When you’re going through IVF, it can be tough if no embryos develop to the blastocyst stage. This happens to about 40 to 50 percent of fertilized embryos. It’s a big letdown.
New tech in IVF labs has made growing and picking embryos better. By taking embryos to the blastocyst stage, doctors can find the best ones. But, when this doesn’t work, it can be really upsetting for patients.
It’s key to know why embryos stop growing and how to improve IVF success. We get how hard a failed IVF cycle can be. We also know how important it is to have support during this tough time. By looking into the science of embryo growth and what to do next, we help patients keep going.
Key Takeaways
- Approximately 40 to 50 percent of fertilized embryos fail to develop into blastocysts.
- IVF lab advances have improved embryo culture and selection.
- Understanding the reasons behind embryo arrest is key for moving forward.
- The emotional impact of a failed IVF cycle should not be underestimated.
- Support is vital during this challenging time.
Understanding Blastocyst Development in IVF
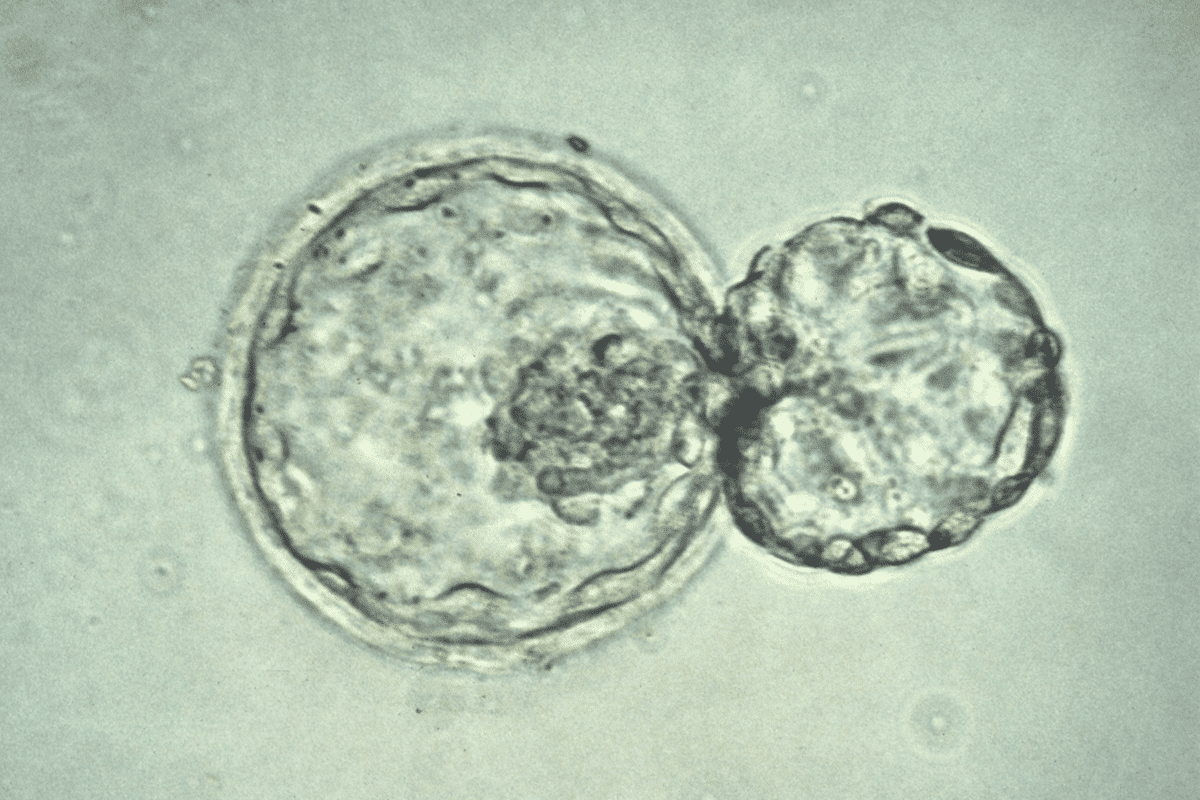
Blastocyst development is key in IVF. Knowing about it can greatly improve treatment success. We’ll look into the details of blastocyst growth, including its normal timeline and what makes a blastocyst successful. Day 5 is also very important.
The Normal Embryo Development Timeline
Embryos grow in a set order, with important steps showing they’re doing well. By day 5 or 6, they usually become blastocysts. Knowing this timeline helps spot problems early. Here’s a quick guide to the main stages:
- Day 1: Fertilization
- Day 2-3: Cleavage stage
- Day 4: Morula stage
- Day 5-6: Blastocyst stage
Understanding these stages helps check if embryos are likely to succeed.
What Defines a Successful Blastocyst
A good blastocyst has clear inner cell mass and trophectoderm. The quality of the blastocyst is a big factor in IVF success. Key signs of a successful blastocyst include:
- Expansion: How much the blastocyst has grown
- Inner Cell Mass (ICM): The quality and presence of the ICM
- Trophectoderm: The quality and number of trophectoderm cells
These signs are checked during blastocyst evaluation.
Characteristic | Description | Importance |
Expansion | Degree of blastocyst expansion | Indicates viability |
ICM Quality | Presence and quality of the inner cell mass | Critical for fetal development |
Trophectoderm Quality | Quality and number of trophectoderm cells | Essential for implantation |
The Significance of Day 5 Development
Day 5 is important because it’s when embryos usually become blastocysts. But, not all embryos develop at the same pace. Some might need until day 6 or 7. The timing of blastocyst growth affects when to transfer embryos.
“The timing of blastocyst development is a critical factor in determining the optimal day for embryo transfer,” said Medical Expert, a renowned fertility specialist. “Understanding this timeline is essential for maximizing the chances of a successful IVF outcome.”
By grasping the embryo development timeline, what makes a blastocyst successful, and the role of day 5, both patients and doctors can better handle IVF’s complexities.
When No Embryos Made It to Blastocyst: How Common Is This?
IVF patients often worry when their embryos don’t turn into blastocysts. This can be tough emotionally and medically.
Statistical Overview of Embryo Arrest
Many studies show that a lot of embryos don’t reach the blastocyst stage. About 40 to 50 percent of fertilized embryos don’t make it to blastocysts. This shows the big challenges in IVF treatments.
IVF attrition is when the number of viable embryos decreases in the lab. It’s a natural part of IVF, but it worries patients a lot.
The 40-50% Development Challenge
The fact that 40 to 50 percent of embryos don’t develop into blastocysts shows the big hurdles in IVF. These challenges include embryo quality, lab conditions, and patient factors.
Knowing this helps manage hopes and make smart choices about IVF treatment.
Understanding What “Arrested Development” Means
“Arrested development” means an embryo stops growing or developing during IVF. This can happen at any stage, including before the blastocyst stage.
Causes of arrested development vary. They include chromosomal issues, egg or sperm problems, and lab factors. Knowing why it happens helps fix it in future IVF cycles.
Primary Causes of Failed Blastocyst Development
Failed blastocyst development is a big challenge in IVF cycles. Knowing why it happens is key to moving forward. When the last embryo doesn’t reach the blastocyst stage, finding out why can help plan the next steps.
Chromosomal Abnormalities (Aneuploidy)
Chromosomal abnormalities, or aneuploidy, are a big reason for failed blastocyst development. Embryos with aneuploidy are less likely to implant or develop into a healthy pregnancy. Research shows many embryos that don’t become blastocysts have these abnormalities.
Egg Quality Factors
Egg quality is very important for embryo development. Things like maternal age and ovarian reserve can affect how well an embryo develops. We’ll look into how these factors affect IVF success.
Sperm Quality Considerations
Sperm quality is also key for embryo development. Poor sperm quality can lead to abnormal fertilization and impaired embryo development. We’ll see how sperm quality affects blastocyst formation.
To understand how these factors affect blastocyst development, let’s look at some data:
Factor | Impact on Blastocyst Development | Percentage of Cases |
Chromosomal Abnormalities | Significant impact, often leading to failed development | 40-60% |
Egg Quality Issues | Moderate to significant impact, depending on age and reserve | 20-40% |
Sperm Quality Issues | Variable impact, can lead to abnormal fertilization | 10-30% |
Knowing these main causes helps couples and fertility specialists make better choices for their IVF journey.
The Impact of Maternal Age on Embryo Development
As women get older, their embryos’ quality and chances of success drop. This is a big deal in IVF treatments. It affects how likely embryos are to reach the blastocyst stage.
Age-Related Decline in Embryo Quality
Embryo quality drops with age. Older women face a higher risk of chromosomal problems in their embryos. This can stop them from becoming blastocysts.
Several things lead to this decline:
- Increased aneuploidy (chromosomal abnormalities)
- Deterioration in egg quality
- Reduced mitochondrial function
Statistical Correlations Between Age and Blastocyst Formation
Studies show a clear link between a woman’s age and blastocyst formation success. Women under 35 have higher blastocyst formation rates than those over 40. The data shows:
Age Group | Blastocyst Formation Rate |
<35 years | 60-70% |
35-37 years | 40-60% |
38-40 years | 20-40% |
>40 years | <20% |
What This Means for Different Age Groups
Maternal age affects embryo development differently for various age groups. Women under 35 have better chances of successful blastocyst formation. This gives them a more hopeful outlook for IVF success. On the other hand, women over 40 face more challenges due to declining embryo quality.
It’s important to understand these age-related factors. This helps manage expectations and make informed IVF decisions. We suggest talking to a fertility specialist to find the best approach for your situation.
Laboratory Factors That May Affect Blastocyst Formation
Laboratory factors play a big role in whether one embryo will become a blastocyst. It’s key to create the best environment for embryo growth in the lab for IVF success.
Culture Media Considerations
The culture media in IVF labs is very important for embryo growth. Different media formulations can greatly affect embryo health. Labs must pick and fine-tune their media to help one embryo become a healthy blastocyst.
The media’s makeup can influence embryo growth, shape, and metabolism. Clinics need to keep up with new research and media advancements to boost IVF success.
Laboratory Protocols and Their Impact
Laboratory protocols, like how embryos are handled and grown, are key to IVF success. Standardized protocols reduce variability and ensure consistent care. Things like temperature, gas mix, and handling can all affect embryo development.
Clinics must have strict quality control to optimize lab protocols for embryo growth. This includes keeping equipment in top shape, training staff, and following best practices.
Discussing Lab Quality With Your Clinic
When you’re going through IVF, talking about lab quality is important. Ask about the laboratory’s quality control measures, the culture media used, and embryo handling and culturing protocols.
Knowing about the lab’s procedures and quality control can give you peace of mind. It’s also a chance to talk about any concerns or questions you have about the lab part of IVF treatment.
Extended Culture: Day 6 Blastocyst Possibilities
Extended culture lets some embryos grow into blastocysts by day 6. This gives hope to those facing challenges. It’s key when no embryos have reached the blastocyst stage by day 5. We’ll look at success rates, quality, and freezing for day 6 blastocysts.
Success Rates for Day 6 Development
Day 5 blastocysts are usually preferred, but day 6 can also lead to successful pregnancies. Success rates for day 6 are slightly lower but are viable.
Our analysis of fertility clinic data shows day 6 blastocyst transfers have a 40-50% success rate. This is a bit lower than day 5’s 50%+ success rate.
Day of Blastocyst Development | Average Success Rate |
Day 5 | 50-60% |
Day 6 | 40-50% |
Day 7 | 20-30% |
Quality Considerations for Late-Developing Blastocysts
The quality of day 6 blastocysts is key for success. We look at several factors, like the blastocyst’s shape, inner cell mass, and trophectoderm integrity.
Morphological grading helps assess blastocyst quality. Grades are based on expansion, inner cell mass cells, and trophectoderm appearance. Higher grades mean better implantation chances.
Freezing Protocols for Day 6 Blastocysts
Freezing day 6 blastocysts involves vitrification to preserve them. We ensure the freezing process is precise to keep the embryo intact.
For frozen embryo transfers, timing and uterine lining preparation are critical. We match the transfer with the patient’s natural or programmed cycle for the best implantation conditions.
In summary, day 6 blastocysts are a viable option for IVF, even when day 5 fails. Understanding success rates, quality, and freezing protocols helps increase pregnancy chances.
Emotional Processing After Failed Blastocyst Development
Not seeing embryos reach the blastocyst stage can be very tough. It’s important to understand the emotional side of this. Finding ways to deal with the sadness and disappointment is key.
Acknowledging Grief and Disappointment
Feeling sad, frustrated, or even hopeless is normal after this. It’s okay to mourn the loss of this IVF cycle. Recognizing these feelings is the first step to healing.
“It’s not just about the embryos; it’s about the hopes and dreams attached to them.” This feeling is common among those trying IVF. It shows how deeply invested they are in the process.
Strategies for Emotional Recovery
Getting over the emotional impact of failed blastocyst development takes time and effort. Self-care, support, and sometimes professional help are important. Here are some ways to help:
Strategy | Description |
Mindfulness and Meditation | Practices that help reduce stress and promote emotional well-being. |
Support Groups | Connecting with others who have experienced similar challenges can provide comfort and understanding. |
Counseling or Therapy | Professional support to address grief, disappointment, and other emotional challenges. |
When to Seek Professional Support
While family and friends can offer a lot of support, some may need professional help. If grief and disappointment feel too much, talking to a mental health professional can be helpful.
It’s essential to prioritize emotional well-being during this challenging time. By acknowledging the emotional impact and seeking the right support, individuals can better handle the challenges of failed blastocyst development.
Consulting With Your Fertility Specialist
Talking to your fertility specialist is key to finding out why embryos might not develop. If no embryos make it to the blastocyst stage, it’s important to discuss the possible reasons and what to do next.
Important Questions to Ask
When you meet with your fertility specialist, ask important questions. This will help you understand your situation better. Some questions to consider are:
- What are the possible reasons for the lack of blastocyst development in my case?
- Are there any underlying issues related to egg or sperm quality that need to be addressed?
- How might our laboratory protocols and culture media be impacting embryo development?
These questions can shed light on the factors at play and suggest ways to improve your chances in future IVF cycles.
Understanding Your Personal Prognosis
Your specialist will look at your age, medical history, and past IVF results to give you a personalized outlook. This will help figure out how likely you are to succeed in future cycles.
Key factors influencing your prognosis include:
- Maternal age and its impact on egg quality
- Previous responses to ovarian stimulation
- Any identified genetic or chromosomal issues
Knowing your personal prognosis can guide your decisions about IVF treatment.
Evaluating Protocol Adjustments
Your specialist might suggest changes to your treatment plan to boost your chances of success. These could be tweaks to how you’re stimulated, lab procedures, or other parts of your treatment.
Potential protocol adjustments may include:
- Modifying the dosage or type of stimulation medications
- Implementing additional laboratory techniques, such as time-lapse embryo imaging
- Considering alternative approaches, such as Day 3 embryo transfer
By collaborating with your specialist and making smart choices, you can increase your chances of a successful pregnancy through IVF.
Alternative Approaches for Future IVF Cycles
When embryo development is tough, looking into new IVF methods can offer hope. If no embryos make it to the blastocyst stage, there are other ways to try. These options might help increase success in future IVF attempts.
Modified Stimulation Protocols
Customizing IVF plans can help each patient get the best results. Modified stimulation protocols adjust the first steps of IVF. This could lead to better egg quality and quantity.
Fertility experts can tweak these plans based on past responses. They might change the medication, dosage, or timing. This is all to help improve egg quality and quantity.
Day 3 Embryo Transfer Considerations
For those who can’t get embryos to the blastocyst stage, a Day 3 embryo transfer might be an option. This means transferring the embryo earlier in its development.
Day 3 transfers might not have the same success rates as blastocyst transfers. Yet, they can be a good choice for some. Always talk to a fertility specialist about this option. They’ll consider your situation and the quality of your embryos.
Adjuvant Therapies and Their Evidence Base
Adjuvant therapies are treatments added to standard IVF to possibly improve results. These can range from medications to supplements. They aim to help the embryo grow better.
It’s key to talk about the science behind these therapies with your fertility doctor. Some have strong research backing them, while others might be less proven. Knowing the benefits and risks helps make better choices for your care.
Exploring these options can help individuals and couples work with their fertility doctors. Together, they can create a plan that tackles specific challenges. This plan aims to increase the chances of success in future IVF cycles.
When to Consider Donor Gametes or Other Options
For many, the reality of no embryos making it to day 5 means looking into other ways to have a child. When traditional IVF doesn’t work, it’s time to think about other options. This can be tough and emotional, but knowing your choices can help you decide what’s best for you.
Evaluating Egg Donation
Egg donation is a common choice for women facing egg quality or quantity issues. Donor eggs come from young, healthy women, boosting the chances of getting pregnant. The process involves matching the donor’s cycle with the recipient’s, then egg retrieval, fertilization, and embryo transfer.
Talking about the legal, ethical, and emotional sides of egg donation with your fertility specialist is key. You’ll learn about donor screening, risks, and the feelings of both the donor and the recipient.
“Egg donation has given many women the chance to experience pregnancy and childbirth, making parenthood a reality for them.”
— Fertility Expert
Exploring Embryo Donation
Embryo donation is for those who’ve tried IVF without success. It uses embryos from others, often from couples who’ve finished their families.
- Embryo donation lets recipients have a pregnancy and give birth.
- It’s a quicker way to become parents than adoption.
- Many clinics have special programs and rules for embryo donation.
Adoption and Child-Free Living as Alternatives
Adoption or choosing not to have children might be the best choice for some. Adoption gives a loving home to a child in need, while child-free living lets people focus on other life aspects.
Both choices need careful thought and emotional preparation. It’s important to weigh the good and bad, talk to loved ones, and maybe get counseling to make a well-informed decision.
The choice to use donor gametes, adopt, or live child-free is very personal. Every person or couple is different, and what’s right for one might not be for another. By looking into these options, people can find a path that fits their values, emotional readiness, and future plans.
Conclusion: Moving Forward After Embryo Development Challenges
Dealing with no embryos reaching the blastocyst stage can be tough. But, remember, even one embryo is a great chance for a healthy pregnancy. This thought can give you hope and direction as you move on.
When thinking about what’s next, it’s key to look at why embryos didn’t develop. Things like chromosomal issues, egg quality, and lab mistakes can play a part. Talking to your fertility doctor can help you understand your situation better and plan for future IVF cycles.
There are other ways to try, like changing how you stimulate your ovaries or transferring embryos on day 3. You might also look into using donor eggs or sperm, or even adoption. Having the last embryo to transfer can really help with your choices.
We’re here to support you every step of the way. We’ll help you understand your options and what affects embryo growth. This way, you can make smart choices about what’s next for you.
FAQ
What does it mean when no embryos reach the blastocyst stage?
When no embryos reach the blastocyst stage, it means they didn’t develop right during IVF. This can happen for many reasons. These include problems with chromosomes, egg or sperm quality, or lab issues.
How common is it for no embryos to make it to blastocyst?
About 40-50% of embryos don’t make it to the blastocyst stage. This shows how tough IVF can be for patients.
What are the primary causes of failed blastocyst development?
Main reasons for failed blastocyst development include chromosomal problems, egg quality, and sperm quality. These all affect how well IVF works.
How does maternal age affect embryo development?
Maternal age greatly affects embryo development. As women get older, embryo quality often goes down. This leads to different success rates for different ages.
Can laboratory factors affect blastocyst formation?
Yes, lab factors like culture media and protocols can affect blastocyst formation. It’s key to talk about lab quality with your clinic.
Is it possible to have a successful IVF cycle with day 6 blastocysts?
Yes, a successful IVF cycle with day 6 blastocysts is possible. Success rates vary based on individual situations. Quality of late-developing blastocysts is also important.
How can I cope emotionally after failed blastocyst development?
After failed blastocyst development, it’s important to acknowledge your feelings. Use strategies for emotional recovery. Also, seek professional help when needed.
What questions should I ask my fertility specialist after failed blastocyst development?
Ask your fertility specialist about your chances, protocol adjustments, and future IVF options. These questions help understand your situation better.
What alternative approaches are available for future IVF cycles?
For future IVF cycles, consider modified protocols, day 3 transfers, and adjuvant therapies. Talk to your fertility specialist about these options.
When should I consider donor gametes or other options?
If repeated IVF cycles fail, think about donor gametes or other options like egg or embryo donation. Discuss these with your fertility specialist.
What are my next steps after experiencing embryo development challenges?
After embryo development challenges, talk to your fertility specialist. Explore alternative approaches and consider donor gametes or other options.
Can I stil have a successful IVF cycle if I had one embryo?
Yes, a successful IVF cycle with one embryo is possible. Success depends on the embryo’s quality and individual circumstances.
What happens if it’s my last embryo?
If it’s your last embryo, discuss the best next steps with your fertility specialist. Consider the embryo’s quality and success chances.
How does no embryos made it to day 5 affect my IVF cycle?
If no embryos reach day 5, it means none developed to the blastocyst stage. This can affect your IVF cycle’s success. You might need to consider other options.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC11224215/[1