Last Updated on November 17, 2025 by Ugurkan Demir
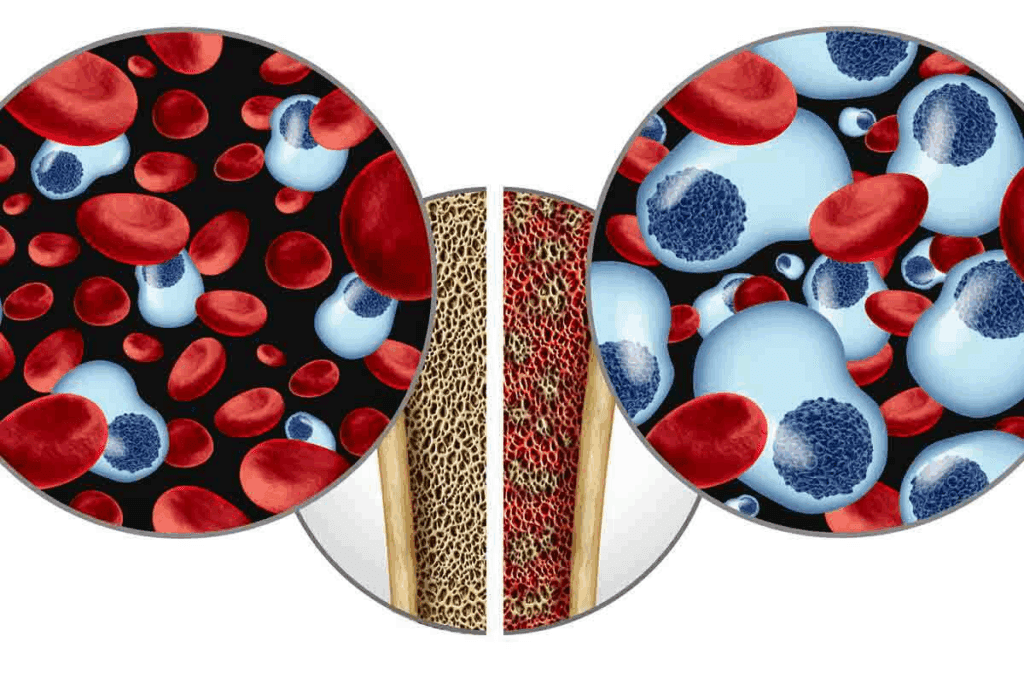
Blood cell production is a complex process. It can be affected by many conditions. Bone marrow, the spongy tissue inside some bones, is key in making red blood cells, white blood cells, and platelets.
Non-cancerous conditions in the bone marrow can cause health problems, from mild to severe. These disorders can mess with blood cell production. This leads to different symptoms and complications. Knowing about these conditions is key for the right diagnosis and treatment.

Bone marrow is key to our health. It’s the spongy tissue inside bones like hips and thighbones. It makes blood cells.
Bone marrow makes blood cells. This includes red blood cells, white blood cells, and platelets. Red blood cells carry oxygen, white blood cells fight infections, and platelets help blood clot.
Stem cells in the bone marrow turn into these cells. This process is carefully controlled. It ensures the right cells are made.
Any problem in this process can cause disorders. For example, not enough red blood cells can lead to anemia. Not enough white blood cells can make infections more likely. Not enough platelets can cause bleeding problems.
Bone marrow disorders can harm the body’s blood cell production. When the bone marrow doesn’t work right, it can cause health issues. These can range from mild to severe.
For instance, aplastic anemia happens when the bone marrow can’t make blood cells. This is very serious and needs quick medical help. Myelofibrosis is another disorder that scars the bone marrow. This also stops blood cell production.
It’s important to understand these disorders to find good treatments. By knowing the causes and how they affect the body, doctors can give better care. They can help manage or even cure these conditions.

Non-cancerous bone marrow disorders affect blood cell production. They can cause health problems, from mild to severe. Knowing about their types and causes helps manage them better.
It’s important to tell cancerous from non-cancerous bone marrow disorders. Cancerous ones, like leukemia, grow out of control. Non-cancerous ones might come from genetic changes, autoimmune issues, or other problems.
Key differences include the presence of cancer cells and how fast the disease grows. Knowing the cause of bone marrow problems is key for treatment.
Non-cancerous bone marrow disorders have many causes. These include genetic issues, environmental factors, and immune problems. Knowing these helps find and treat problems early.
Diagnosing bone marrow disorders involves several steps. These include clinical checks, lab tests, and sometimes, bone marrow biopsies. The goal is to find the cause and see how it affects blood cells.
Tests include blood tests, bone marrow biopsies, and genetic tests. These help doctors understand the disorder and plan treatment.
Understanding non-cancerous bone marrow disorders helps doctors create better treatment plans. This is tailored to each patient’s needs.
Aplastic anemia happens when the bone marrow can’t make enough blood cells. This makes it hard for the body to fight off infections and stop bleeding. It’s a serious condition that needs quick diagnosis and treatment.
Many things can damage the bone marrow and cause aplastic anemia. These include toxins, certain medicines, and viruses. Sometimes, it’s inherited, and other times, there’s no clear reason. The bone marrow’s stem cells, which make blood cells, get destroyed or fail to work.
The expert says knowing why aplastic anemia happens is key to finding good treatments.
The symptoms of aplastic anemia can vary. They often include feeling very tired, getting infections easily, and bleeding or bruising a lot. If it gets worse, it can lead to serious problems like life-threatening infections or severe bleeding.
Finding the right diagnosis can be hard because the symptoms are not always clear. But, a detailed medical check-up can help figure out what’s going on and guide treatment.
To diagnose aplastic anemia, doctors use blood tests, bone marrow biopsies, and other tests. These help see how the bone marrow is working and rule out other conditions. The treatment depends on how bad the condition is and what caused it.
| Treatment Approach | Description | Applicability |
| Immunosuppressive Therapy | Suppresses the immune system to reduce its attack on the bone marrow | Effective for some patients with idiopathic aplastic anemia |
| Bone Marrow Transplantation | Replaces the damaged bone marrow with healthy stem cells | Ideal for patients with severe aplastic anemia and a suitable donor |
| Supportive Care | Includes blood transfusions and antibiotics to manage symptoms and prevent complications | Used for all patients, regardless of the treatment approach |
Doctors tailor treatment plans to each patient. They consider how severe the condition is, the patient’s overall health, and other important factors.
Fanconi anemia is a genetic disorder that makes it hard for the body to make blood cells. It leads to bone marrow failure, causing anemia, infections, and bleeding problems.
Fanconi anemia happens when genes that fix DNA damage are broken. This makes it hard for the body to repair DNA, leading to bone marrow failure and cancer risk. It’s inherited in an autosomal recessive pattern, meaning a child needs two bad copies of the gene to have it.
Genetic testing is key to finding Fanconi anemia. It looks for gene mutations. Families with a history of it can get genetic counseling to understand their children’s risks.
Fanconi anemia shows differently in everyone. Common signs include:
As it gets worse, people might face bone marrow failure and higher cancer risk.
“The diagnosis of Fanconi anemia is often made in childhood, though some cases are diagnosed later. Early diagnosis is key to managing it well.”
Diagnosing Fanconi anemia involves clinical checks, lab tests, and genetic tests. The process includes:
| Diagnostic Test | Purpose |
| Blood tests | To check blood cell counts and find anemia or other issues |
| Bone marrow biopsy | To see if the bone marrow can make blood cells |
| Genetic testing | To find mutations in Fanconi anemia genes |
Managing Fanconi anemia focuses on treating symptoms and complications. Treatments include blood transfusions, medicines to boost blood cell making, and bone marrow transplants in severe cases. Regular check-ups and care are vital to manage it well.
Understanding Fanconi anemia’s genetics, symptoms, and how to diagnose it helps healthcare providers give better care. This improves the quality of life for those affected.
Diamond-Blackfan anemia is a rare condition where the body can’t make enough red blood cells. It has big effects on health. We’ll look at the genetic causes, symptoms, and how it’s treated.
This anemia is linked to problems with genes that make ribosomal proteins. These issues stop the body from making enough red blood cells, causing anemia. Many genes are involved in Diamond-Blackfan anemia. Some of these include RPS19, RPL5, and RPL11. These genes are key to making red blood cells.
People with Diamond-Blackfan anemia often have severe anemia. This can cause:
Each person with Diamond-Blackfan anemia is different. This makes it hard to diagnose and treat.
Doctors usually use corticosteroids to help make more red blood cells. Sometimes, blood transfusions are needed to treat severe anemia.
Here’s a table showing common treatments and their results:
| Treatment Approach | Outcome |
| Corticosteroids | Helps make more red blood cells in some cases |
| Blood Transfusions | Helps manage severe anemia |
| Bone Marrow Transplantation | Can be a cure for some patients |
We keep an eye on new treatments to help those with Diamond-Blackfan anemia.
Shwachman-Diamond syndrome is a rare genetic disorder. It affects the bone marrow and pancreas, causing health problems. This condition impacts many body systems, needing a detailed diagnosis and treatment plan.
The SBDS gene mutations cause Shwachman-Diamond syndrome. These mutations harm the bone marrow and pancreas. Studies show the SBDS gene is key for ribosome function, and its mutations lead to the syndrome’s symptoms.
The syndrome’s cause is complex. It affects the bone marrow, causing blood issues like low white blood cells. It also harms the pancreas, making it hard to digest food.
People with Shwachman-Diamond syndrome face many symptoms. These include frequent infections, not growing well, and trouble digesting food. They also have a higher risk of blood cancers.
Other issues may include bone problems and a weak immune system. Each person’s symptoms are different, so treatment must be personalized.
Doctors diagnose Shwachman-Diamond syndrome by looking at symptoms, lab results, and genetic tests. Finding specific blood and pancreatic problems, along with SBDS gene mutations, confirms the diagnosis.
Treatment focuses on managing symptoms. It includes medicines for low white blood cells and pancreatic issues. Regular check-ups for blood cancers are also important.
In summary, Shwachman-Diamond syndrome is a complex genetic disorder. It needs a team effort to manage. Knowing the genetic causes, symptoms, and how to diagnose it is key to helping those affected.
We look at congenital amegakaryocytic thrombocytopenia, a rare condition. It causes a big drop in platelet count because of bone marrow failure. This shows how complex bone marrow disorders can be and why we need good management plans.
This condition is linked to MPL gene mutations. These changes stop megakaryocytes from making platelets. Knowing how this works helps us find better ways to diagnose and treat it.
The MPL gene is inherited in an autosomal recessive way. This means you need two copies of the mutated gene to have the condition. Carriers have one normal and one mutated gene. They don’t show symptoms but can pass the mutation to their kids.
People with this condition often have low platelet counts from birth or early childhood. They might get petechiae, bruising, and bleeding because of it. As it gets worse, some might also get aplastic anemia, where the bone marrow can’t make blood cells.
The disease can progress differently for everyone. Some might have severe low platelet counts and problems early on. Others might see their counts drop more slowly. Each person needs a special plan to manage their condition.
Managing congenital amegakaryocytic thrombocytopenia involves many steps. This includes supportive care like platelet transfusions to stop bleeding. For some, getting a bone marrow transplant can be a cure by replacing bad marrow with good stem cells.
The outlook for people with this condition depends on how bad it is and how well they respond to treatment. With the right care, some can live better lives. Research keeps getting better at understanding and treating this condition.
To understand GATA2 deficiency, we must look at its genetic roots. It affects blood cell development and the immune system. GATA2 is key for these processes to work right.
GATA2 deficiency comes from gene mutations. The GATA2 gene controls genes for blood and immune system development. It’s inherited in an autosomal dominant way, meaning one mutated gene copy is enough.
“The genetic basis of GATA2 deficiency highlights the importance of genetic testing in diagnosing and managing this condition,” as noted by recent studies. This means a single mutated gene can cause the condition, passed down from either parent.
GATA2 deficiency shows different symptoms in different people. Common issues include severe infections, thrombocytopenia, and myelodysplastic syndromes. Some may also have lymphedema and a higher risk of cancer.
Diagnosing GATA2 deficiency is hard because symptoms vary. A full check-up, including genetic tests and immune function checks, is needed. “Early diagnosis is critical for managing the complications associated with GATA2 deficiency,” experts say.
Diagnosing GATA2 deficiency involves genetic tests, bone marrow biopsies, and immune function checks. Genetic tests confirm the diagnosis. Treatment focuses on managing symptoms like infections and blood issues.
Treatment plans are made for each person’s needs. A team of doctors works together. As research grows, new treatments are being found to help those with GATA2 deficiency.
Understanding non-cancerous myelofibrosis means looking into its causes and effects on the body. This condition scars the bone marrow, leading to health problems like anemia. It can also cause other issues.
Non-cancerous myelofibrosis happens when bone marrow gets replaced with fibrotic tissue. This reduces blood cell production. It can be caused by genetic mutations or autoimmune responses.
We will look into what drives this condition. This includes cytokines and other molecules that cause fibrosis.
Non-cancerous myelofibrosis symptoms vary among patients. Common ones are fatigue, weakness, and shortness of breath. These are mainly due to anemia from reduced bone marrow function.
As the disease gets worse, the spleen and liver may grow. This makes the condition even more complex.
Treatment for non-cancerous myelofibrosis aims to manage symptoms and improve life quality. It includes medicines for anemia, pain relief, and treatments for spleen size reduction.
We will talk about the different treatments available. This includes supportive care and the need for regular monitoring. This helps adjust treatment plans as needed.
Understanding paroxysmal nocturnal hemoglobinuria (PNH) means knowing its molecular basis and clinical effects. PNH is a rare, acquired disease that affects the blood. It causes the destruction of red blood cells, failure of the bone marrow, and the risk of blood clots.
The cause of PNH lies in a mutation in the phosphatidylinositol glycan class A (PIGA) gene. This mutation affects the production of GPI, a molecule that anchors proteins to the cell surface. Without GPI-anchored proteins, hematopoietic cells are more prone to destruction, leading to PNH symptoms.
Red blood cells without these proteins are more likely to be destroyed by the complement system. This is why targeted therapies are so important.
PNH can show up in different ways, including:
These symptoms can greatly affect a patient’s life, making it essential to have a thorough care plan.
| Clinical Feature | Description | Impact on Patient |
| Hemolytic Anemia | Destruction of red blood cells | Fatigue, Shortness of Breath |
| Bone Marrow Failure | Reduced production of blood cells | Increased Risk of Infections, Bleeding |
| Thrombosis | Formation of blood clots | Risk of Stroke, Organ Damage |
Treatment for PNH has greatly improved with the use of complement inhibitors. These drugs, like eculizumab, have made survival better and reduced the risk of blood clots by blocking the complement system.
Managing PNH requires a team effort from hematologists, primary care doctors, and supportive care teams. This approach helps meet the complex needs of PNH patients, leading to better outcomes and quality of life.
Key treatment strategies include:
By using these modern treatments, we can greatly improve the future for PNH patients.
Medical care has made big strides in handling non-cancerous bone marrow disorders. This means people can now control their symptoms better and avoid serious problems. These conditions need careful care and attention to manage well.
Dealing with bone marrow disorders requires a lot of effort. It includes regular check-ups, custom treatment plans, and making lifestyle changes. Knowing how these conditions work helps people manage their care better and live a better life.
Managing bone marrow disorders is a team effort. Healthcare providers, patients, and families must work together. By doing so, people can get the best treatment and live a fulfilling life, even with their conditions.
Non-cancerous bone marrow disorders affect the bone marrow’s ability to make blood cells. They don’t cause cancer. These issues can cause anemia, infections, and bleeding problems.
No, it doesn’t. Some bone marrow issues might be linked to cancer. But many are not, like aplastic anemia or myelofibrosis.
Bone marrow is key in making blood cells. It produces red, white blood cells, and platelets. Any problem here can disrupt blood cell production.
Causes include genetic changes, autoimmune diseases, infections, and chemical exposure.
Doctors use clinical checks, lab tests, and bone marrow biopsies. These help find the cause and plan treatment.
Aplastic anemia means the bone marrow can’t make blood cells. Treatment includes drugs, bone marrow transplants, and blood transfusions.
Non-cancerous myelofibrosis scatters bone marrow, causing anemia and fatigue. It’s different from cancerous forms and needs specific treatment.
PNH is rare and destroys red blood cells. It causes anemia and fatigue. Treatment focuses on the disease’s molecular causes.
Yes, with the right diagnosis and treatment, many can live well. Management includes medicines, lifestyle changes, and blood transfusions.
Proper care is vital. It helps manage symptoms, prevent complications, and improves life quality.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!