
A neurological exam in urology is a structured assessment of the nervous system for patients with lower urinary tract symptoms. It checks sensory, motor, and reflex functions related to bladder and pelvic control. This exam helps us understand how neurological conditions impact bladder function. What is a neurological exam in urology? Understand neurourology and the crucial, powerful tests specialists use to check nerve function affecting the bladder.
Neurogenic bladder refers to various bladder dysfunctions due to nerve damage. It’s not a single disease. We use these exams to diagnose and treat such conditions, aiming to improve patient outcomes.
Key Takeaways
- Neurological exams in urology assess sensory, motor, and reflex functions.
- These exams help diagnose neurogenic bladder and other lower urinary tract symptoms.
- Specialists use the exam results to guide effective, personalized treatment.
- Neuromodulations and understanding detrusor function are key in managing bladder control.
- Advanced treatments, such as bladder BOTOX ®, may be offered to reduce bladder spasms.
The Fundamentals of Neurological Assessment in Urology
Understanding the neurological assessment in urology is key to diagnosing and treating urological conditions. A thorough evaluation is needed to find the root cause of neurogenic bladder and other disorders.
Definition and Clinical Purpose
A neurological assessment in urology checks how the nervous system controls the lower urinary tract. It’s vital for figuring out how much bladder dysfunction there is and for making treatment plans. The goal is to find any neurological problems that might be causing urological symptoms.
The assessment includes various tests. These include mental status checks, cranial nerve tests, and motor and sensory exams. We also do reflex checks and rectal exams to see how well the anal sphincter is working. These tests help us understand how the nervous system and urinary tract work together.
Patient Populations Requiring Neurological Evaluation
Some patients need a neurological evaluation as part of their urological check-up. This includes those with suspected neurogenic bladder, those who have had spinal cord injuries, and people with neurological disorders like multiple sclerosis or Parkinson’s disease.
We also look at patients with symptoms like urinary incontinence, retention, or frequent infections. These symptoms might point to neurological problems. The American Paraplegic Society guidelines and ICS guidelines on urodynamics help us do these assessments.
By combining neurological findings with urodynamic studies, we get a better understanding of the patient’s condition. This helps us create a treatment plan that works. A team approach is key for managing complex neurourological disorders.
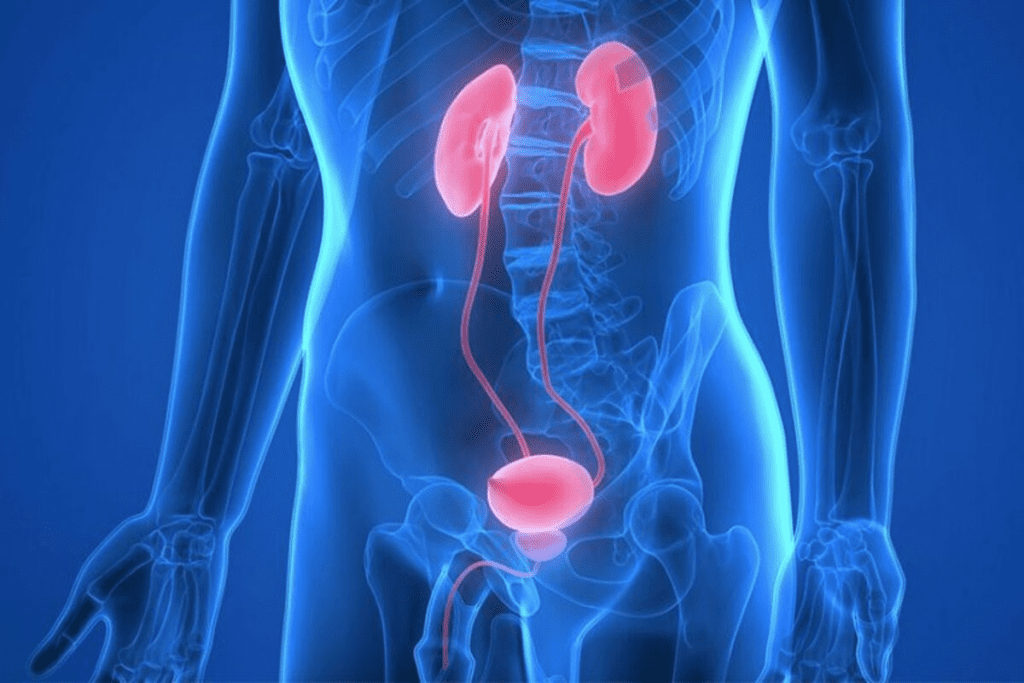
The Neuroanatomy Behind Urological Function
Neuroanatomy is key in controlling urological functions, like micturition. The nervous system and urinary tract work together. This is how we understand urological disorders and how to manage them.
Neural Pathways Controlling Micturition
Micturition, or urination, is controlled by complex neural pathways. These involve the central and peripheral nervous systems. The lumbosacral spinal cord is essential, with neurons and reflex circuits that control the bladder. A study onNCBI shows how vital this is for diagnosing and treating urinary issues.
Sacral Nerve Roots and Bladder Innervation
The sacral nerve roots are key for bladder innervation. They control the detrusor muscle and the urethral sphincter. The bladder’s innervation involves both sympathetic and parasympathetic systems. Studies show that 21-40% of patients with neurogenic bladder have abnormal sacral reflexes or anal sphincter dysfunction.
Common Neurological Disorders Affecting Urination
Neurological disorders like neurogenic bladder, multiple sclerosis, and spinal cord injuries can affect urination. These conditions can cause urinary incontinence or retention. Knowing the neuroanatomy behind these disorders is vital for effective treatment plans.
As we dive deeper into urological function and its neuroanatomy, it’s clear we need a deep understanding. This knowledge helps healthcare providers diagnose and treat urological conditions better. By understanding neural pathways, sacral nerve roots, and common disorders, we can improve patient care.
Step-by-Step Components of a Urological Neurological Exam
The urological neurological exam is a detailed check-up. It helps doctors manage complex urinary issues. This thorough test is key to diagnosing and treating problems with the lower urinary tract.
Mental Status Assessment
A mental status assessment is a key part of the exam. It looks at the patient’s thinking, memory, and decision-making skills. This helps doctors see if the patient can handle their urinary symptoms and follow treatment plans.
Cranial Nerve Evaluation
Cranial nerve evaluation is also vital. It checks how well the nerves that control urination are working. For example, the pontine micturition center in the brain helps control the bladder muscle.
Understanding the detrusor muscle is important. It’s a muscle in the bladder wall that helps with urination. Problems with this muscle can lead to a neurogenic bladder.
Motor Testing
Motor testing is another important part. It checks muscle strength, tone, and reflexes. In urology, it helps see if nerves controlling the bladder are working properly. It looks at the strength of the pelvic floor muscles and the anal sphincter.
Here are some key parts of motor testing in a urological exam:
- Checking muscle strength in the lower legs
- Looking at muscle tone, mainly in the pelvic floor
- Testing reflexes, like the bulbocavernosus reflex
Neuromodulations, like sacral nerve stimulation, can help with neurogenic bladder. These treatments adjust the signals to the bladder.
Sensory Examination in Neurourology
The sensory examination is key in neurourology. It gives us important insights into how the urinary system works. This is vital because it lets us check how the nerves control the lower urinary tract.
Sacral Dermatome Assessment
Checking the sacral dermatomes is a big part of the sensory exam. We look at how sensitive the areas covered by the sacral nerves (S2-S5) are. This helps us spot problems in the nerves that might cause issues with the bladder and bowel.
We test these areas with light touch, pinprick, and vibration. If these tests show something’s off, it could mean there’s damage to the sacral nerves. This damage can affect how well you can control your bladder and bowel.
Perineal Sensation Testing
Testing the perineal area is also very important. This area is covered by the sacral nerves. By checking how sensitive it is, we can find out if there are nerve problems that might be causing urinary issues.
We use a cotton swab to lightly touch the perineal area to see how sensitive it is. We look for any unusual feelings, like being too sensitive or not sensitive enough.
Subjective vs. Objective Findings
It’s important to know the difference between what the patient feels and what we can see. What the patient says is subjective, while what we observe is objective.
What the patient feels is very important. But what we can measure gives us a clearer picture of their nerve function. We use both to get a full picture of their health.
Statistical Significance in Diagnosis
The results of the sensory exam can really help us figure out what’s wrong. By matching these results with other tests, like urodynamic studies, we can be more sure of our diagnosis.
Knowing how important these results are helps us make better choices for our patients. It also helps us find patterns and connections that might not be obvious at first. This helps us understand more about nerve problems in the urinary system.
Critical Reflex Testing for Urological Function
Reflex testing is key in checking how well the bladder works. It helps us see if the nerves controlling the bladder are okay. We look at reflexes like the bulbocavernosus and anal wink reflexes to check this.
Bulbocavernosus Reflex: Technique and Interpretation
The bulbocavernosus reflex shows if the nerves to the urogenital tract are working. To test it, you gently squeeze the glans penis or clitoris. Then, you watch if the anal sphincter contracts. This means the nerves from S2-S4 are okay.
The Paraplegic Society guidelines say this reflex checks the nerves and the sacral cord. Experts say it’s vital for diagnosing bladder problems.
Anal Wink Reflex: Procedure and Significance
The anal wink reflex checks the nerves from S2-S4, too. It’s tested by lightly touching the perianal skin. If the external anal sphincter contracts, it means the nerves are working properly.
This reflex is very important for people with spinal cord injuries or bladder problems. If it’s not there or is weak, it might mean a nerve problem.
Abnormal Reflex Patterns in Neurogenic Bladder
Neurogenic bladder means the bladder doesn’t work properly because of a nerve problem. Detrusor sphincter dyssynergia (DSD) is a big issue here. It’s when the bladder muscle and urethral sphincter contract on their own.
Testing reflexes like the bulbocavernosus and anal wink reflexes is key. It helps doctors figure out and treat DSD.
In short, reflex testing is very important for checking bladder function, mainly in people with nerve problems. By looking at reflexes, doctors can understand bladder control better and make the right treatment plans.
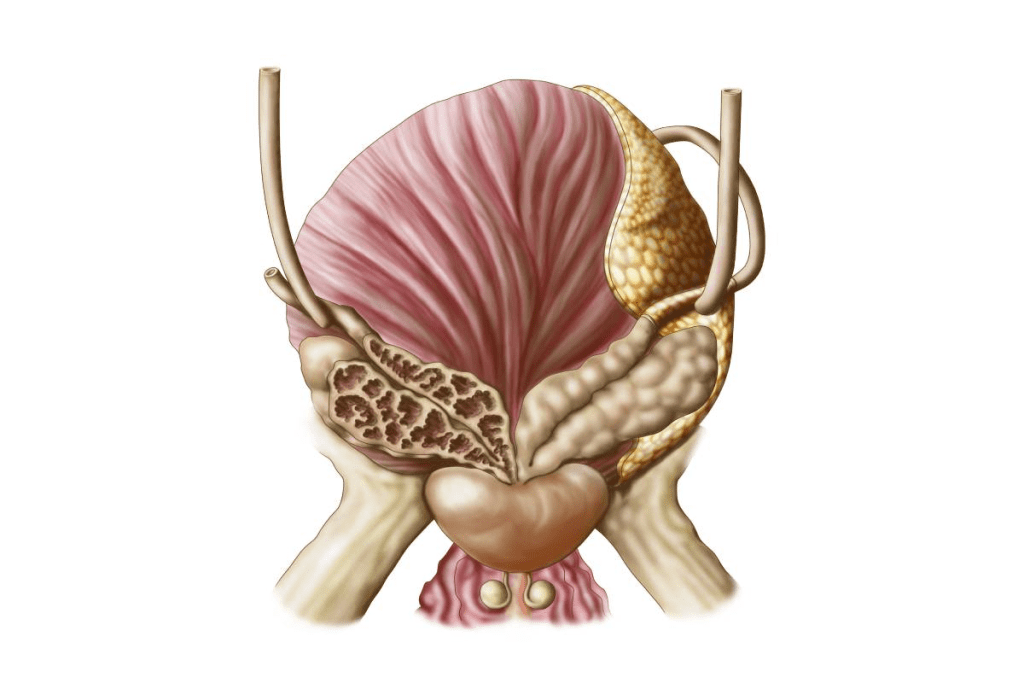
Rectal Examination and Sphincter Function
The rectal examination is key in checking how well the sphincter works. It gives us important information about the nerves. This is vital for understanding how the lower urinary tract works.
Proper Technique and Patient Preparation
To do a rectal exam right, we need the right method and to prepare the patient well. We start by telling the patient what to expect. This makes them feel more at ease.
The patient lies on their side, and we use a lubricated finger. This makes the exam less painful and more accurate.
Patient preparation means more than just explaining the exam. We also make sure they feel respected and comfortable. We tell them to relax to help the exam go smoothly.
Anal Sphincter Tone Assessment
Checking the anal sphincter tone is a big part of the exam. We look at how tight the sphincter is when it’s at rest and when it contracts on purpose. If it’s not right, it could mean there’s a nerve problem.
We check the tone by inserting a finger into the rectum and asking the patient to squeeze. We look at how strong the squeeze is and if they can relax the sphincter. This helps us understand the patient’s nerve health.
Correlation with Urinary Symptoms
The results of the rectal exam can tell us about urinary problems. People with neurogenic bladder or spinal cord injuries often have trouble with both urine and stool. This is because the nerves that control the bladder and bowel are connected.
Knowing how the sphincter functions relates to urine issues is key to treating patients with these problems. For example, someone with a spinal cord injury might need to watch for urinary tract problems. This is part of their follow-up care.
By linking what we find in the rectal exam with the patient’s urine problems, we can create a better treatment plan. This way, we take care of both the urological and neurological parts of their health. It’s a more complete approach to care.
Clinical Integration of Neurological Findings
Understanding neurological findings is key to diagnosing and treating urological disorders. A detailed neurological exam helps us see how the nervous system affects urology.
By mixing neurological findings with other tests, we get a clearer picture of a patient’s health. This is important because it shows how urodynamic studies and neurological findings work together. Together, they help doctors make better diagnoses and treatment plans.
Relationship to Urodynamic Studies
Urodynamic studies are vital for checking bladder function. They measure things like bladder pressure and flow rate. When we look at these studies with neurological findings, we can find the real cause of symptoms.
For example, if a patient with a neurological disorder has abnormal urodynamic results, it might mean they have a neurogenic bladder. This condition needs special care.
Impact on Treatment Selection
Knowing about neurological findings changes how we pick treatments for urological issues. For instance, patients with neurogenic bladder might need neuromodulation therapies like sacral nerve stimulation. The American Paraplegic Society guidelines stress the need for personalized care for urinary problems in spinal cord injury patients.
Multidisciplinary Approach to Neurourological Disorders
Dealing with neurourological disorders needs a team effort. Urologists, neurologists, and others work together. This team approach makes sure patients get care that meets their urological and neurological needs.
Guidelines from the American Paraplegic Society and others support this team-based care for complex urinary issues.
In summary, combining neurological findings with other tests is essential for top-notch care in urology. This way, we can create effective treatment plans that meet the complex needs of these patients.
Conclusion: Advancing Neurological Assessment in Urological Care
Neurourology is growing fast, and so is the need for detailed neurological checks in urology. Places like Liv Hospital are leading the way. They use the latest academic methods and teamwork to improve care.
New ways to check and treat the brain and bladder are making a big difference. These methods, like neuromodulations, help patients control their bladder better. This not only makes life better for them but also helps us learn more about complex issues like vasocongestion.
It’s key to know what terms like vasocongestion mean and how they affect health. As we keep moving forward, using brain findings in urology will be more important than ever. It will help doctors choose the right treatments and work together to solve complex brain and bladder problems.
FAQ
What is the purpose of a neurological exam in urology?
A neurological exam in urology checks patients with lower urinary tract symptoms. It finds the neurological causes of their condition.
What are the key components of a urological neurological exam?
The exam checks sensory, motor, and reflex functions. These help assess bladder and pelvic control.
How do urodynamics relate to neurological assessment in urology?
Urodynamics are key in checking bladder function. They are used with neurological exams to diagnose and manage neurogenic bladder.
What is detrusor sphincter dyssynergia, and how is it diagnosed?
Detrusor sphincter dyssynergia occurs when the detrusor muscle and urethral sphincter don’t work together. This can cause urinary retention or incontinence. It’s diagnosed with urodynamic studies and a neurological exam.
What is the significance of the bulbocavernosus reflex in neurourology?
The bulbocavernosus reflex is a key test. It checks the sacral spinal cord’s health. It’s used to diagnose neurogenic bladder and other urological issues.
How does a suburethral sling compare to stricture, pressure, and no flow on urodynamics?
A suburethral sling treats stress urinary incontinence. A strict high-pressure no flow on urodynamics is a urethral narrowing causing obstructed urine flow. Urodynamics help tell these conditions apart.
What is the role of neuromodulation in managing neurogenic bladder?
Neuromodulations, like sacral nerve stimulation, manage neurogenic bladder. They adjust the neural pathways controlling bladder function.
What is the definition of detrusor function?
Detrusor function is the ability of the detrusor muscle to contract and relax. This allows for proper bladder filling and emptying.
What are normal bladder pressure values?
Normal bladder pressure values depend on the context. Generally, pressures above 40 cmH2O are considered elevated.
What is vasocongestion, and how does it relate to urology?
Vasocongestion is increased blood flow to the genital area. It’s a normal physiological response. In urology, it’s relevant to sexual function and erectile dysfunction.
What is the meaning of sexually incontinent?
Sexually incontinent means involuntary urine loss during sexual activity. It can be a sign of underlying urological or neurological issues.
What are the guidelines for urinary tract management in spinal cord injury patients?
The American Paraplegic Society has guidelines for urinary tract management in spinal cord injury patients. They stress the importance of regular urodynamic studies and proper bladder management.
References
- Dorsher, P. T., & McIntosh, P. M. (2012). Neurogenic bladder. In Advances in Urology.https://onlinelibrary.wiley.com/doi/10.1155/2012/816274
- Anal reflex versus bulbocavernosus reflex in evaluation of patients with spinal cord injury. (2020). Spinal Cord Series and Cases / PMC.https://pmc.ncbi.nlm.nih.gov/articles/PMC6946655/

































