Last Updated on November 26, 2025 by Bilal Hasdemir

Nearly 20% of women with ovarian cancer can’t have surgery because their disease is too advanced, highlighting a serious challenge in managing this condition. The chance to undergo surgery greatly influences treatment outcomes, and when no surgery ovarian cancer becomes the reality, it often means more limited treatment options and poorer prognosis.
Deciding against surgery is complex and involves factors such as the disease’s stage, how far it has spread, the patient’s overall health, and the tumor’s specific type. Understanding these details is essential for both patients and doctors to choose the most effective treatment path when surgery is not possible.
Key Takeaways
- Advanced stage diagnosis is a significant factor in determining the suitability of surgery for ovarian cancer.
- Patient’s overall health and tumor characteristics play a critical role in treatment decisions.
- When surgery isn’t an option, other treatments are considered.
- Understanding why surgery isn’t chosen helps patients make better decisions.
- Doctors look at many factors before deciding on a treatment plan.
Understanding Ovarian Cancer and Standard Treatment Approaches
Ovarian cancer is a group of diseases that start in the ovaries. Each type has its own challenges and treatments. Knowing the different types and stages is key to finding the right treatment.
Types and Stages of Ovarian Cancer
Ovarian cancer is divided into several types, like epithelial, germ cell, and sex cord-stromal tumors. Epithelial ovarian cancer is the most common, making up about 90% of cases. The stage of ovarian cancer, from stage I to stage IV, affects treatment and outlook.
Staging is very important because it shows how far the cancer has spread. Stage I means the cancer is only in the ovaries. But stage IV means it has spread to distant organs, making treatment harder.
The Role of Surgery in Conventional Treatment
Surgery is a key part of treating ovarian cancer, mainly for early-stage cases. The goal is to remove as much of the tumor as possible. The success of surgery depends a lot on the stage of the cancer.
Research is ongoing for new treatments, like STRO-002 from Sutro Biopharma. This shows how ovarian cancer treatment is constantly evolving.
Doctors need to know the types of ovarian cancer and their stages to choose the best treatment. This might include surgery, chemotherapy, or both.
No Surgery for Ovarian Cancer: When and Why
Not every ovarian cancer patient needs surgery. A detailed check is needed to find the best treatment. This check looks at many things, like the cancer’s stage, the patient’s health, and the risks of surgery.
Surgical Candidacy Assessment
Figuring out if surgery is right for a patient is complex. It involves several important steps. These include:
- Imaging tests to see how far the cancer has spread
- Blood tests to check the patient’s health and find biomarkers
- A physical check to see how well the patient can handle surgery
Based on these checks, doctors decide if surgery is a good option. They look at the benefits and risks of surgery. A team of doctors and experts discuss these points to make a decision.
The Multidisciplinary Decision-Making Process
A team of doctors, including gynecologic oncologists and medical oncologists, make the surgery decision. They look at the patient’s case and talk about the possible outcomes of different treatments.
| Specialist | Role in Decision-Making |
| Gynecologic Oncologist | Looks at if surgery is possible and what the results might be |
| Radiologist | Reads imaging tests to see how far the cancer has spread |
| Medical Oncologist | Decides if chemotherapy or other treatments are needed |
Working together, the team makes sure all parts of the patient’s situation are looked at. This leads to a better treatment choice.
The team looks at many things to decide the best treatment. This could be surgery or other options.
Advanced Stage Disease: Too Widespread for Effective Surgery
Advanced stage ovarian cancer is a big challenge. The disease has spread too far for surgery to work. It has often spread to different parts of the body, making treatment hard.
Metastasis Patterns and Surgical Limitations
Ovarian cancer usually spreads in the peritoneal cavity. It affects organs like the intestines, bladder, and uterus. This makes it hard to remove tumors surgically.
When ovarian cancer spreads to distant sites like the liver, lungs, or outside the abdomen, surgery is not always possible. In these cases, surgery might not remove all cancerous tissues.
When Cancer Has Spread Beyond Operable Areas
When ovarian cancer spreads to areas that can’t be operated on, like parts of the intestines or major blood vessels, surgery is very challenging. The risks of trying to remove tumors in these areas are often too high.
In such advanced cases, treatment shifts to other options. This includes chemotherapy, targeted therapy, or palliative care. These aim to control symptoms and improve life quality.
Key considerations in determining the feasibility of surgery include:
- The extent of tumor spread
- The location of metastases
- The overall health of the patient
Understanding these factors is key to choosing the best treatment for advanced ovarian cancer.
Tumor Location and Technical Limitations
The place of a tumor is key in figuring out the surgery’s technical hurdles. How easy it is to get to and take out the tumor affects the surgery’s complexity.
Anatomically Challenging Tumor Positions
Ovarian tumors in some pelvic spots are hard to remove. Tumors stuck deep or close to important parts are big challenges. For example, tumors near big blood vessels or key organs make surgery tricky and raise the risk of problems.
The pelvic area’s complex layout, with many nerves, blood vessels, and organs, needs careful planning. Doctors must check the tumor’s spot against these structures to pick the best surgery plan.
When Complete Tumor Removal Is Not Feasible
Sometimes, the tumor’s spot or how far it has spread means it can’t be removed fully. Exploring the tumor might show it’s too mixed up with important parts, making it too risky or not possible to remove.
| Tumor Location | Surgical Challenges | Feasibility of Removal |
| Deep within the pelvic cavity | Access and dissection difficulties | Limited |
| Adjacent to major blood vessels | Risk of vascular injury | Challenging |
| Near critical organs | Risk of organ damage | Difficult |
Knowing these hurdles is key for setting realistic hopes and planning other treatments when surgery isn’t an option.
Medical Comorbidities Preventing Surgical Intervention
Medical conditions can affect whether ovarian cancer patients can have surgery. Other serious health issues can make surgery risky. This means other treatments might be needed instead.
Cardiovascular and Respiratory Conditions
Patients with severe heart or lung problems face higher surgery risks. Issues like heart failure, chronic obstructive pulmonary disease (COPD), or coronary artery disease can lead to complications. For example, heart failure might make it hard for patients to handle surgery or the anesthesia.
Respiratory issues like COPD can also hinder recovery after surgery. This is because lung function is compromised. In these cases, the risks of surgery might be too high, leading to alternative treatments.
Other Health Issues That Increase Surgical Risk
Other health problems can also affect a patient’s surgery suitability. For instance, diabetes, kidney disease, or liver dysfunction can complicate recovery and increase risks of complications after surgery.
Patients with a history of blood clotting disorders or those on anticoagulant therapy also face higher risks. Healthcare providers must carefully consider these factors when deciding if surgery is right for a patient.
Understanding these medical comorbidities helps healthcare teams make better treatment choices. They balance the need to treat cancer with managing other health issues.
Age and Frailty Considerations in Elderly Patients
Dealing with ovarian cancer in older adults is a big challenge. As more people live longer, more older adults get ovarian cancer. It’s key to adjust treatments for this age group.
Older patients often face more health issues and have less energy. Assessing surgical risk for them is tricky. It looks at the cancer and the patient’s health and how well they can function.
Assessing Surgical Risk in Older Populations
Doctors must weigh the risks and benefits of surgery for older ovarian cancer patients. They do a Comprehensive Geriatric Assessment (CGA) to check the patient’s health, other health issues, thinking skills, and support system. “A detailed check before surgery is key to spot high-risk patients.”
The Comprehensive Geriatric Assessment helps find ways to improve the patient’s health before surgery. This could mean fixing health problems, improving nutrition, or helping with thinking or moving issues.
Quality of Life Considerations for Elderly Patients
For many older patients, quality of life is just as important as living a long time. Decisions about treatment must think about how it will affect their life and health.
“The goal is to keep them independent and reduce side effects from treatment.”
Thinking about quality of life means managing symptoms, keeping physical function, and controlling pain. Sometimes, treatments that don’t involve surgery are better to avoid surgery risks.
In summary, treating ovarian cancer in older patients needs a careful approach. It must consider the medical side of the disease and the patient’s overall health and happiness.
Neoadjuvant Chemotherapy: Treatment Before Surgery

Neoadjuvant chemotherapy is now used more often for ovarian cancer, mainly in advanced cases. It involves giving chemotherapy before surgery.
The main reason for this treatment is to shrink tumors. This makes them easier to remove during surgery. It can also improve outcomes for patients with advanced ovarian cancer.
Goals and Benefits of Pre-Surgical Chemotherapy
The main goals of neoadjuvant chemotherapy are to reduce tumor size and check how well the treatment works. It also aims to improve surgical outcomes. The benefits are many:
- Improved surgical resectability: Shrinking tumors makes surgery easier.
- Enhanced patient selection: It helps choose the right patients for surgery.
- Better overall outcomes: It can lead to better survival rates and quality of life.
Determining When to Attempt Surgery After Chemotherapy
Deciding when to have surgery after chemotherapy is complex. It involves checking how well the tumor responds to treatment. A team of healthcare professionals makes this decision.
| Tumor Response | Surgical Considerations | Clinical Implications |
| Significant shrinkage | Surgery is more feasible | Potential for improved outcomes |
| Minimal response | Surgery may not be beneficial | Alternative treatments considered |
| Disease progression | Surgery is typically not recommended | Focus on palliative care |
Healthcare providers carefully check how well the tumor responds to chemotherapy. This helps decide the next steps in treatment. It balances the benefits and risks of surgery.
Poor Performance Status and Surgical Candidacy
Evaluating a patient’s performance status is key in deciding if they can have ovarian cancer surgery. Performance status shows how well a patient can do daily tasks.
Checking performance status is important because it affects how well a patient can handle surgery. Doctors use scores like the Karnofsky Performance Status (KPS) or the Eastern Cooperative Oncology Group (ECOG) to see how well a patient can function.
Understanding Performance Status Scoring
Scoring systems for performance status measure how well a patient can function and care for themselves. The Karnofsky Performance Status (KPS) scale goes from 0 to 100. A score of 100 means the patient is very healthy, while a score of 0 means they have passed away.
The ECOG performance status scale also ranges from 0 to 5. It’s a quick way to see how well a patient is doing. For example, an ECOG score of 0 means the patient is very active, but a score of 4 means they can’t do anything for themselves.
How Low Performance Status Affects Surgical Decisions
A low performance status score means a patient might have serious health problems or be very weak. This makes them a poor surgical candidate. Surgery might be too risky because of the chance of complications and a long recovery.
For patients with a low performance status, treatment might focus on palliative care or non-surgical treatments. This aims to improve their quality of life, not just cure the cancer. A team of doctors, including oncologists and palliative care specialists, will decide the best treatment.
The main goal is to give the patient the best care possible. This means weighing the benefits of treatment against the risks and how it affects their life quality.
Recurrent Ovarian Cancer and Surgical Limitations
Surgery has its limits in treating ovarian cancer that comes back. This makes finding new ways to treat it very important. A team effort is needed to tackle this challenge.
First Recurrence: Evaluating Surgical Options
Deciding on surgery for the first time it comes back is tough. It depends on how far the cancer spread, how long ago it was treated, and the patient’s health.
A study in the Journal of Clinical Oncology found mixed results on surgery’s benefits for ovarian cancer that comes back. This shows the importance of a treatment plan made just for the patient.
“The decision to perform secondary surgery should be based on a careful evaluation of the patient’s condition and the likelihood of achieving a complete resection.”
Multiple Recurrences: Diminishing Returns of Surgery

With each time ovarian cancer comes back, surgery becomes less of an option. The risks of surgery, like complications and long recovery, need to be considered. They must be weighed against any possible benefits.
| Recurrence | Surgical Feasibility | Alternative Treatments |
| First Recurrence | Often considered, depending on initial disease stage and patient health | Chemotherapy, targeted therapy |
| Multiple Recurrences | Limited, due to increased risks and reduced benefits | Palliative care, clinical trials |
Research, like the study on Sutro Biopharma’s STRO-002, shows the hard work in finding non-surgical treatments for ovarian cancer that comes back.
Managing ovarian cancer that comes back needs a complete treatment plan. It should balance surgery with other treatments and care to make the patient comfortable.
Non-Surgical Treatment Alternatives for Ovarian Cancer
Medical research has led to new non-surgical treatments for ovarian cancer. These options are great for those who can’t have surgery. This might be because of the cancer’s stage, their health, or past treatments.
These treatments have many benefits. They can lower the risk of surgery’s side effects and help keep quality of life high. The right treatment depends on the cancer type, stage, and the patient’s health and wishes.
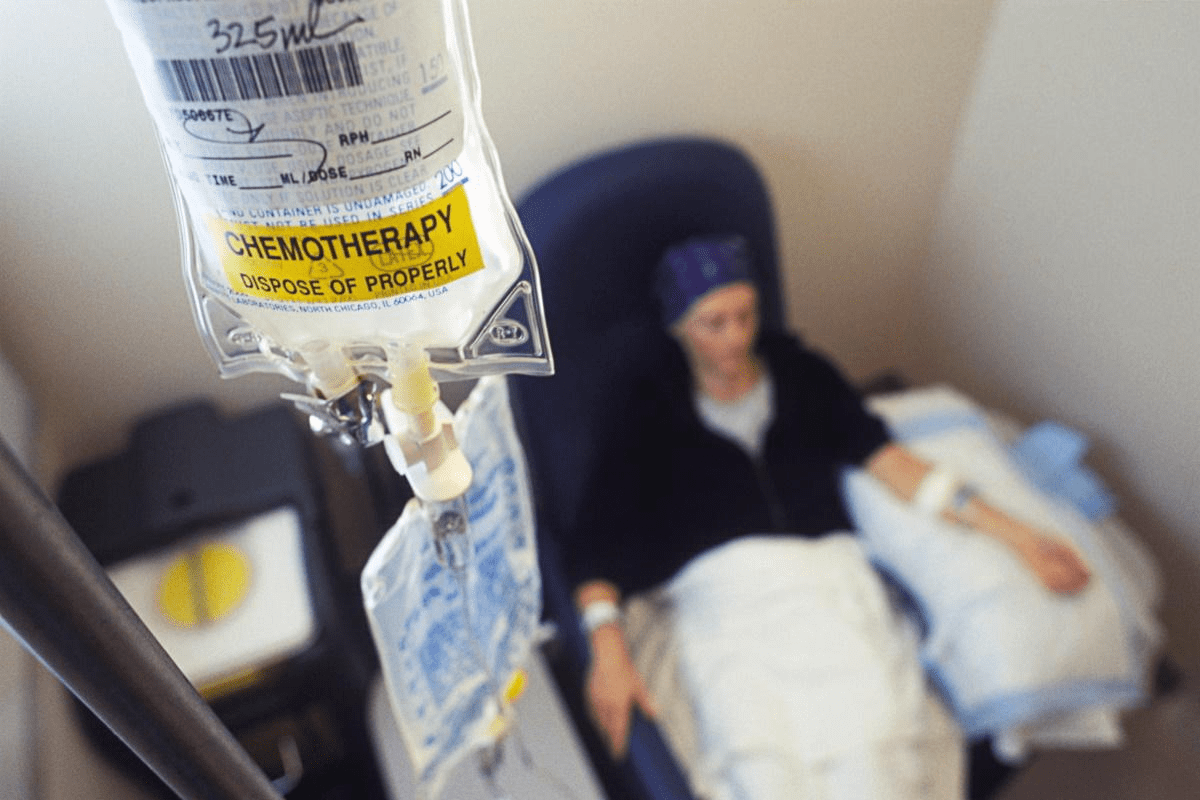
Chemotherapy Regimens as Primary Treatment
Chemotherapy is key for treating ovarian cancer, mainly for those who can’t have surgery. It uses a mix of drugs to fight cancer cells well.
- Platinum-based chemotherapy: Often the first choice, used with other drugs.
- Taxane-based chemotherapy: Works with platinum drugs to better outcomes in ovarian cancer.
The choice of chemotherapy depends on the patient’s health, cancer stage, and past treatments.
Targeted Therapies and Immunotherapy Options
Targeted therapies and immunotherapy are also important for ovarian cancer treatment. They aim to target cancer cells or boost the immune system against cancer.
Targeted therapies target specific cancer molecules. For example, PARP inhibitors help with certain genetic mutations in ovarian cancer.
“The integration of targeted therapies and immunotherapy into the treatment paradigm for ovarian cancer represents a significant advancement in our approach to managing this disease.”
Research into MET inhibition with chemoimmunotherapy started with small cell lung cancer. But it could also help with ovarian cancer, showing the need for more research.
As ovarian cancer treatment evolves, non-surgical options are becoming more important. They offer new hope and possibilities for patients and doctors.
Palliative Care Approaches Instead of Surgery
When surgery is not an option for ovarian cancer, patients can benefit from palliative care. This care focuses on improving quality of life. Palliative care is a specialized medical care for people living with a serious illness, such as ovarian cancer.
Palliative care teams work with patients, families, and other healthcare providers. They manage symptoms, treat pain, and address emotional and practical needs. This care is very helpful for patients with advanced ovarian cancer.
Goals of Palliative Treatment in Advanced Disease
The main goal of palliative care is to improve the patient’s quality of life. It aims to alleviate suffering in all its forms. This includes managing pain, symptoms, and stress, as well as addressing psychological, social, and spiritual needs.
- Symptom management: Palliative care teams are skilled in managing complex symptoms associated with ovarian cancer, such as pain, nausea, and shortness of breath.
- Emotional support: Providing emotional and psychological support to patients and their families is a key part of palliative care.
- Coordination of care: Palliative care teams work closely with other healthcare providers to ensure complete care.
Integrating Palliative Care with Oncology Treatment
Integrating palliative care with oncology treatment can significantly enhance patient outcomes. Studies have shown that patients who receive palliative care alongside cancer treatment have improved quality of life, reduced symptom burden, and sometimes even longer survival.
| Benefits of Integrating Palliative Care | Description |
| Improved Symptom Management | Palliative care specialists are skilled in managing complex symptoms, improving patient comfort. |
| Enhanced Quality of Life | By addressing physical, emotional, and social needs, palliative care enhances overall quality of life. |
| Better Coordination of Care | Palliative care teams work closely with oncology teams to ensure complete, patient-centered care. |
Palliative care is not just for end-of-life care; it can be provided at any stage of ovarian cancer. It can be given alongside curative treatments or when those treatments are no longer effective. By integrating palliative care into ovarian cancer management, healthcare providers can offer more support to patients. They can address their multifaceted needs.
Psychological Impact and Patient Support When Surgery Is Not an Option
Ovarian cancer treatment can vary, but without surgery, patients face special emotional challenges. Hearing that surgery is not possible can be very hard. It can lead to feelings of frustration, anxiety, and uncertainty about the future.
Coping with Changed Treatment Expectations
Dealing with new treatment plans is complex. Patients must accept their new options, which might include chemotherapy or targeted therapy. It’s key for patients to talk openly with their doctors about their choices, what to expect, and the support they can get.
Support from loved ones and support groups is also critical. Sharing stories and connecting with others facing similar issues can offer comfort and advice. Patients should look into these support networks as part of their care.
Support Resources and Mental Health Considerations
It’s important for patients to have access to mental health professionals. Counseling and therapy can help manage anxiety and depression that may come up during treatment.
There are many resources for ovarian cancer patients, like online forums and educational materials. These can offer valuable info and emotional support, helping patients deal with their treatment and improve their life quality.
By understanding the emotional impact of not having surgery and using available support, ovarian cancer patients can cope better with their condition and its treatment.
Conclusion: The Future of Ovarian Cancer Management Without Surgery
Managing ovarian cancer without surgery is a big challenge. Many factors, like how advanced the disease is and the patient’s health, can make surgery too risky. This makes finding other ways to treat the cancer very important.
New treatments and approaches are being developed. This includes better chemotherapy, targeted therapies, and immunotherapy. These options are helping to treat ovarian cancer without surgery.
The future of treating ovarian cancer looks bright. As we learn more about the disease, we’ll find even better ways to treat it. This will involve working together, with doctors, radiologists, and others, to give patients the best care.
By using these new treatments, we can make life better for ovarian cancer patients. Even when surgery isn’t possible, we can help them live better.
FAQ
Why might surgery not be recommended for ovarian cancer?
Surgery might not be recommended if the cancer is too advanced. Or if it has spread too far. Also, if the patient’s health makes surgery too risky.
What are the stages of ovarian cancer, and how do they affect treatment?
Ovarian cancer is staged from I to IV. Stage I is the earliest and most treatable. The stage of the disease greatly affects if surgery is an option.
How is a patient’s suitability for surgery determined?
A team of doctors checks the patient’s health and the disease’s extent. They also look at other factors to decide if surgery is right.
What is neoadjuvant chemotherapy, and how is it used in ovarian cancer treatment?
Neoadjuvant chemotherapy is given before surgery. It shrinks tumors, making them easier to remove. It can also make tumors that were not operable operable.
Can ovarian cancer recur after initial treatment, and what are the implications for surgery?
Yes, ovarian cancer can come back. Deciding to try surgery again depends on many things. This includes where and how far the cancer has come back, the patient’s health, and previous treatments.
What are the alternatives to surgery for ovarian cancer treatment?
Alternatives include different chemotherapy plans, targeted therapies, and immunotherapy. Palliative care also focuses on managing symptoms and improving life quality.
How does a patient’s performance status affect their suitability for surgery?
A patient’s performance status is very important. It shows their health and ability to do daily tasks. A poor performance status may make surgery too risky.
What is palliative care, and how is it integrated with oncology treatment for ovarian cancer?
Palliative care aims to ease symptoms, pain, and stress of cancer and its treatment. It’s part of oncology care to improve life quality, mainly in advanced cases where surgery is not an option.
How do medical comorbidities impact the decision to perform surgery for ovarian cancer?
Certain health conditions, like heart or lung diseases, can raise surgery risks. This makes surgery less viable for some patients.
What are the psychological impacts on patients when surgery is not an option, and how can they be supported?
Patients may feel a lot of emotional pain if surgery is not possible. Counseling and mental health services are key in helping them cope.
Are there emerging trends or advances in non-surgical treatments for ovarian cancer?
Yes, research and new treatments in chemotherapy, targeted therapies, and immunotherapy are improving. These advancements help patients, even if surgery is not an option.
Why is ovarian cancer sometimes too advanced for curative surgery?
Ovarian cancer may be too advanced for surgery if it has spread a lot. This makes it impossible to remove all the cancer.
What role does debulking surgery play in ovarian cancer treatment, and are there alternatives?
Debulking surgery tries to remove as much tumor as possible. While it’s valuable, alternatives like neoadjuvant chemotherapy may be used when debulking is not possible.
How does the location of ovarian tumors impact surgical feasibility?
Tumors in hard-to-reach areas can make surgery very challenging. Tumors in these areas may not be completely removed.
References
- National Cancer Institute. (2025). Ovarian Cancer Treatment (PDQ ®)“Health Professional Version.https://www.cancer.gov/types/ovarian/hp/ovarian-treatment-pdq