Last Updated on November 26, 2025 by Bilal Hasdemir

Prostate cancer is a big health issue for men all over the world. It’s one of the most common cancers in men. As it gets worse, it can really change how well treatment works and how long patients live.
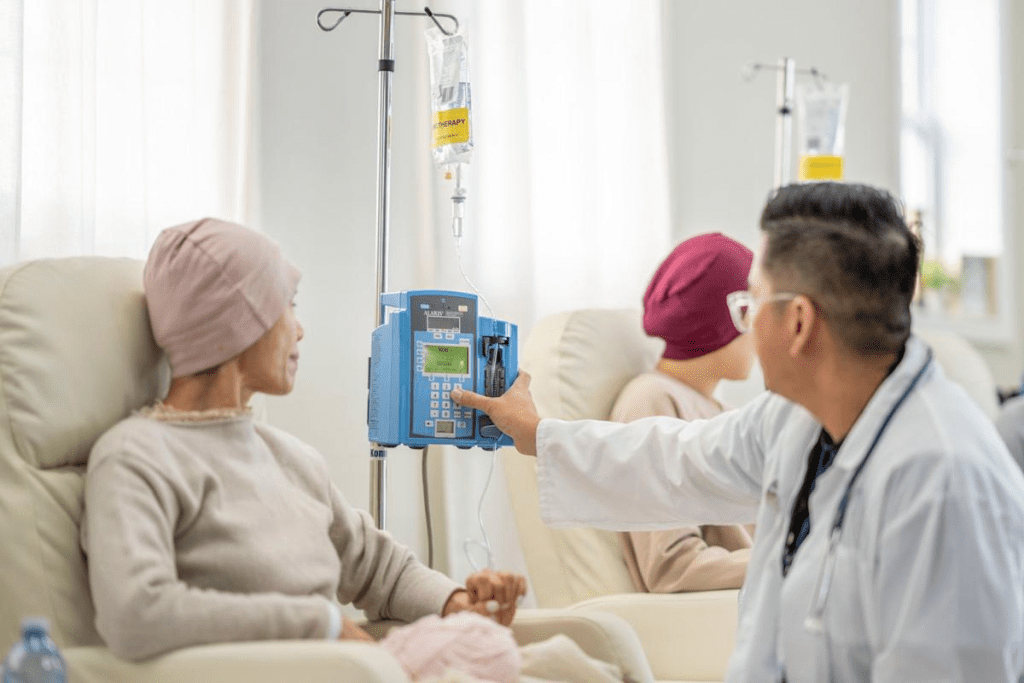
Stopping cancer treatment is a big decision. It’s not made lightly. Oncologists usually stop chemotherapy when the treatment no longer works or when the patient’s overall health cannot tolerate it.
Knowing why treatment stops can help patients and their families make better choices.
Key Takeaways
- Prostate cancer is a common malignancy in men worldwide.
- Treatment cessation decisions are complex and multifaceted.
- Oncologists consider various factors when deciding to stop chemotherapy.
- Understanding treatment cessation can aid in informed decision-making.
- Cancer treatment efficacy and patient health are key considerations.
Understanding Why an Oncologist Stops Chemotherapy
Stopping chemotherapy is a big decision. It involves looking at many medical and personal factors. Oncologists think about these carefully before making their choice.
Medical Rationale Behind Treatment Cessation
Stopping chemotherapy often happens when it’s not working well or is causing too many side effects. If the cancer keeps growing or the treatment is too harsh, doctors might stop it.
Studies show that sometimes, keeping up with chemotherapy doesn’t help anymore. It could even hurt the patient because of the treatment’s side effects.
Balancing Benefits and Risks
Oncologists always weigh the good and bad of chemotherapy. If the bad outweighs the good, or if it’s not helping much anymore, they might stop it.
For example, some treatments can make cancer harder to fight. This can make future treatments less effective.
| Factors Influencing Decision | Description | Impact on Treatment |
| Disease Progression | Cancer continues to grow or spread despite chemotherapy. | May necessitate a change in treatment plan. |
| Severe Side Effects | Patient experiences significant adverse effects from chemotherapy. | Could lead to cessation of chemotherapy to improve quality of life. |
| Treatment Resistance | Cancer becomes resistant to the chemotherapy drugs being used. | May require switching to alternative treatments. |
Evidence-Based Decision Making
Oncologists use the latest research and guidelines to decide when to stop chemotherapy. They look at new studies and treatment plans.
This way, doctors can make choices that are best for their patients. They use their knowledge and the latest research together.
Common Reasons Why Chemotherapy Is Discontinued

Stopping chemotherapy is a complex decision. It involves many clinical and personal factors. Knowing why it happens is key for patients and their families.
Disease Progression Despite Treatment
One main reason for stopping chemotherapy is when the disease gets worse. If cancer keeps growing or spreading, doctors might stop treatment. High copper levels can make treatment less effective by causing DNA damage.
Severe or Unmanageable Side Effects
Chemotherapy can have strong side effects. If these effects become too much, doctors might stop treatment. This choice focuses on improving the patient’s quality of life.
Declining Overall Health Status
When a patient’s health starts to decline, chemotherapy might be stopped. Cancer and treatment can weaken the body. Doctors carefully decide when to stop treatment based on the patient’s condition.
“The goal of cancer treatment is not only to extend life but also to ensure that the remaining time is lived with dignity and minimal suffering.”
Completion of Planned Treatment Course
Chemotherapy can also stop when the planned treatment is finished. This is a sign of a successful treatment plan. Afterward, patients move to a new phase of care, watching for any signs of cancer coming back.
Understanding why chemotherapy stops can help patients and families. It shows the complex reasons behind these decisions. This knowledge helps in understanding treatment outcomes better.
The Oncologist’s Decision-Making Process
Deciding to stop chemotherapy is complex. It involves many medical and ethical aspects. Oncologists must think about the treatment’s benefits and risks. They consider the latest research and the patient’s unique situation.
Evaluating Treatment Response
How well the cancer responds to chemotherapy is key. They check if the tumor is getting smaller, staying the same, or growing. Regular tests and lab results are vital for this check.
A study found that copper plays a role in cancer growth and spread. This knowledge helps oncologists decide if treatment should continue or stop.
Considering Patient’s Quality of Life
Chemotherapy’s effect on the patient’s life is also important. Oncologists weigh the treatment’s benefits against its side effects. What the patient says about their life is very important.
“The goal of cancer treatment is not only to prolong life but also to maintain its quality.” This shows why the patient’s quality of life matters in treatment choices.
Consulting with Multidisciplinary Teams
Oncologists don’t make decisions alone. They work with teams like surgeons and radiologists. This teamwork ensures all important factors are looked at.
Weighing Ethical Considerations
Oncologists also think about ethics. They respect the patient’s choices, act in their best interest, avoid harm, and ensure fairness. This is about treating patients with dignity and respect.
By thinking about these points, oncologists make choices that put the patient first. They guide and support patients through tough times.
When Chemotherapy Is No Longer Effective
When chemotherapy stops working, patients and doctors face a big decision. This happens for many reasons, like the cancer becoming resistant or the patient’s health changing.
Recognizing Treatment Resistance
Treatment resistance happens when cancer cells get used to the drugs. Doctors use tests and scans to see if this is the case.
Spotting treatment resistance early is key. This means changing treatment plans or trying new options.
Understanding Cancer Adaptation
Cancer cells can change and keep growing even with treatment. High copper levels in cancer cells are linked to this. For example, in prostate cancer, high copper levels mean the disease is getting worse.
Knowing how cancer adapts helps doctors find better treatments. They might target specific ways cancer cells survive.
Measuring Risk-Benefit Ratio
When treatment stops working, doctors must think hard about what to do next. They look at side effects, quality of life, and treatment success chances.
At times, the risks of more treatment are too high. Doctors might suggest other ways to treat the cancer then.
Identifying Diminishing Returns
Knowing when treatment isn’t helping anymore is important. Doctors use many ways to check if treatment is working.
When treatment isn’t helping, doctors and patients look for new options. This could be targeted therapies or clinical trials.
Patient-Doctor Communication When Chemotherapy Ends
Talking openly with your doctor about stopping chemotherapy is key. When a doctor decides to stop treatment, it’s important to understand why. This helps you know what to expect next.
Having Difficult Conversations
Talking about stopping chemotherapy can be tough. Patients might feel many emotions. Doctors should be kind and clear in their explanations.
Key elements of effective communication include:
- Clear explanations of the reasons for stopping chemotherapy
- Discussion of alternative treatment options or clinical trials
- Emotional support and addressing patient concerns
- Involving family members or caregivers in the conversation as needed
Questions to Ask Your Oncologist
It’s important to ask questions during these talks. Here are some ideas:
- What are the primary reasons for stopping chemotherapy?
- Are there alternative treatments available?
- How will my condition be monitored after chemotherapy?
- What are the expected outcomes, and how can we manage symptoms?
| Question | Purpose |
| What are the primary reasons for stopping chemotherapy? | Understand the medical rationale |
| Are there alternative treatments available? | Explore other treatment options |
| How will my condition be monitored after chemotherapy? | Understand follow-up care |
Seeking Second Opinions
Getting a second opinion can offer new insights. It’s helpful when thinking about stopping chemotherapy.
Involving Family in Discussions
Having family or caregivers join the conversation helps. It offers emotional support and ensures everyone is on the same page.
Good communication between patients and doctors is vital. It helps make informed decisions about ending chemotherapy and what comes next.
Emotional Impact When Told “No More Chemo”
When an oncologist says no more chemo, patients feel a mix of emotions. It’s not just a medical choice. It affects their feelings and mind deeply.
Processing Grief and Disappointment
Stopping chemotherapy brings grief and disappointment. It’s normal, as chemo is a big part of treatment. Patients should let themselves feel these emotions and look for support.
- Allow yourself to grieve the loss of the treatment that has been a significant part of your life.
- Seek support from family, friends, or support groups who understand your experience.
- Consider counseling or therapy to process your emotions.
Managing Anxiety About the Future
Stopping chemo makes the future uncertain, causing anxiety. It’s important to manage this anxiety for emotional health.
Strategies for managing anxiety include:
- Staying informed about your condition and treatment options.
- Engaging in relaxation techniques such as meditation or deep breathing.
- Setting realistic goals and priorities for the future.
Supporting Family Members
Stopping chemo affects not just patients but their families too. It’s important to support them.
Supporting family can be done by:
- Openly discussing feelings and concerns.
- Involving them in decision-making processes.
- Encouraging them to seek support for themselves.
Finding Emotional Resilience
Building emotional resilience is key when stopping chemo. It’s about coping with emotions and adapting to new situations.
Building resilience can be achieved through:
- Practicing self-care and maintaining a healthy lifestyle.
- Engaging in activities that bring joy and fulfillment.
- Seeking professional help when needed.
Getting advice on stopping chemo is tough. But it opens up new treatment options and helps manage ending chemo side effects. Understanding the emotional impact and seeking support helps patients get through this tough time.
Alternative Treatment Options After Chemotherapy Ends
When chemotherapy stops, it’s time to look at other ways to treat cancer. Patients and doctors start to explore different treatments. These are chosen based on what the patient needs and their health.
Clinical Trials and Experimental Therapies
One option is to join clinical trials for new treatments. These trials help find better ways to fight cancer. They offer treatments that are not yet common.
- Investigational drugs that target specific cancer cells
- Immunotherapy approaches that boost the body’s immune response
- Combination therapies that pair different treatment modalities
Targeted Therapies and Immunotherapies
Targeted therapies and immunotherapies are big steps forward in cancer treatment. Targeted therapies aim at cancer cells without harming healthy ones. Immunotherapies help the body fight cancer better.
Elesclomol is a targeted therapy being studied. It helps copper ions get into cancer cells. This leads to more reactive oxygen species, slowing down tumor growth.
Integrative and Complementary Approaches
Along with traditional treatments, integrative and complementary approaches can help. These include changing your diet, practicing mind-body therapies, and using holistic practices. They aim to improve your overall health and treatment results.
- Nutritional counseling to optimize diet during treatment
- Mind-body practices such as meditation and yoga
- Acupuncture for symptom management
Maintenance Therapies
For some, maintenance therapies are recommended. They help keep treatment working or stop cancer from coming back. These treatments are less intense and can be used for a long time.
Choosing treatments after chemotherapy is very personal. It depends on the cancer type, past treatments, and health. It’s a big decision that needs careful thought and talking with doctors.
Support Systems and Resources
When an oncologist stops chemotherapy, patients need more than medical advice. They need a strong support system for their cancer journey. This support can be emotional, financial, or practical.
Coping with Emotional Challenges
Support groups and counseling are key for emotional support. They offer a safe place to share and learn from others. This helps patients cope with the emotional impact of stopping chemotherapy.
Many cancer support groups exist, both in-person and online. They provide a sense of community. For example, the American Cancer Society offers support groups, counseling, and educational materials.
Navigating Financial Considerations
Cancer treatment can be very expensive. But, there are financial aid programs to help with medical costs. This includes medication, hospital stays, and more.
The Cancer Financial Assistance Coalition (CFAC) helps patients find financial aid. Also, some pharmaceutical companies offer discounted or free medications to those who qualify.
Home Care and Hospice Services
Home care services are vital for ongoing care after chemotherapy. They offer nursing care, physical therapy, and help with daily tasks.
Hospice care is also important for advanced cancer patients. Hospice teams provide medical, emotional, and spiritual support to patients and their families.
Digital Resources and Communities
The internet offers a wealth of information and support. Online forums, social media groups, and cancer websites provide educational content and emotional support.
Digital tools can help manage care, like tracking medications and appointments. These tools empower patients to stay organized during their cancer journey.
Getting oncologist guidance post-chemo is essential. But, having access to support systems and resources greatly improves a patient’s quality of life. Support comes in many forms, from groups and financial aid to home care and digital tools.
Life After an Oncologist Stops Chemotherapy
Life after chemotherapy is a mix of relief, uncertainty, and new beginnings. Patients often feel many emotions and face challenges. This time is key for setting new goals, managing side effects, and finding purpose.
Setting New Goals and Priorities
After treatment ends, patients should rethink their priorities and goals. This helps them regain control and direction. Goal setting can cover personal, professional, and health goals, based on what they can do now.
Managing Long-term Side Effects
Dealing with chemotherapy’s long-term side effects is vital. Patients might face fatigue, neuropathy, or cognitive changes. To manage, they can try physical therapy, cognitive rehabilitation, and medication for symptoms.
| Side Effect | Management Strategy |
| Physical Fatigue | Graded Exercise Therapy, Rest and Relaxation Techniques |
| Neuropathy | Medications (e.g., Gabapentin), Physical Therapy |
| Cognitive Changes | Cognitive Rehabilitation, Memory Aids |
Finding Meaning and Purpose
Finding meaning and purpose is a personal journey. Patients look for new ways to connect, help others, or find joy. This might mean joining support groups, volunteering, or exploring creative pursuits.
Celebrating Life Milestones
Celebrating milestones is part of healing. Patients should mark their progress, like treatment completion or birthdays. These moments help them feel accomplished and hopeful for the future.
Recent studies show copper’s role in prostate cancer growth. Research into copper metabolism might lead to new treatments. Understanding copper’s impact on prostate cancer helps manage the disease after chemotherapy.
How to Prepare for Follow-up Care
The time after chemotherapy is very important. Getting ready for follow-up care helps keep you healthy and tackles any new problems fast. It’s key to know what makes up good care after treatment.
Ongoing Monitoring and Appointments
Seeing your oncologist regularly is a must. It helps keep an eye on your health and spots problems early. These visits might include:
- Physical checks to see how you’re doing
- Imaging tests (like CT scans, MRI) to check on the disease
- Lab tests to look at tumor markers or other health signs
Ongoing monitoring is important. It helps manage side effects and tackles any worries or symptoms quickly.
Symptom Management Strategies
Handling symptoms well is a big part of follow-up care. This means:
- Spotting and writing down symptoms
- Finding ways to deal with these symptoms, like medicine or lifestyle changes
- Checking and changing symptom plans as needed
Knowing about glutathione and how it affects copper levels is also helpful. Studies show that less glutathione can raise copper levels inside cells, which can harm cells.
Creating a Survivorship Care Plan
A survivorship care plan outlines your care after treatment. It covers:
- A summary of your treatment
- A plan for follow-up care, like appointments and tests
- Ways to handle late effects of treatment
- How to get support services
Having such a plan ensures your care is well-coordinated. This improves your health and quality of life.
Building Your Healthcare Team
It’s important to build a team of healthcare professionals for follow-up care. This team might include:
- Your oncologist and primary care doctor
- Nurses and nurse practitioners
- Experts in areas like cardiology or psychology
- Support staff, like social workers and nutritionists
Building a strong healthcare team means you get care that covers all your needs. This includes physical, emotional, and practical support.
Conclusion
When an oncologist stops chemotherapy, it’s a big decision. It shows they’ve carefully thought about the patient’s health and treatment choices. They might stop chemotherapy if the disease is getting worse, if side effects are too severe, or if the treatment plan is complete.
Stopping chemotherapy can be tough for patients. It affects their emotions and mental health. It’s important for patients to understand why their oncologist made this choice. This helps them deal with their care better.
Scientists are always looking for new ways to fight cancer. They’re studying things like copper ion carriers to kill cancer cells. But, more research is needed to see if these methods work well for different types of cancer.
After stopping chemotherapy, patients need to focus on their care. They should manage symptoms and take care of their overall health. Knowing about cancer treatment and why chemotherapy might stop can help patients make good choices for their care.
FAQ
Why does an oncologist decide to stop chemotherapy?
An oncologist might stop chemotherapy if the disease gets worse, if side effects are too severe, or if the patient’s health declines. They also stop if the treatment plan is complete. The decision is based on a detailed look at the patient’s health and how they’re responding to treatment.
What factors influence an oncologist’s decision to discontinue chemotherapy?
The oncologist looks at the patient’s health, how well they’re responding to treatment, and their quality of life. They also consider the risks and benefits of continuing treatment. Sometimes, they’ll talk to a team of experts to make the best choice.
How is treatment resistance recognized, and what are the implications?
Treatment resistance is spotted by checking how the patient is doing and how they’re reacting to treatment. If resistance is found, the oncologist might look into other treatments. This could include targeted therapies or joining a clinical trial.
What are the emotional implications for patients when chemotherapy is stopped?
Stopping chemotherapy can make patients feel sad, anxious, and unsure. It’s important to talk openly with the oncologist. Patients should also reach out to family, friends, and support groups for help.
What alternative treatment options are available after chemotherapy ends?
After chemotherapy, patients might look into clinical trials, targeted therapies, or immunotherapies. They might also explore integrative approaches or maintenance therapies. The oncologist will help pick the best option based on the patient’s situation.
How can patients prepare for follow-up care after chemotherapy?
Patients should understand what follow-up care will involve. They should manage symptoms and create a care plan. Building a healthcare team is also key. This helps ensure they get the best care after treatment.
What role does copper play in cancer treatment and tumor biology?
Copper is being studied for its role in cancer. It might help in treating tumors. Researchers are looking at copper ion transporters, like Elesclomol, as possible treatments.
How can patients manage long-term side effects after chemotherapy?
Patients can work with their healthcare team to handle long-term side effects. This might include medication, lifestyle changes, or alternative therapies. The goal is to improve their quality of life.
What support systems and resources are available to patients after chemotherapy?
Patients can find support through groups, counseling, and financial help. Home care services and digital resources are also available. These can help them deal with life after chemotherapy.
How can patients find emotional resilience after being told “no more chemo”?
Patients can find emotional strength by talking to loved ones and joining support groups. They can also seek help from mental health professionals. Focusing on new goals and activities can help them cope emotionally.
Reference
- Prigerson, H. G., Bao, Y., Shah, M. A., Paulk, M. E., LeBlanc, T. W., Schneider, B. J., et al. (2015). Chemotherapy use, performance status, and quality of life at the end of life. JAMA Oncology, 1(6), 778“784. https://pubmed.ncbi.nlm.nih.gov/26181822/