Last Updated on December 1, 2025 by Bilal Hasdemir

Cancer diagnosis and treatment have become more complex. Over 1.8 million new cases are expected in the United States each year. Understanding the various treatment options for cancer is crucial for effective care.
The three main cancer treatment specialties are medical oncology, surgical oncology, and radiation oncology. Each one has its own way of diagnosing and treating cancer.
Medical oncology uses medication to fight cancer. Surgical oncology removes tumors through surgery. Radiation oncology kills cancer cells with high-energy radiation.
Key Takeaways
- There are three main types of oncology: medical oncology, surgical oncology, and radiation oncology.
- Each specialty has a distinct approach to cancer diagnosis and treatment.
- Understanding these differences is key for effective cancer care.
- Medical oncology involves using medication to treat cancer.
- Surgical oncology focuses on the surgical removal of tumors.
Understanding Oncology: The Study and Treatment of Cancer

Oncology focuses on combating cancer, a complex and multifaceted disease. It needs a full care approach. Many disciplines come together to help patients the best they can.
Definition and Scope of Oncology
Oncology is the study, diagnosis, treatment, and prevention of cancer. It’s a field that uses many medical specialties. This way, it meets the varied needs of cancer patients.
It’s not just about treating cancer. It also looks into why it happens and how to stop it.
The Historical Development of Cancer Treatment
Cancer treatment has changed a lot over time. It started with surgery and has grown to include many new therapies. Now, we have radiation, chemotherapy, and targeted treatments.
These new methods have changed how we care for cancer patients. They offer more options based on each patient’s needs.
The Importance of Specialized Cancer Care
Specialized cancer care is key to better patient results. Oncologists focus on certain cancers or treatments. This specialized approach enhances treatment effectiveness by targeting specific cancer types and patient needs.
Understanding cancer’s complexity is vital. It requires knowledge of tumor biology, genetics, and new treatments.
In summary, oncology is essential in the fight against cancer. Its many disciplines and treatments work together for full care. The history of cancer treatment and the need for specialized care show our ongoing efforts to better manage cancer and help patients.
Oncology Types: Medical, Surgical, and Radiation

Oncology is divided into three main areas: medical, surgical, and radiation oncology. These fields work together to give complete cancer care. They meet the varied needs of patients. Our essential guide to the 3 main oncology types. Discover the critical, amazing differences between medical, surgical, and radiation.
Classification of Oncology Specialties
Oncology specialties are grouped by their treatment methods. Medical oncology uses treatments like chemotherapy and targeted therapy. Surgical oncology removes tumors through surgery. Radiation oncology kills cancer cells with ionizing radiation.
| Oncology Specialty | Treatment Modalities |
| Medical Oncology | Chemotherapy, Targeted Therapy, Immunotherapy |
| Surgical Oncology | Surgical Removal of Tumors |
| Radiation Oncology | External Beam Radiation, Brachytherapy |
Multidisciplinary Approach to Cancer Care
A team effort is key in cancer care. It combines different specialties for effective plans. This teamwork ensures care fits each patient’s needs.
“The multidisciplinary team approach is essential in oncology. It brings together experts for the best care for cancer patients.”
How Treatment Plans Incorporate Multiple Specialties
Treatment plans often use many oncology specialties. For example, a patient might have surgery, then chemotherapy and radiation. This mix improves treatment results and survival chances.
Knowing about oncology’s types helps healthcare providers give better care. The division into medical, surgical, and radiation specialties leads to better patient results. It shows the importance of teamwork in cancer treatment.
Medical Oncology: Systemic Treatment Approaches
Systemic treatments have changed how we fight cancer. Medical oncology is all about treating cancer with treatments that affect the whole body.
Role and Responsibilities of Medical Oncologists
Medical oncologists are key in cancer care. They diagnose and treat cancer with systemic treatments. They plan treatments, give chemotherapy, and care for patients during treatment.
Key Responsibilities:
- Creating treatment plans tailored to each patient
- Managing systemic therapies like chemotherapy and targeted treatments
- Checking how treatments work and making changes as needed
- Helping with side effects to make treatment easier
Chemotherapy and Drug-Based Treatments
Chemotherapy is a mainstay in cancer treatment. Doctors use different drugs to kill cancer cells. They choose the best chemotherapy plan based on the cancer type, stage, and patient’s health.
The table below shows some common chemotherapy drugs and their uses:
| Drug | Cancer Type | Administration |
| Doxorubicin | Breast, bladder, lymphoma | Intravenous |
| Cisplatin | Testicular, ovarian, lung | Intravenous |
| 5-Fluorouracil | Colorectal, breast, skin | Intravenous or topical |
Immunotherapy and Targeted Therapies
Medical oncology also includes immunotherapy and targeted therapies. These treatments are more precise and may have fewer side effects. Immunotherapy boosts the body’s fight against cancer. Targeted therapies attack specific cancer growth points.
Immunotherapies like checkpoint inhibitors and CAR T-cell therapy are promising. Targeted therapies, like tyrosine kinase inhibitors, help patients with certain genetic changes.
Surgical Oncology: Removing Cancer Through Operation
Surgical oncologists focus on removing cancers through surgery. They use different methods to help patients get better. They work with other doctors to give complete care.
Functions of Surgical Oncologists
Surgical oncologists check if surgery is right for patients. They remove tumors and affected tissues. Their goal is to get rid of cancer and keep as much normal tissue as they can.
Key responsibilities include:
- Preoperative evaluation and planning
- Surgical removal of tumors and affected tissues
- Intraoperative decision-making to ensure optimal outcomes
- Postoperative care and follow-up
Types of Cancer Surgeries
Cancer surgeries differ based on the cancer type, stage, and patient’s health. Here are some common ones:
| Type of Surgery | Description | Examples |
| Curative Surgery | Aim is to remove all cancerous tissue | Mastectomy for breast cancer, colectomy for colon cancer |
| Palliative Surgery | Relieves symptoms, improves quality of life | Relieving obstruction in gastrointestinal cancer |
| Diagnostic Surgery | Obtains tissue for diagnosis | Biopsy procedures |
Minimally Invasive Techniques in Cancer Surgery
Minimally invasive surgery has changed cancer surgery a lot. It offers smaller cuts, less pain, and faster healing. Laparoscopic and robotic-assisted surgeries are examples.
Using these new methods, surgical oncologists can offer better treatments. These treatments help patients recover faster and get better results.
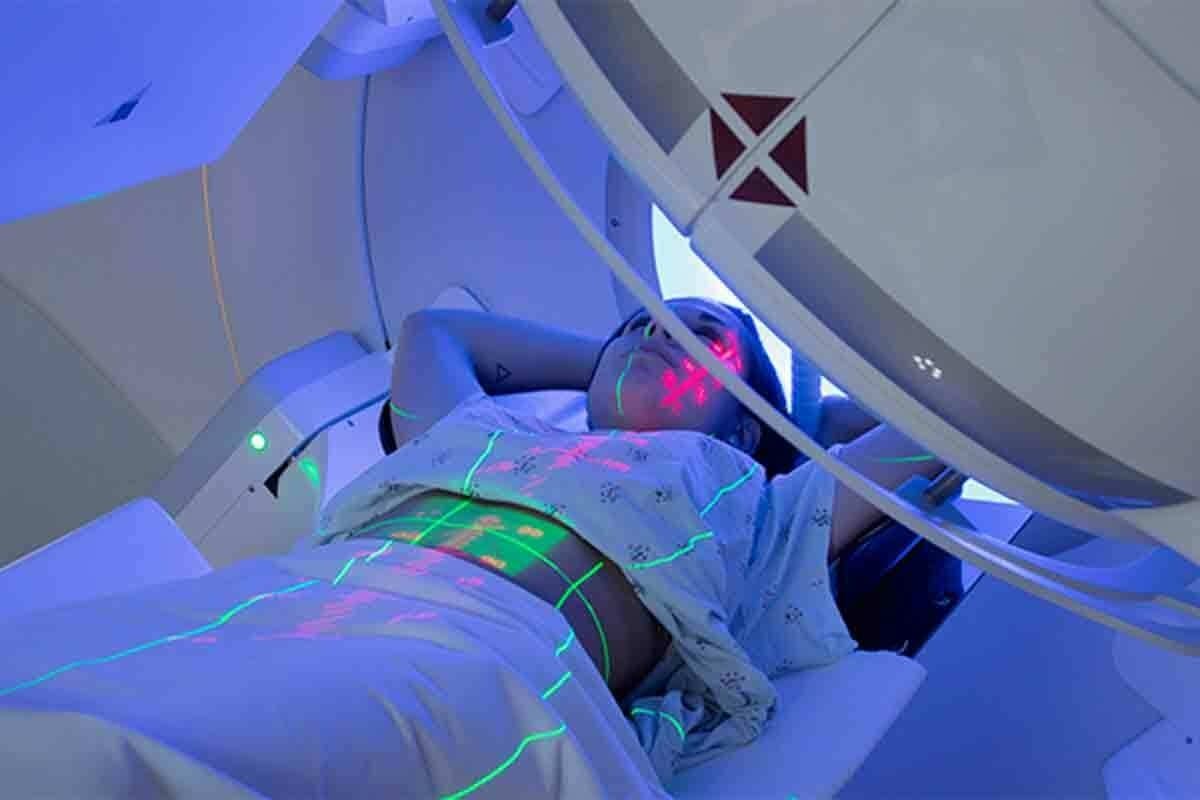
Radiation Oncology: Treating Cancer with Ionizing Radiation
Radiation oncology is a key part of fighting cancer. It uses ionizing radiation to treat cancer. Each patient gets a treatment plan that fits their needs.
How Radiation Oncologists Work
Radiation oncologists team up with other cancer experts. They figure out the best radiation therapy for each patient. They consider the cancer type and stage.
Key responsibilities of radiation oncologists include:
- Evaluating patient suitability for radiation therapy
- Designing and implementing personalized treatment plans
- Monitoring patient response to treatment and adjusting plans as necessary
External Beam Radiation Therapy
External beam radiation therapy (EBRT) is a common method. It uses beams from outside the body to kill cancer cells.
EBRT can be further categorized into several types, including:
- 3D conformal radiation therapy
- Intensity-modulated radiation therapy (IMRT)
- Stereotactic body radiation therapy (SBRT)
Brachytherapy and Other Radiation Approaches
Brachytherapy places radioactive material close to the tumor. It treats the area with less harm to nearby tissues.
Other methods include total body irradiation (TBI) and intraoperative radiation therapy (IORT). Each has its own use and benefits.
Radiation oncology keeps getting better. New tech and techniques help cancer patients get better care.
Integration of the Three Oncology Types in Treatment Plans
Combining medical, surgical, and radiation oncology is key for good cancer treatment plans. This team effort makes sure patients get care that fits their needs perfectly.
Neoadjuvant and Adjuvant Therapy Concepts
Neoadjuvant therapy is given before the main treatment, and adjuvant therapy is after. These can include chemotherapy, radiation, or hormone therapy. They help shrink tumors or get rid of cancer cells left behind.
Tumor Boards and Collaborative Decision Making
Tumor boards are where experts from different oncology fields meet. They talk about patient cases and make collaborative treatment plans. This way, they consider all important factors for better tumor treatment.
Case Studies of Integrated Treatment Approaches
Many case studies show the good results of mixing different oncology types. For example, a stage III breast cancer patient might get chemotherapy first, then surgery, and lastly radiation. These combined methods have led to better results in cancer care types.
It’s important to mix oncology research and services to improve oncology services and patient results. By working together, doctors can give more tailored and effective treatments.
Specialized Oncology Fields Beyond the Main Types
Oncology is a wide field with many specialized areas. Each area focuses on different cancers and patient needs. These fields have grown to offer more precise and effective care for various cancers.
Gynecologic Oncology
Gynecologic oncology deals with cancers of the female reproductive system. This includes ovarian, cervical, and uterine cancers. Gynecologic oncologists use surgery and medicine to manage these cancers. Minimally invasive surgery has led to better patient outcomes.
Pediatric Oncology
Pediatric oncology treats cancers in children, like leukemia and brain tumors. Pediatric oncologists use treatments like chemotherapy and surgery. Survivorship care is key, focusing on long-term health.
Neuro-oncology
Neuro-oncology focuses on brain and spinal cord tumors. Neuro-oncologists work with neurosurgeons and radiation oncologists. Advances in radiation therapy and targeted therapies have helped patients with brain tumors.
Urologic Oncology
Urologic oncology treats cancers of the urinary tract, such as prostate and bladder cancers. Urologic oncologists use surgery and medicine, including robotic surgery and immunotherapy. Early detection and treatment have greatly improved survival rates.
| Specialized Field | Cancers Focused On | Key Treatments |
| Gynecologic Oncology | Ovarian, Cervical, Uterine | Surgery, Chemotherapy |
| Pediatric Oncology | Leukemia, Lymphoma, Brain Tumors | Chemotherapy, Radiation, Surgery |
| Neuro-oncology | Brain, Spinal Cord Tumors | Radiation, Targeted Therapies |
| Urologic Oncology | Prostate, Bladder, Kidney | Surgery, Immunotherapy |
These specialized fields show the complexity and diversity of cancer care. They highlight the need for a team approach to treatment.
Hematologic Oncology: Treating Blood Cancers
Hematologic oncology has made big strides in fighting blood cancers. Doctors in this field focus on diagnosing and treating blood cancers like leukemia, lymphoma, and myeloma. These cancers are complex and need a detailed treatment plan.
Leukemia, Lymphoma, and Myeloma Treatment
Treatment for blood cancers depends on the type and stage. For example, leukemia treatment often includes chemotherapy and targeted therapy. Lymphoma treatment might involve chemotherapy, radiation, and immunotherapy. Myeloma treatment could include these methods, plus stem cell transplantation.
Innovative treatments are being developed to better patient outcomes. For example, CAR T-cell therapy is showing promise in treating some lymphomas and leukemias.
Stem Cell Transplantation
Stem cell transplantation is a key treatment for blood cancers. It replaces damaged stem cells with healthy ones. This helps the bone marrow make normal blood cells. The procedure can use the patient’s own stem cells or donor stem cells.
CAR T-Cell Therapy and Innovative Approaches
CAR T-cell therapy is a type of immunotherapy. It modifies a patient’s T-cells to attack cancer cells. This treatment has shown great promise in clinical trials, giving hope to patients with certain blood cancers.
Other new approaches include targeted therapies and bispecific antibodies. These are designed to target cancer cells while protecting healthy tissues.
The Role of Pathology in Guiding Oncology Treatment
Getting a precise cancer diagnosis is key to good oncology treatment. Pathology helps understand cancer’s details. This lets oncology specialists create targeted treatment plans.
Cancer Diagnosis and Classification
The journey starts with cancer diagnosis and sorting it out. Pathologists look at tissue samples. They figure out if there’s cancer, what type, and how far it has spread. This info is vital for picking the right treatment.
Molecular Pathology and Precision Medicine
Molecular pathology has changed oncology a lot. It makes precision medicine possible. Pathologists study tumor genetics to find specific mutations. This helps target therapies to those mutations.
Biomarkers and Treatment Selection
Biomarkers are key in choosing treatments. They show how a patient might react to certain treatments. This leads to more personalized cancer care. Oncology research keeps finding new biomarkers, making treatments better.
In short, pathology is essential in guiding oncology treatment. It ensures patients get the best care through accurate diagnosis, molecular analysis, and biomarker use.
Cancer Staging and Its Impact on Treatment Selection
Cancer staging is key to planning treatment. It tells us how far the cancer has spread. This is vital for knowing the outlook and choosing the right treatment.
TNM Classification System
The TNM system is a common way to stage cancer. It looks at three main things: the tumor size (T), lymph node involvement (N), and if it has spread (M). This system makes it easier for doctors to talk about cancer in a standard way.
The TNM system is important for:
- Understanding how far the cancer has spread
- Choosing the best treatment
- Estimating how the cancer will progress
- Helping in research and comparing data
How Staging Determines Treatment Approach
The stage of cancer is key in picking the right treatment. Doctors use the stage to decide if surgery or radiation is best. Or if the cancer has spread and needs treatments like chemotherapy or immunotherapy.
For example, early-stage cancers might be treated with:
- Surgery alone
- Radiation therapy
- A mix of both
For more advanced cancers, treatments are more complex.
Stage-Specific Protocols Across Oncology Types
Each type of cancer has its own treatment plans based on the stage. In medical oncology, the stage helps choose between chemotherapy, targeted therapy, or immunotherapy. In surgical oncology, the stage affects how much surgery is possible.
In radiation oncology, the stage helps decide the radiation dose and area. Knowing these specific plans is key for effective care.
Emerging Technologies Transforming Oncology Types
The world of oncology is changing fast with new technologies. These new tools are making cancer treatments better and opening up new ways to care for patients.
Artificial Intelligence in Cancer Diagnosis
Artificial intelligence (AI) is making a big impact in oncology. It helps doctors make more accurate diagnoses and tailor treatments to each patient. AI looks at lots of medical data, like images and genes, to find things humans might miss.
Robotic Surgery Advancements
Robotic surgery is changing surgical oncology. It brings more precision, flexibility, and control to operations. This means surgeons can do complex surgeries with less effort, helping patients recover faster and do better.
Proton Therapy and Advanced Radiation Techniques
Proton therapy is a big step forward in radiation oncology. It targets tumors precisely, protecting healthy tissues. Other new radiation methods, like IMRT, are also making treatments more effective.
Liquid Biopsies and Non-invasive Monitoring
Liquid biopsies are a new way to check on cancer without invasive tests. They look at DNA in blood to see how cancer is growing and responding to treatment. This could change how we manage cancer, giving us instant insights into tumors.
| Technology | Application in Oncology | Benefits |
| Artificial Intelligence | Diagnostic accuracy, personalized treatment | Enhanced pattern recognition, improved patient outcomes |
| Robotic Surgery | Surgical oncology | Precision, reduced recovery time |
| Proton Therapy | Radiation oncology | Precise tumor targeting, minimized collateral damage |
| Liquid Biopsies | Cancer monitoring, treatment response | Non-invasive, real-time insights into tumor genetics |
These new technologies are changing oncology in big ways. They offer new ways to find, treat, and watch cancer. As they keep getting better, they promise to make cancer care even better for patients.
Oncology Research: Advancing Cancer Treatment Methods
Oncology research is key in improving cancer treatments, giving hope to patients everywhere. It keeps evolving thanks to new research in clinical trials, translational research, and precision medicine.
Clinical Trials and Experimental Therapies
Clinical trials are vital in oncology research. They help test new cancer treatments for safety and effectiveness. This leads to the creation of new therapies, like targeted treatments and immunotherapies, which are transforming cancer care.
Types of Clinical Trials:
- Phase I: Focus on safety and dosing
- Phase II: Evaluate efficacy and side effects
- Phase III: Compare new treatments with standard therapies
Translational Research in Oncology
Translational research connects scientific discoveries to clinical use in oncology. It speeds up the creation of new treatments by applying lab findings to patient care. This deepens our understanding of cancer biology.
Precision Medicine and Personalized Treatment
Precision medicine is a big leap forward in oncology. It tailors treatments to each patient’s unique cancer characteristics. By looking at genetic and molecular data, doctors can pick the best treatments. This improves results and lowers side effects.
| Aspect | Traditional Approach | Precision Medicine Approach |
| Treatment Selection | Based on cancer type and stage | Based on genetic and molecular profiling |
| Therapeutic Focus | Generalized treatments | Targeted therapies |
Careers and Education in Different Oncology Types
Oncology is a branch of medicine focused on cancer treatment. It offers many career paths that need specialized education and training. As cancer treatment advances, the need for skilled oncology professionals grows.
Education and Training Requirements
Careers in oncology start with a strong educational base. This usually includes medical school and then specialized training in oncology. For example, medical oncologists need a fellowship in medical oncology after their internal medicine residency. Radiation oncologists also get specialized training.
Subspecialization Opportunities
Oncology offers many chances for subspecialization. Gynecologic oncology deals with cancers of the female reproductive system. Pediatric oncology focuses on cancer in children. These areas need extra training and knowledge.
Interdisciplinary Collaboration Skills
Oncology professionals must work well in teams. They collaborate with surgeons, radiologists, and others to give full care. Good communication and teamwork skills are key to success in this field.
To thrive in oncology careers, one must keep learning and growing. Staying updated with the latest in clinical oncology and oncology services is vital.
The Patient Journey Through Different Oncology Types
Cancer patients face a complex journey through various oncology services. Their path is not simple. It involves many specialists and treatments.
Navigating Multiple Specialists
Patients with cancer see many oncology experts. They meet medical oncologists, surgical oncologists, and radiation oncologists. A team approach is key for effective tumor treatment.
Supportive Care and Survivorship
Supportive care is critical in the patient’s journey. It helps manage side effects and boosts quality of life. Survivorship programs aid in the transition back to normal life.
Patient Advocacy and Shared Decision Making
Patient advocacy ensures patients get the right care. It’s important for patients, families, and doctors to make decisions together. This way, cancer care types are tailored to each patient’s needs and values.
Understanding and navigating oncology services helps patients get the care they need. It’s about addressing their unique health needs.
Global Perspectives and Access to Oncology Services
Worldwide, the quality and availability of cancer care vary a lot. This affects how well cancer is treated. Many factors play a role, like the state of healthcare, the economy, and access to new treatments.
Disparities in Cancer Care Worldwide
There are big differences in cancer care around the world. Low- and middle-income countries struggle with limited access to screening and treatment. This leads to more deaths compared to richer countries with better cancer care.
Differences in Oncology Practice Internationally
Oncology practices differ because of healthcare policies and technology adoption. For example, some countries quickly adopted immunotherapy and targeted therapy. This changes treatment plans and patient results.
Initiatives to Improve Global Cancer Treatment
Many efforts aim to fix these disparities. There are global research collaborations, projects to increase screening and treatment access, and guidelines for cancer care. These can fit different healthcare systems.
Conclusion: The Future of Oncology and Cancer Care
The future of fighting cancer looks bright. This is thanks to ongoing research and the growth of precision medicine. Cancer treatments are getting better and more focused.
Precision medicine is changing how we treat cancer. It makes treatments fit each patient’s needs. This new approach, along with the latest research, is making a big difference in patient care.
As we look ahead, combining different cancer specialties will be key. This mix will help give patients the best care possible. New research and a focus on personalized treatment will keep improving cancer care.
Thanks to research and precision medicine, we’re getting closer to better cancer treatments. There’s hope for even better care for patients in the future.
FAQ
What are the three main types of oncology?
Oncology has three main types: medical, surgical, and radiation oncology. These work together for full cancer care.
What is the role of a medical oncologist in cancer treatment?
Medical oncologists use treatments like chemotherapy and immunotherapy to fight cancer. They help diagnose and treat it.
How does surgical oncology differ from other types of oncology?
Surgical oncologists remove tumors through surgery. They work with others to plan treatments that might include surgery.
What is radiation oncology, and how is it used in cancer treatment?
Radiation oncology uses radiation to treat cancer. Specialists in this field help plan treatments that include radiation therapy.
What is hematologic oncology, and what types of cancer does it involve?
Hematologic oncology deals with blood cancers like leukemia and lymphoma. It’s a part of oncology.
How do oncologists determine the stage of cancer, and why is it important?
Oncologists use the TNM system to stage cancer. This system looks at the tumor, lymph nodes, and if it has spread. Knowing the stage helps plan treatment and predict outcomes.
What is precision medicine, and how is it used in oncology?
Precision medicine tailors treatments to a patient’s tumor. It uses biomarkers and genetic tests to guide treatment.
What are some emerging technologies transforming oncology?
New technologies like AI and robotic surgery are changing oncology. They help diagnose and treat cancer better.
How do different oncology specialties work together in cancer care?
Oncology specialties work together in a team effort. They collaborate to create detailed treatment plans.
What is the role of pathology in guiding oncology treatment?
Pathology is key in cancer diagnosis and treatment. Pathologists examine samples to determine cancer type and stage. Molecular pathology guides targeted therapies.
What are some specialized oncology fields beyond the main types?
There are many specialized fields like gynecologic and pediatric oncology. These focus on specific cancers or patient groups.
How do oncologists stay current with the latest advancements in cancer treatment?
Oncologists keep up with new treatments through education and research. They attend conferences and join clinical trials.
References
World Health Organization. Evidence-Based Medical Insight. Retrieved from https://www.who.int/news-room/fact-sheets/detail/cancer