Last Updated on November 26, 2025 by Bilal Hasdemir
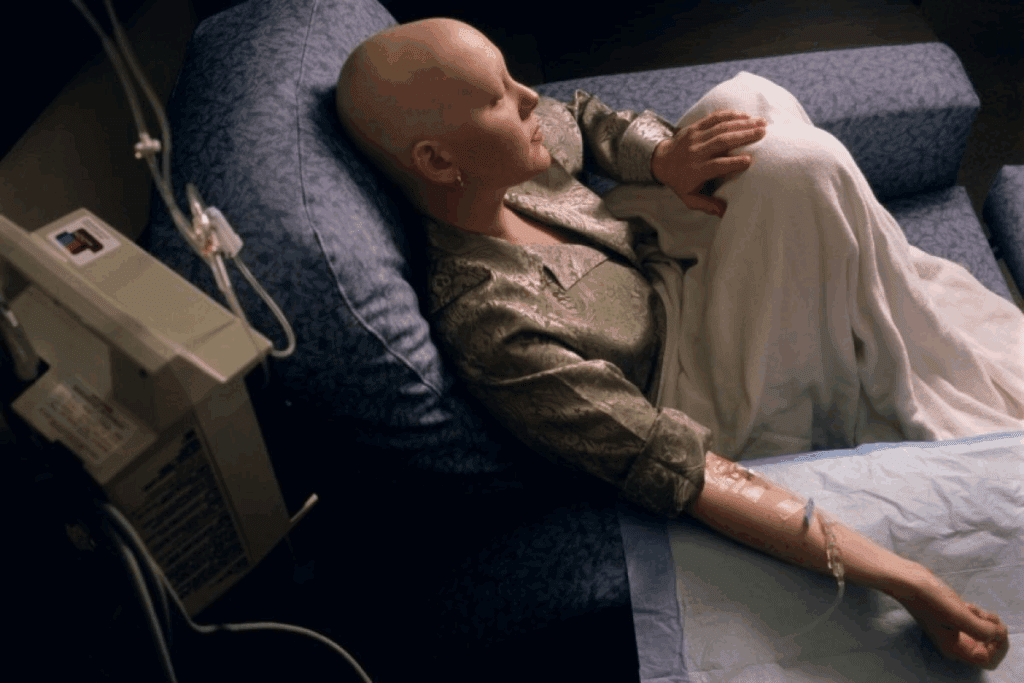
Did you know that adjuvant chemotherapy can greatly improve survival chances for those with non-small cell lung cancer (NSCLC)? Recent studies show it’s effective in lowering the risk of cancer coming back.Explore nsclc chemotherapy treatments and their effectiveness in lung cancer.
Adjuvant therapy is given after the main treatment to kill off any cancer cells left behind. For NSCLC patients, it’s a key part of their treatment. The success of adjuvant chemotherapy depends on the cancer’s stage and type.
Knowing the survival rate for adjuvant chemotherapy is vital for both patients and doctors. It helps them choose the best lung cancer treatment options.
Key Takeaways
- Adjuvant chemotherapy improves survival rates for NSCLC patients.
- The treatment is given after primary therapy to reduce cancer recurrence.
- Success rates vary depending on the type and stage of cancer.
- Adjuvant chemotherapy is a key part of the treatment journey.
- Understanding survival rates helps patients make informed decisions.
Understanding Adjuvant Chemotherapy

Adjuvant chemotherapy is a key part of cancer treatment. It aims to get rid of any cancer cells left after the main treatment. This helps lower the chance of cancer coming back.
Definition and Purpose
Adjuvant chemotherapy is given after the main treatment, like surgery. It’s meant to kill any cancer cells that might have been missed. This way, it helps prevent cancer from coming back.
When is Adjuvant Chemotherapy Recommended?
Doctors suggest adjuvant chemotherapy for patients at high risk of cancer coming back. The choice to have this treatment depends on the cancer type and stage.
Difference Between Adjuvant and Neoadjuvant Chemotherapy
Adjuvant and neoadjuvant chemotherapy are both used in cancer treatment. But they are used at different times and for different reasons. Neoadjuvant chemotherapy is given before the main treatment to make tumors smaller. This makes them easier to remove surgically.
Adjuvant chemotherapy, on the other hand, is given after the main treatment. Its goal is to kill any cancer cells that might have been left behind.
| Characteristics | Adjuvant Chemotherapy | Neoadjuvant Chemotherapy |
| Timing | After primary treatment | Before primary treatment |
| Purpose | Kill remaining cancer cells | Shrink tumors before the main treatment |
| Main Goal | Prevent recurrence | Make surgery easier or more effective |
NSCLC Chemotherapy: Survival Rates and Protocols

Non-small cell lung cancer (NSCLC) is a common lung cancer type. Chemotherapy is key in treating it. The choice of treatment depends on the cancer’s stage and type.
| Subtype | Common Chemotherapy Regimens |
| Adenocarcinoma | Cisplatin + Pemetrexed, Carboplatin + Paclitaxel |
| Squamous Cell Carcinoma | Cisplatin + Gemcitabine, Carboplatin + Paclitaxel |
| Large Cell Carcinoma | Cisplatin + Etoposide, Carboplatin + Paclitaxel |
Timing of Adjuvant Chemotherapy
Adjuvant chemotherapy starts 6-8 weeks after surgery. This is when the patient has fully recovered. It aims to kill any cancer cells left behind.
Survival Statistics: How to Interpret the Data
Understanding survival statistics is key for patients and doctors to make informed decisions about cancer treatment. Survival rates help predict outcomes, but it’s important to know the details behind them.
Understanding Survival Rate Terminology
Survival rates show the percentage of people who live with a certain cancer for a set time, usually five years. The five-year survival rate is a common measure. Yet, it’s vital to remember these rates are based on past data and might not reflect today’s treatments.
The survival rate for non-small cell lung cancer (NSCLC) changes a lot depending on when it’s found. Knowing these rates helps patients understand their chances.
Relative vs. Absolute Survival Benefit
It’s important to know the difference between relative survival benefit and absolute survival benefit. The relative benefit shows how much less likely you are to die or have the cancer come back. The absolute benefit shows the actual increase in survival time between treated and untreated groups.
| Treatment | Relative Survival Benefit | Absolute Survival Benefit |
| Adjuvant Chemotherapy for NSCLC | 20% reduction in risk | 5% increase in 5-year survival rate |
| Targeted Therapy for NSCLC | 30% reduction in risk | 10% increase in 5-year survival rate |
Limitations of Survival Statistics
Survival statistics are useful but have their limits. Results can differ a lot based on health, age, and how well someone responds to treatment. Also, these rates are often from old data, which might not match today’s treatments.
Knowing how to understand survival statistics helps patients make better choices about their care. By understanding the terms, benefits, and limits of survival rates, patients can better navigate their cancer journey.
Adjuvant Chemotherapy Success Rates for Lung Cancer
Adjuvant chemotherapy is key in lung cancer treatment, mainly for non-small cell lung cancer (NSCLC). It helps get rid of any cancer cells left after surgery. This greatly lowers the chance of cancer coming back, which boosts survival chances.
Stage I NSCLC Survival Rates
For Stage I NSCLC, the use of adjuvant chemotherapy is debated. Research shows mixed results. Some studies suggest it might help certain patients, like those with bigger tumors or specific genetic markers.
Stage II NSCLC Survival Rates
In Stage II NSCLC, adjuvant chemotherapy clearly helps. Studies have shown that those who get chemotherapy after surgery live longer than those who don’t.
Stage III NSCLC Survival Rates
For Stage III NSCLC, adjuvant chemotherapy is clear. Using chemotherapy along with other treatments improves survival chances for these patients.
Key Clinical Trials and Their Findings
Many clinical trials have looked into adjuvant chemotherapy in NSCLC. The LACE (Lung Adjuvant Cisplatin Evaluation) study found a big survival benefit with cisplatin-based chemotherapy. The ANITA and JBR.10 studies also support using adjuvant chemotherapy to boost survival rates for NSCLC patients.
These studies highlight the critical role of adjuvant chemotherapy in lung cancer treatment, mainly for Stage II and III NSCLC. As research keeps improving, adjuvant chemotherapy’s role is expected to be even more defined, leading to better outcomes for lung cancer patients.
Adjuvant Treatment for Breast Cancer: Survival Outcomes
Adjuvant therapies are key in fighting breast cancer, giving patients a chance for better survival. These treatments include chemotherapy, hormone therapy, and targeted therapy. They work together to help patients live longer.
Early-Stage Breast Cancer Survival Rates
For those with early-stage breast cancer, adjuvant treatment greatly boosts survival chances. Chemotherapy is often chosen for those with high-risk features like large tumors or lymph node involvement.
Hormone therapy also shows big benefits for hormone receptor-positive breast cancer. It helps lower the chance of cancer coming back and improves survival.
Triple-Negative Breast Cancer Outcomes
Triple-negative breast cancer is tough because it lacks estrogen, progesterone receptors, and too much HER2 protein. The main treatment is anthracycline and taxane-based chemotherapy.
HER2-Positive Breast Cancer Outcomes
Targeted therapies have changed the game for HER2-positive breast cancer. Using trastuzumab in adjuvant therapy has greatly increased survival rates for these patients.
Hormone Receptor-Positive Breast Cancer Outcomes
Hormone receptor-positive breast cancer is treated with hormone therapy. This can include tamoxifen or aromatase inhibitors. These treatments help lower the risk of cancer coming back and improve survival.
Chemotherapy Success Rates for Colon Cancer
Chemotherapy is a key part of treating colon cancer. Different treatments are used to help patients live longer. The success of these treatments is often measured by how well they improve survival rates.
Stage II Colon Cancer Adjuvant Therapy Results
For Stage II colon cancer, doctors might suggest adjuvant chemotherapy. This is when the cancer is at a higher risk. Research shows that this treatment can help patients live longer.
Stage III Colon Cancer Adjuvant Therapy Results
Patients with Stage III colon cancer also benefit from adjuvant chemotherapy. They see better survival rates and more time without the disease coming back.
Risk Factors Affecting Colon Cancer Survival
Several factors can impact how long colon cancer patients live. These include the cancer’s stage, the patient’s health, and genetic mutations.
FOLFOX vs. CAPOX Regimens: Survival Comparison
Choosing between FOLFOX and CAPOX regimens depends on several things. These include how well the patient can handle the treatment and the cancer’s characteristics. Both treatments have been shown to improve survival chances.
| Regimen | Stage II Survival Rate | Stage III Survival Rate |
| FOLFOX | 80-90% | 60-70% |
| CAPOX | 85-95% | 65-75% |
The table shows how FOLFOX and CAPOX compare in survival rates. While both are effective, the right choice depends on the patient’s needs.
Common Chemotherapy Drugs Used in Adjuvant Settings
Adjuvant chemotherapy is a key part of cancer treatment. It aims to get rid of any cancer cells left after the main treatment. The drugs chosen depend on the cancer type, its stage, and the patient’s health.
Adjuvant chemotherapy often uses a mix of drugs. These include platinum-based agents, taxanes, and antimetabolites. Together, they target cancer cells and help prevent them from coming back.
Platinum-Based Agents
Drugs like cisplatin and carboplatin are often used. They mess with the DNA of cancer cells, stopping them from growing and leading to cell death. Research shows they can greatly improve survival rates for some cancers, like non-small cell lung cancer and ovarian cancer.
Taxanes
Taxanes, like paclitaxel and docetaxel, also play a big role. They disrupt the cell division process by affecting microtubules. This leads to cell death. Taxanes are effective against many types of cancer.
Antimetabolites
Antimetabolites, such as 5-fluorouracil (5-FU) and gemcitabine, work differently. They mimic DNA or RNA building blocks, stopping new cell production. They are used to treat various cancers.
| Drug Class | Examples | Cancer Types |
| Platinum-Based Agents | Cisplatin, Carboplatin | Non-small cell lung cancer, ovarian cancer |
| Taxanes | Paclitaxel, Docetaxel | Breast cancer, ovarian cancer, lung cancer |
| Antimetabolites | 5-Fluorouracil, Gemcitabine | Colorectal cancer, breast cancer, pancreatic cancer |
Side Effects of Adjuvant Chemotherapy and Management
Adjuvant chemotherapy helps lower cancer risk but comes with side effects. These can affect a patient’s quality. It’s key to manage these side effects well.
Short-Term Side Effects
Short-term side effects include nausea, vomiting, and fatigue. Hair loss and appetite changes are also common. These effects are most noticeable during and right after treatment.
- Nausea and vomiting can be managed with antiemetic meds.
- Fatigue is common. Patients should rest and save energy.
- Hair loss is usually temporary and can be upsetting.
Long-Term Side Effects
Long-term side effects can last months or years after treatment. These include neuropathy, cognitive changes, and a higher risk of secondary cancers.
Neuropathy can cause numbness, tingling, or pain in the hands and feet. Cognitive changes, or “chemo brain,” can affect memory and focus.
Strategies for Side Effect Management
Managing chemotherapy side effects needs a multi-faceted approach. This includes:
- Medications for specific symptoms, like antiemetics for nausea.
- Lifestyle changes, like diet and exercise, to reduce fatigue and other effects.
- Supportive care, like counseling and physical therapy, for emotional and physical support.
When to Contact Your Healthcare Provider
Patients should know when to seek medical help for side effects. Severe symptoms like intense pain, fever, or signs need immediate care. Report any lasting or worsening side effects to your doctor.
Understanding and managing adjuvant chemotherapy side effects helps patients navigate their treatment better. This improves their quality of life.
Targeted Therapy vs. Traditional Chemotherapy in Adjuvant Settings
The world of adjuvant therapy is changing. Targeted therapy and traditional chemotherapy are two different ways to fight cancer. Knowing the differences helps doctors make better treatment plans.
Mechanism of Action Differences
Targeted therapy attacks cancer cells by focusing on specific proteins or genes. Traditional chemotherapy kills fast-growing cells, including some healthy ones. This difference affects how each treatment works and its side effects.
Targeted Therapy: It targets specific molecular targets, reducing harm to healthy cells.
Traditional Chemotherapy: It affects all fast-growing cells, both cancerous and healthy.
Survival Rate Comparisons
Research shows mixed results on survival rates for targeted therapy and traditional chemotherapy. Targeted therapy might offer better survival for some cancers because it’s more precise. But traditional chemotherapy is often effective, even when there’s no specific targetable mutation.
| Cancer Type | Targeted Therapy Survival Rate | Traditional Chemotherapy Survival Rate |
| HER2-Positive Breast Cancer | 85% | 70% |
| EGFR-Mutated NSCLC | 80% | 60% |
Patient Selection Criteria
Choosing between targeted therapy and traditional chemotherapy depends on several factors. These include the cancer type and stage, and the presence of specific biomarkers. Testing for biomarkers is key to finding the right treatment for each patient.
- Biomarker testing to identify targetable mutations
- Cancer stage and type
- Patient’s overall health and preferences
Cost-Effectiveness Considerations
Targeted therapy is often more expensive than traditional chemotherapy. But for patients with the right biomarkers, it might offer better results. This could make the higher cost worth it.
Cost-effectiveness analysis looks at drug costs and side effect management. It also considers how the treatment affects a patient’s quality of life.
Personalized Approaches to Adjuvant Therapy
Personalized adjuvant therapy is changing how we treat cancer. It tailors treatment to each patient’s unique needs. This makes treatments more effective and reduces side effects.
Biomarker Testing
Biomarker testing is key in personalizing cancer treatment. It finds specific biomarkers linked to a patient’s cancer. This helps doctors choose the best treatment plan.
For example, biomarker testing can show if a breast cancer patient will benefit from hormone therapy.
Key biomarkers used in cancer treatment include:
- ER/PR status for breast cancer
- HER2 status for breast cancer
- KRAS mutations for colorectal cancer
- EGFR mutations for non-small cell lung cancer
Genomic Assays
Genomic assays give insights into a tumor’s genetics. They help predict cancer recurrence and the benefit of adjuvant therapy. These assays are useful when treatment options are unclear.
Examples of genomic assays include:
- Oncotype DX for breast cancer
- ColoPrint for colon cancer
Risk Assessment Tools
Risk assessment tools help doctors evaluate cancer recurrence risk. They look at tumor size, grade, and lymph node status. These tools guide treatment decisions.
| Risk Factor | Description | Impact on Treatment Decision |
| Tumor Size | Larger tumors are associated with a higher risk | May indicate need for more aggressive adjuvant therapy |
| Tumor Grade | Higher-grade tumors are more aggressive | May indicate need for adjuvant therapy |
| Lymph Node Status | Positive lymph nodes indicate a higher risk | May indicate need for adjuvant therapy |
Emerging Predictive Technologies
New technologies like artificial intelligence are changing adjuvant therapy. They can analyze complex data to find patterns. This helps personalize treatment even more.
Future directions for personalized adjuvant therapy include:
- Integration of multiple data sources to inform treatment decisions
- Development of more sophisticated genomic assays
- Use of artificial intelligence to predict treatment outcomes
Quality of Life Considerations During and After Adjuvant Chemotherapy
Quality of life is key for cancer patients and their doctors. Adjuvant chemotherapy helps lower cancer risk but affects well-being. It’s important to think about this.
Physical Well-being
Adjuvant chemotherapy can cause side effects like fatigue, nausea, hair loss, and neuropathy. These symptoms can make daily life hard. They can affect a patient’s ability to do everyday tasks.
Managing Physical Side Effects is key to a better quality of life. This includes medicines, lifestyle changes, and other therapies. For example, exercise can help with fatigue and improve physical function.
Emotional and Psychological Impact
The emotional and psychological effects of adjuvant chemotherapy are significant. Anxiety, depression, and fear of cancer coming back are common. Emotional support from loved ones and mental health experts is very important.
Supportive Care Resources
Supportive care can greatly improve life during and after chemotherapy. It includes nutrition advice, psychological support, and rehab programs. These help a lot.
| Supportive Care Resource | Description | Benefit |
| Nutritional Counseling | Personalized dietary advice to manage treatment side effects | Improved nutritional status, reduced side effects |
| Psychological Support | Counseling and therapy to address emotional and psychological needs | Reduced anxiety and depression, improved coping mechanisms |
| Rehabilitation Programs | Physical therapy and rehabilitation to regain strength and function | Improved physical function, enhanced quality of life |
Return to Work and Normal Activities
Going back to work and normal activities after chemotherapy needs planning. Patients should start slowly and listen to their bodies. It’s important not to overdo it.
By focusing on quality of life, doctors can give better care. This care looks at the whole patient, not just the cancer. It leads to better results and happier patients.
Decision-Making: When Adjuvant Chemotherapy May Not Be Worth It
Choosing to have adjuvant chemotherapy is a big decision. It depends on many factors. Each person’s situation is different, affecting the treatment’s benefits and risks.
Patients and doctors must think about the good and bad sides of chemotherapy. This helps decide if it’s the right choice.
Risk vs. Benefit Assessment
First, we look at the good and bad of chemotherapy. We consider the cancer’s stage and how likely it is to come back. We also think about how chemotherapy can change these things.
Considerations for Age and Comorbidities
Age and other health problems are important too. Older people or those with other health issues might face more risks. This can affect their decision.
Patient Preferences and Values
It’s key to know what matters most to the patient. What are their goals and values? How do they see the treatment’s benefits and risks? This helps make a choice that fits their life.
Shared Decision-Making Approaches
Working together is vital. Patients, families, and doctors need to talk and share information. This way, they can make a choice that’s well-informed and right for everyone.
Conclusion: The Future of Adjuvant Therapy and Survival Outcomes
Adjuvant therapy is key in cancer treatment, boosting survival rates. The future looks bright with new technologies and methods coming. These advancements promise better care for cancer patients.
Adjuvant therapy, including chemotherapy and targeted therapy, has changed cancer care. It helps patients and doctors make better treatment choices. This knowledge is vital for informed decisions.
Research is moving forward, aiming for more effective treatments. New tools like genomics and artificial intelligence will help. These innovations could lead to treatments that are more precise and effective, improving life quality for patients.
Thanks to adjuvant therapy, cancer treatment is getting better. This brings hope to patients and their families. Staying updated on cancer care helps individuals take charge of their health and make informed choices.
FAQ
What is adjuvant chemotherapy, and how does it work?
Adjuvant chemotherapy is a treatment given after primary therapy. It aims to get rid of any cancer cells left behind. This helps lower the chance of cancer coming back and improves survival chances.
What is the difference between adjuvant and neoadjuvant chemotherapy?
Adjuvant chemotherapy is given after primary treatment. Neoadjuvant chemotherapy is given before. Adjuvant aims to kill any leftover cancer cells. Neoadjuvant aims to shrink tumors before surgery.
What are the standard chemotherapy regimens for NSCLC?
For NSCLC, standard treatments include platinum-based chemotherapy. This has been shown to increase survival rates. Other treatments might include taxanes, antimetabolites, and targeted therapy agents.
How is the timing of adjuvant therapy after lung surgery determined?
Adjuvant therapy timing after lung surgery starts a few weeks after. It depends on the patient’s health and cancer stage.
What are the survival rates for adjuvant chemotherapy in NSCLC patients?
Adjuvant chemotherapy significantly improves survival rates in NSCLC, particularly for stage II and III cases. Studies show it reduces cancer recurrence risk.
What are the common side effects of adjuvant chemotherapy?
Adjuvant chemotherapy can cause side effects like nausea and fatigue. It can also lead to long-term issues like neuropathy and secondary cancers. Managing these side effects is key to improving patients’ quality of life.
How do targeted therapy and traditional chemotherapy differ in adjuvant settings?
Targeted therapy targets specific cancer cells. Traditional chemotherapy kills fast-growing cells. The choice depends on the cancer type and stage.
What is personalized adjuvant therapy, and how is it determined?
Personalized adjuvant therapy uses biomarkers and genomic assays to find the best treatment. New predictive technologies are also being developed to make treatments more effective.
How does adjuvant chemotherapy affect patients’ quality of life?
Adjuvant chemotherapy can impact patients’ physical and emotional health. Supportive care is vital to help manage side effects and improve quality of life.
What factors are considered when deciding whether to undergo adjuvant chemotherapy?
Deciding on adjuvant chemotherapy involves weighing risks and benefits. Age, comorbidities, patient preferences, and shared decision-making are important factors.
What is the role of immunotherapy in NSCLC treatment?
Immunotherapy uses the body’s immune system to fight cancer. It’s effective in treating NSCLC, mainly in advanced cases.
How do chemotherapy regimens for colon cancer vary depending on the stage of the cancer?
Chemotherapy for colon cancer changes with the cancer stage. For stage III, treatments like FOLFOX or CAPOX are used.
References
- Li, K., et al. (2025). Survival analysis of postoperative adjuvant chemotherapy for stage IB NSCLC: Racial heterogeneity in efficacy. Thoracic Cancer, 16(13), 1662-1670. https://pubmed.ncbi.nlm.nih.gov/40904175/






