Types of Anesthesia Used
Neurosurgery often uses general or local anesthesia. Each has its own use.
General Anesthesia for Brain Procedures
General anesthesia is used for complex brain surgeries. It keeps the patient unconscious and pain-free. It’s best for long surgeries or when the patient can’t help.
Local Anesthesia Applications
Local anesthesia is for targeted surgeries, like awake brain surgery. It numbs the area, letting the patient stay awake and respond.
Advanced Anesthesia Techniques for Brain Surgery
New anesthesia techniques have boosted neurosurgery results. Two key advancements are:
- Targeted drug delivery systems for precise anesthetic use.
- Monitoring brain function during anesthesia for better safety.
Targeted Drug Delivery Systems
These systems let anesthesiologists target anesthetics to specific areas. This reduces side effects and improves pain control.
Monitoring Brain Function During Anesthesia
Keeping an eye on brain function during anesthesia is vital. Techniques like EEG help monitor brain activity. This allows for quick adjustments to anesthesia levels.
Awake Brain Surgery: A Special Case
Being awake during brain surgery might sound scary, but it’s key for some operations. Awake brain surgery, or awake craniotomy, helps keep important brain functions safe.
Why Patients Remain Conscious
Patients stay awake to help with functional mapping. This method finds out which brain parts control things like speech and movement.
Functional Mapping Requirements
For functional mapping, patients must be awake and able to respond. This lets surgeons see brain functions live. It’s vital for surgeries near brain areas that control key functions.
Benefits of Patient Participation
When patients are awake, the surgery is more precise. Surgeons can see how the patient reacts. This helps them avoid harming important brain parts.
Pain Management During Awake Procedures
Managing pain is key during awake brain surgery. Scalp block techniques and conscious sedation are used to keep pain low.
Scalp Block Techniques
Scalp block techniques use local anesthetics in the scalp. This numbs the area where the surgery is done. It makes the procedure less painful.
Conscious Sedation Approaches
Conscious sedation uses sedatives to relax the patient. It keeps them awake and able to follow instructions during surgery.
Awake brain surgery is a complex method that needs the patient’s help. It uses functional mapping and good pain control. This way, neurosurgeons can get better results.
Neurological Surgical Pain Management Strategies
Neurosurgical procedures need a mix of treatments to manage pain. This includes medicines and non-medical methods. Good pain management is key for patient comfort and better surgical results.
Pharmaceutical Approaches
Medicines are a big part of pain control in neurological surgery. They include early pain medicines and new treatments.
Pre-emptive Analgesic Protocols
Pre-emptive analgesics are given before surgery to lessen pain. Research shows they can cut down on pain after surgery a lot.
Advanced Pharmaceutical Interventions
New medicines and custom pain plans are part of advanced treatments. These plans are made for each patient’s needs and health history.
Non-Pharmaceutical Interventions
Non-medical methods are also key in pain management during neurological surgery. They help reduce stress from surgery and make patients more comfortable.
Surgical Stress Reduction Techniques
Techniques like minimally invasive surgery can greatly reduce pain and discomfort. They also help patients recover faster.
Physical Comfort Optimization
Keeping patients physically comfortable is vital for pain control. This includes using comfortable positions, controlling temperature, and other comfort measures.
| Pain Management Strategy | Description | Benefits |
| Pre-emptive Analgesics | Administering analgesics before surgery | Reduced post-operative pain |
| Advanced Pharmaceutical Interventions | Personalized pain management plans | Improved pain control, reduced side effects |
| Surgical Stress Reduction | Minimally invasive surgical techniques | Less tissue damage, faster recovery |
A leading neurosurgeon says, “Good pain management is more than just easing pain. It’s about making the whole surgical experience better for the patient.”
Pain management is a critical component of neurosurgical care, requiring a complete and team-based approach.
Immediate Post-Operative Pain Experience
Managing pain right after brain surgery is key for patients. This time is very important for their comfort and safety.
First 24-48 Hours After Surgery
The first 24 to 48 hours after brain surgery are very important. Patients are watched closely in intensive care units during this time.
Intensive Care Monitoring
In intensive care, patients are always being watched. This lets doctors quickly see any changes, like pain levels. Being able to quickly change pain plans is very important.
Acute Pain Control Methods
There are many ways to control pain right after surgery. Doctors use medicines like opioids and NSAIDs. They also use deep breathing and relaxation to help.
Patient-Specific Pain Assessment
Every patient feels pain differently. So, doctors need to tailor pain care to each person. They use different tools to check pain levels and adjust treatment plans.
Personalized Medical Treatment Approaches
Doctors make pain plans just for each patient. This might mean changing medicine doses or trying new treatments.
Communication Tools for Non-verbal Patients
For patients who can’t talk, doctors use special tools to check pain. These include pain scales and watching how the patient acts.
By focusing on each patient’s needs, doctors can make care better. The American Pain Society says, “Good pain care is key to quality care.”
Recovery Timeline and Pain Progression
Patients who have had brain surgery need to understand the recovery timeline. This helps them deal with pain after surgery. The recovery has two parts: short-term and long-term. Each part has its own pain management strategies.
Short-term Recovery (1-2 Weeks)
In the first weeks after surgery, patients face different types of pain. Knowing these patterns is key to managing pain well.
Expected Pain Patterns
At first, patients might feel acute pain from the surgery and their body’s reaction. Doctors usually treat this pain with medicine.
Neurological Recovery Progression
As healing starts, the body’s functions begin to come back. It’s important to watch this to make sure the patient is healing right.
Long-term Pain Resolution
The long-term recovery aims to fix any pain that stays and help the brain heal fully.
Chronic Pain Prevention
To avoid chronic pain, a mix of medicine and lifestyle changes is needed. A proactive approach can greatly lower the chance of chronic pain.
Neurological Healing Support
Helping the brain heal is vital for a full recovery. This includes rehab and sometimes extra therapies to keep the brain healthy.
A leading neurosurgeon says, “A well-managed recovery timeline is key to less pain and better brain recovery.” Good pain management and brain support go hand in hand. A complete plan is needed for the best results.
Potential Complications Affecting Pain Levels
Brain surgery is lifesaving but can lead to complications that affect pain. It’s important to understand these complications for better pain management.
Infection and Inflammation
Infection and inflammation can greatly impact pain after brain surgery. Signs of infection include fever, redness, swelling, and increased pain at the surgical site.
Signs of Problematic Pain
Problematic pain shows as increasing pain intensity, pain spreading to other areas, or pain with fever or neurological issues.
Intervention Strategies
Early action is key to manage pain from infection or inflammation. This might involve antibiotics for infection or anti-inflammatory medications.
Nerve Damage Considerations
Nerve damage can cause neuropathic pain. This pain is often sharp, shooting, or burning.
Neuropathic Pain Patterns
Neuropathic pain patterns vary based on the nerves affected. Knowing these patterns is key for diagnosis.
Specialized Treatment Approaches
Treating neuropathic pain often needs specialized medications like anticonvulsants or antidepressants. Sometimes, neuromodulation techniques are considered.
| Complication | Symptoms | Treatment |
| Infection | Fever, redness, swelling, increased pain | Antibiotics |
| Inflammation | Swelling, pain, redness | Anti-inflammatory medications |
| Nerve Damage | Sharp, shooting, or burning pain | Specialized medications, neuromodulation |
Psychological Aspects of Neurosurgical Pain
The mind plays a big role in how we feel pain after neurosurgery. This kind of surgery is not just about physical damage. It also brings a lot of mental stress.
Anxiety and Pain Perception
Feeling anxious can make pain feel worse. This is because our brains link fear and pain together.
Neurological Basis of Fear-Pain Connection
The brain has special areas for fear and pain. When we’re scared, our pain can feel stronger. Knowing this helps us manage pain better.
Patient Psychological Support Methods
Helping patients mentally can really help with anxiety. We use things like talking therapy, relaxation, and teaching about pain control.
Cognitive Strategies for Pain Management
There are ways to think about pain that can help. Mindfulness and cognitive behavioral therapy are good examples.
Mindfulness Techniques
Mindfulness teaches us to stay in the moment. It helps us deal with pain better. Mindfulness-based stress reduction (MBSR) is very helpful.
Cognitive Behavioral Approaches
Cognitive Behavioral Therapy (CBT) helps us see pain differently. It makes pain easier to handle. It’s a great addition to other pain treatments.
| Strategy | Description | Benefit |
| Mindfulness | Focuses on the present moment | Reduces stress and pain perception |
| CBT | Changes pain perception | Enhances pain management |
| Relaxation Techniques | Reduces anxiety | Lowers overall stress levels |
Advanced Medical Technology in Pain Reduction
Advanced medical technology has changed neurosurgery a lot. It makes brain surgery less painful before and after. This is thanks to new surgical methods and tools.
Minimally Invasive Techniques
Modern neurosurgery uses less invasive methods. These methods are less harsh and help patients heal faster. They cause less pain and fewer complications.
Endoscopic Approaches
Endoscopic surgery lets doctors work through small cuts. They use a camera and special tools. It’s great for precise work without harming much tissue.
Laser Surgery Applications
Laser surgery is a cutting-edge tool in neurosurgery. It removes or fixes problems with little harm to healthy tissue. Lasers are used for many neurosurgical tasks, like removing tumors.
Precision Surgical Tools and Pain Reduction
New surgical tools help neurosurgeons do their job better. These tools make procedures more precise and gentle. This reduces the chance of problems.
Neurosurgical Precision Techniques
Techniques like stereotactic surgery and intraoperative MRI have made neurosurgery more precise. These technologies let doctors watch and adjust in real-time. This makes surgeries safer and more effective.
Robotic Assistance Benefits
Robotic systems are being used more in neurosurgery. They help with precise and controlled surgeries. This leads to less pain and quicker healing for patients.
Patient Testimonials and Experiences
Patient testimonials give us a look into the lives of those who have had brain surgery. They share their pain experiences and how they coped.
Varied Pain Experiences
Patients’ pain after brain surgery can differ a lot. Some feel little pain, while others face more severe discomfort.
Success Stories and Challenges
Many patients talk about their successful recoveries. They share the challenges they faced and how they beat them. For example, effective pain management was key for many.
Unexpected Aspects of Recovery
Some patients mention unexpected parts of their recovery. They say emotional support from loved ones was vital. Others talk about practical tips that helped them manage pain.
Coping Strategies from Former Patients
Former patients often share their coping strategies. These insights are helpful for those facing brain surgery. Common strategies include:
- Following a strict medication regimen to manage pain.
- Engaging in gentle physical activity to promote recovery.
- Utilizing support systems, such as family, friends, and support groups.
Practical Tips for Pain Management
Practical tips for pain management include keeping a pain journal to track pain. Using relaxation techniques like deep breathing or meditation also helps.
Support System Utilization
A strong support system is very important. Patients with a good support network often have better outcomes and easier recoveries.
Conclusion: The Comprehensive Approach to Brain Surgery Pain
Understanding pain is key to managing brain surgery pain. Advanced anesthesia and effective strategies are used before and after surgery. This approach is vital for better patient outcomes and fewer complications.
Advanced pain management is essential for reducing brain surgery pain. Healthcare providers use both medicines and non-medical methods. This way, they create pain plans that fit each patient’s needs.
New medical technology has made brain surgery pain management better. Tools like minimally invasive techniques and precise surgical instruments help a lot. As technology gets better, so will pain management, leading to better patient experiences.
Healthcare providers can make sure patients get the best care by focusing on brain surgery pain. This approach helps reduce pain and makes recovery smoother.
FAQ
What is the role of anesthesia in managing pain during brain surgery?
Anesthesia is key in managing pain during brain surgery. It includes general and local anesthesia. Also, advanced techniques like targeted drug delivery systems are used. These ensure patient comfort and safety.
Can the brain itself feel pain during surgery?
The brain itself can’t feel pain. But, tissues and nerves around it can. This shows why managing pain well is so important.
What are the benefits of awake brain surgery, and how is pain managed during these procedures?
Awake brain surgery lets surgeons map brain functions. This helps them avoid harming important areas. Pain is managed with local anesthesia and careful pain assessment. Strategies to reduce stress and improve comfort are also used.
What are the common misconceptions about brain surgery pain, and what are the facts?
Many think brain surgery pain is always severe. But, pain varies greatly among people. Good pain management strategies can help reduce pain.
How is pain managed in the immediate post-operative period after brain surgery?
Right after surgery, pain is managed with close monitoring and acute pain control. Each patient’s pain is assessed and treated personally. This ensures effective pain relief.
What are the possible complications that can affect pain levels after brain surgery?
Complications like infection, inflammation, and nerve damage can increase pain. It’s vital to watch for these signs and act quickly to manage pain.
How can patients cope with pain and anxiety during the recovery period after brain surgery?
Patients can manage pain and anxiety with mindfulness and cognitive strategies. Support systems and practical tips also help during recovery.
What is the role of advanced medical technology in reducing pain during neurosurgery?
Advanced technology, like minimally invasive techniques and robotic tools, reduces pain. It does this by causing less tissue damage and helping patients recover faster.
How can patients prepare for brain surgery to minimize pain and optimize recovery?
Patients should get a thorough pain evaluation before surgery. They should talk to their healthcare team about pain management. Using cognitive strategies for pain management can also help.
What are the long-term pain resolution strategies after brain surgery?
Long-term pain management includes both medication and non-medication approaches. This includes using pre-emptive analgesics and advanced treatments. It also involves reducing stress and supporting neurological healing to prevent chronic pain.