Last Updated on November 27, 2025 by Bilal Hasdemir

Cardiac surgery is a complex field. It includes procedures that can save lives but are also very hard. Did you know that open heart surgery accounts for a significant portion of major surgeries performed worldwide? This shows how important and complex cardiothoracic surgery is.
We see many cardiac surgeries, like coronary artery bypass grafting and heart transplantation. Each one has its own challenges and complexities. The difficulty comes from the patient’s health, the procedure’s complexity, and the need for precision.
Exploring cardiothoracic surgery, we find some procedures are more complex and risky. In this article, we’ll look into cardiac surgeries and what makes some of them very hard.
Key Takeaways
- Cardiac surgery includes many complex procedures.
- The difficulty of cardiac surgeries depends on several factors.
- Coronary artery bypass grafting and heart transplantation are among the most complex.
- The procedure’s intricacy and the patient’s health are key in determining difficulty.
- Understanding cardiac surgery challenges is vital for improving medical practices.
The Complexity Spectrum of Cardiac Surgery
It’s key for surgeons and patients to grasp the complexity of cardiac surgery. This field includes many procedures, from simple to very complex. The complexity depends on the patient’s health, any other health issues, and the surgery type.
Factors That Determine Surgical Difficulty
Several factors make a cardiac surgery hard. Patient-specific factors like age and health status matter. So do any other health problems, like diabetes or high blood pressure.
The heart’s anatomy and the surgery’s purpose also affect the difficulty. For example, fixing complex heart defects is tougher than treating heart disease.
Surgical technique is also key. Choosing between open-heart surgery and less invasive methods changes the surgery’s complexity. Using cardiopulmonary bypass or off-pump techniques can make things easier or harder, depending on the situation.
Risk Assessment in Cardiac Procedures
Assessing risk is critical in planning cardiac surgery. Surgeons use models like EuroSCORE or STS Score to predict risks. These models look at patient demographics, health status, and the surgery details.
Good risk assessment helps surgeons choose the best treatment for each patient. It also helps in talking to patients and their families about surgery risks and benefits. Knowing the complexity and risks helps tailor care to each patient, improving surgery outcomes.
Open Heart Surgery: The Foundation of Cardiac Interventions

Open heart surgery has been key in treating heart issues for many years. It lets surgeons fix complex heart problems directly. This was not possible before.
Exploring open heart surgery, we see its core ideas and history. It involves opening the chest to reach the heart. This lets surgeons see and work on the heart’s parts.
Definition and Basic Concepts
Open heart surgery means opening the chest to work on the heart. It gives surgeons a clear view and access. They can do detailed repairs and interventions.
Cardiopulmonary bypass (CPB) is a key part of many surgeries. It stops blood flow to the heart and lungs. This makes the heart and lungs quiet and bloodless for surgery.
Historical Development of Open Heart Techniques
The history of open heart surgery is one of innovation and hard work. The first successful surgery was in the late 1950s. It started a new chapter in heart care.
Over time, open heart surgery has grown. It now includes many procedures like CABG and valve repairs. These advancements have greatly improved patient outcomes and quality of life.
Open heart surgery keeps getting better. Ongoing research aims to make surgery safer and recovery faster. It’s clear that open heart surgery will keep being a major part of heart care, helping patients all over the world.
Coronary Artery Bypass Grafting (CABG)
Coronary Artery Bypass Grafting, or CABG, is a key surgery for those with severe heart disease. It helps by bypassing blocked arteries to improve blood flow to the heart.
Procedure Overview and Variations
CABG uses a graft, often from the saphenous vein or internal mammary artery, to bypass blocked arteries. The method can change based on how many arteries need fixing and the technique used.
Doctors might use traditional on-pump or newer off-pump CABG methods. The choice depends on the patient’s health and the surgeon’s skills.
Technical Challenges for Surgeons
One big challenge in CABG is attaching the graft correctly. Surgeons also face issues like graft failure or heart rhythm problems.
Dealing with these issues is harder when patients have many blockages or need more heart repairs.
Off-Pump vs. On-Pump CABG
The choice between off-pump and on-pump CABG is ongoing. Off-pump might lower the risk of some complications by not using a heart-lung machine.
On-pump CABG offers a clearer view of the heart, which helps in complex cases. The decision depends on the patient’s health and their heart disease specifics.
We know CABG can be scary for patients. Our team is here to offer full care and support every step of the way.
Heart Valve Replacement and Repair
Heart valve replacement and repair are key surgeries for valvular heart disease. They help the heart work better and improve life quality.
Valvular heart disease includes stenosis, regurgitation, and mixed valve disease. Whether to repair or replace a valve depends on disease type, severity, patient age, and health.
Mitral Valve Complex Reconstructions
The mitral valve is vital for heart function. Repairing the mitral valve is often chosen over replacement. This keeps the natural valve and avoids lifelong anticoagulation therapy.
“Mitral valve repair is a highly effective treatment for degenerative mitral regurgitation, with excellent long-term outcomes,” studies say.
Aortic Valve Procedures
Aortic valve disease requires surgery. Aortic valve replacement (AVR) uses mechanical or bioprosthetic valves. The choice depends on patient age, lifestyle, and anticoagulation therapy risks.
Transcatheter aortic valve replacement (TAVR) is a less invasive option. It’s good for high-risk or inoperable patients, with fewer complications and quicker recovery.
Multiple Valve Surgeries
Some patients need surgery for multiple valve diseases. These surgeries are complex, requiring careful planning and precise technique.
Advanced imaging, like 3D echocardiography, helps plan these surgeries. It lets surgeons see the heart valves’ complex anatomy and plan better.
Cardiac surgery is getting better, leading to better patient outcomes and life quality.
Heart Transplantation: The Ultimate Challenge
The journey of heart transplantation is filled with challenges. It starts with finding the right donor and ends with caring for the recipient. This process is a lifesaver for those with failing hearts.
Donor Selection and Organ Preservation
Finding the right donor is key to a successful transplant. We look at the donor’s health and how well their heart works. Organ preservation is also vital to keep the heart alive during the transplant.
We check the donor’s medical history for any risks. We also examine their heart for any problems. This helps ensure the heart will work well for the recipient.
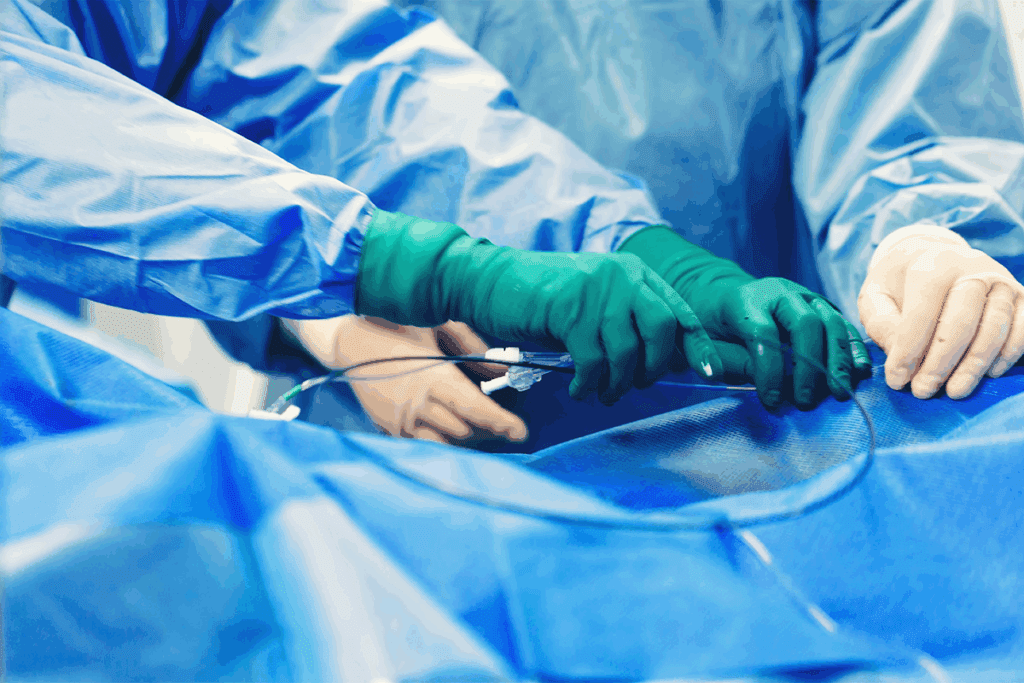
Surgical Technique and Timing Constraints
The surgical technique for heart transplants is very precise. The diseased heart is removed and replaced with a healthy one. The goal is to keep the donor heart alive as long as possible.
Surgeons plan the surgery carefully. They work with the team that gets the donor heart to make sure everything goes smoothly. The surgery is complex and requires a lot of skill.
Post-Transplant Management Complexities
After the transplant, post-transplant management is very important. Patients need to be watched closely for any problems. They also need to take medicine to prevent their body from rejecting the new heart.
Long-term care includes regular check-ups and adjusting the medicine as needed. We teach patients how to live a healthy lifestyle to reduce risks. This helps them stay well and avoid complications.
Aortic Dissection and Aneurysm Repair
Aortic dissection and aneurysm repair need quick and precise surgery. These complex conditions require a skilled surgical team.
Emergency Nature and Time Sensitivity
Aortic dissection happens when there’s a tear in the aorta’s inner layer. Blood flows between the layers, leading to serious complications. If not treated fast, it can be deadly.
It’s vital to act quickly because the time for treatment is short. Every minute is critical in treating aortic dissection.
Surgical Approaches to the Aortic Arch
The aortic arch is a key area where the aorta curves. It supplies blood to the head and arms. Surgery here is tough because of its complex anatomy.
Surgical techniques might include replacing the aortic arch with a graft. The choice depends on the disease’s extent and the patient’s health.
Endovascular vs. Open Techniques
Endovascular techniques are a new option for some aortic aneurysms or dissections. They involve placing a stent-graft through arteries to block the damaged area.
Endovascular methods have benefits like less recovery time and less trauma. But, open surgery is often the best choice for complex cases. The right approach depends on the patient’s condition and the aortic problem’s details.
Congenital Heart Defect Corrections in Pediatric Patients
Fixing congenital heart defects in kids is tough. These defects are heart problems kids are born with. They can be simple or very complex, needing surgery.
Hypoplastic Left Heart Syndrome Repair
Hypoplastic left heart syndrome (HLHS) is a serious heart defect. The left side of the heart is not fully developed. To fix it, kids need a series of surgeries called the Norwood procedure.
The first surgery is done soon after birth. Later surgeries are done as the child grows.
Arterial Switch Operation
The arterial switch operation fixes a heart defect called transposition of the great arteries (TGA). In TGA, the heart’s main arteries are reversed. This surgery is a big win in pediatric heart care.
It switches the arteries and moves the coronary arteries to the new aorta.
Complex Single Ventricle Palliation
Single ventricle heart defects mean the heart only has one working ventricle. Surgery aims to improve heart function, not fix it completely. The Fontan procedure is a key part of this process.
This surgery directs blood to the lungs, skipping the heart. It’s a complex operation that needs careful planning.
Fixing congenital heart defects in kids takes a team effort. Cardiologists, surgeons, and others work together. Thanks to new surgery methods and care, kids are doing better.
Ventricular Assist Device Implantation and Artificial Hearts
Ventricular assist devices (VADs) have changed how we treat advanced heart failure. They give hope to those waiting for a heart transplant. These devices help or replace the heart’s function, part of mechanical circulatory support systems.
Types of Mechanical Circulatory Support
There are different types of mechanical circulatory support devices. These include ventricular assist devices (VADs) and total artificial hearts (TAHs). VADs can be left ventricular assist devices (LVADs), right ventricular assist devices (RVADs), or biventricular assist devices (BiVADs). Each type meets specific needs based on the patient’s condition.
The right device depends on the patient’s heart condition, how severe the heart failure is, and if they might recover or need a transplant.
Surgical Complexity and Anatomical Considerations
Putting in VADs and TAHs is a complex surgery that needs careful planning. Surgeons look at the patient’s anatomy, the device’s design, and possible complications. They make a chest incision, connect the device to the heart, and check it works before closing.
They consider the heart’s size and position, any scar tissue from past surgeries, and the patient’s overall health.
Managing Device-Related Complications
Patients with VADs and TAHs face risks like infection, bleeding, and device failure. A team of doctors, including cardiologists and surgeons, works together to manage these risks. Regular check-ups and monitoring are key to preventing problems.
To handle complications, doctors use anticoagulation therapy to stop clots, antibiotics to prevent infections, and check the device regularly to ensure it’s working right.
Redo Cardiac Surgeries: Operating Through Scar Tissue
Redo cardiac surgeries are very complex. They need careful planning and execution. Scar tissue from previous surgeries makes the surgery harder.
Technical Challenges of Reoperations
Redo cardiac surgeries face big challenges. Scar tissue increases the risk of problems. The main issues are:
- It’s hard to find the right structures because of adhesions.
- Scar tissue can cause more bleeding.
- The surgery takes longer.
Surgeons use special techniques and tools to tackle these problems. They plan carefully before surgery and use precise dissection. The right tools are also key.
Risk Stratification for Repeat Procedures
It’s important to know the risks in redo cardiac surgeries. This helps identify patients who might face more problems. Consider these factors:
- The history of previous surgeries and scar tissue.
- The patient’s overall health and any other health issues.
- The type of cardiac procedure being done again.
By looking at these, surgeons can prepare better. They can plan to reduce risks and improve outcomes.
Surgical Strategies to Minimize Complications
Surgeons use different ways to lower the risk of problems. These include:
- Trying minimally invasive techniques when it’s safe.
- Using advanced imaging for better planning.
- Using special tools made for redo surgeries.
These methods help make redo cardiac surgeries less complex and risky. They improve the chances of a good outcome for patients.
The Role of Cardiopulmonary Bypass in Complex Cases
Cardiopulmonary bypass is key in complex heart surgeries. It lets surgeons work on a heart that’s not beating. This tech has changed cardiac surgery, making complex operations possible.
This technology, also known as a heart-lung machine, takes over heart and lung functions during surgery. It gives surgeons a bloodless, motionless area to work. This is vital in complex surgeries where precision is essential.
Deep Hypothermic Circulatory Arrest
Cardiopulmonary bypass is vital in deep hypothermic circulatory arrest (DHCA). DHCA cools the body, stops the heart, and stops blood flow. It’s used in surgeries needing a bloodless field, like aortic arch surgery.
DHCA lowers the body’s metabolic rate, reducing oxygen demand and protecting organs. But, it also risks neurological injuries from prolonged hypothermia and arrest.
Neurological Complications and Prevention
Neurological issues are a big worry in surgeries with cardiopulmonary bypass, like DHCA. Risks include stroke and cognitive problems. To lower these risks, doctors manage blood pressure, temperature, and use neuroprotective agents.
Tools like EEG and NIRS monitor brain function and oxygenation during surgery. These help doctors and anesthesiologists make safer choices.
Advancements in Perfusion Technology
New developments in perfusion tech have made cardiopulmonary bypass safer and more effective. Modern machines have advanced controls for blood flow, temperature, and oxygen. Miniaturized systems have also made things simpler and safer.
Future improvements will likely include even smaller machines, better biocompatibility, and real-time monitoring. These advancements will keep improving outcomes for patients in complex surgeries.
Mortality Rates and Outcomes of High-Risk Cardiac Surgeries
It’s important to know the mortality rates of high-risk cardiac surgeries to improve patient care. These surgeries are complex and can have different outcomes. They are often done on patients with many health issues or advanced heart disease.
We will look at the statistics of these surgeries’ mortality rates. We will also examine quality metrics and what predicts poor outcomes. This will help us understand this critical topic better.
Statistical Analysis of Procedure-Specific Mortality
Statistical analysis helps us understand the death rates of different heart surgeries. By looking at data from registries and clinical trials, we can spot trends. This information helps doctors and patients make better choices.
For example, surgeries like heart transplants or complex valve repairs have their own risk levels. These risks depend on the patient, the surgery, and aftercare. We use statistics to adjust for these factors and give a clearer picture of the risks.
| Procedure | 30-Day Mortality Rate (%) | 1-Year Survival Rate (%) |
| CABG | 2.5 | 90 |
| Heart Transplant | 5 | 85 |
| Complex Valve Repair | 3.2 | 88 |
Quality Metrics in Cardiac Surgery
Quality metrics are key in cardiac surgery to measure performance and improve quality. These metrics include death rates, complication rates, and patient satisfaction.
By tracking these metrics, we can find areas to improve. For example, following guidelines and joining national registries can lower death rates and improve care quality.
Predictors of Poor Outcomes
Finding what predicts poor outcomes is vital for managing risk and patient care. Age, health conditions, and surgery complexity all play a role. Biomarkers and preoperative tests also help assess risk.
Understanding these predictors helps us counsel patients and their families better. It also helps us tailor treatments to improve outcomes. Every patient is different, so a personalized approach is key in managing high-risk surgeries.
We aim to achieve the best outcomes for our patients through a mix of clinical expertise, evidence-based practices, and continuous quality improvement.
The Making of a Cardiothoracic Surgeon
Becoming a cardiothoracic surgeon is a long journey. It needs dedication, skill, and a deep understanding of the heart. These surgeons treat heart diseases with complex surgeries. They must be very precise and skilled.
Training Pathway and Expertise Development
The path starts with a strong medicine education. Then, there’s specialized training in cardiothoracic surgery. This training takes years, with hands-on experience under experts.
To stay skilled, cardiothoracic surgeons must keep up with new techniques. They do this through continuous education, workshops, and conferences.
Physical and Mental Demands of Complex Cases
Cardiothoracic surgery is physically tough. Surgeons work long hours in stressful environments. They need to be in great shape.
The mental challenges are just as big. They must make quick, accurate decisions under stress. Cases range from simple to very complex, like heart transplants.
Decision-Making Under Extreme Pressure
Decision-making is key for cardiothoracic surgeons. They quickly assess situations, weigh risks, and make decisions that affect patients’ lives.
Staying calm and focused is vital. Surgeons work in teams, needing good communication and leadership. This ensures the best care for patients.
Here’s a look at the typical training for cardiothoracic surgeons:
| Stage | Description | Duration |
| Medical School | Basic medical education | 4 years |
| Residency | Hands-on training in surgery | 5-7 years |
| Fellowship | Specialized training in cardiothoracic surgery | 2-3 years |
Recovery Challenges After Major Cardiac Surgery
The journey to recovery after major cardiac surgery is complex and multifaceted. Patients often face a range of challenges that can impact their overall outcome and quality of life.
Intensive Care Management
Immediately after surgery, patients are closely monitored in the intensive care unit (ICU). ICU care is critical for managing possible complications and ensuring a stable transition to the recovery phase.
Effective intensive care management involves a team of experts. They closely watch the patient’s vital signs, manage pain, and address any immediate post-surgical complications.
Long-Term Rehabilitation Protocols
As patients move beyond the ICU, they start a phase of long-term rehabilitation. This includes physical therapy, dietary counseling, and lifestyle adjustments to support cardiac health.
Rehabilitation protocols are tailored to the individual patient’s needs. They may include exercises to improve cardiovascular endurance, strength training, and flexibility exercises.
Quality of Life Considerations
Improving or maintaining the patient’s quality of life is a primary goal of recovery. This involves not just physical recovery but also addressing psychological and emotional needs.
Healthcare providers work with patients to develop strategies for managing stress, improving mental health, and reintegrating into daily activities and social roles.
Technological Frontiers in Complex Cardiac Surgery
The field of complex cardiac surgery is changing fast thanks to new technologies. These innovations are making surgeries better and improving patient care. As we explore new possibilities, several technologies stand out as key.
3D Printing and Surgical Planning
3D printing is a big deal in cardiac surgery. It lets surgeons make exact models of a patient’s heart. This helps them plan surgeries better.
These models are super helpful for complex heart issues or valve repairs. They let surgeons see the heart’s details clearly. This makes planning more precise.
3D printing also helps make custom surgical tools and implants. These fit perfectly in the patient’s body. This can make surgeries shorter and more successful.
Artificial Intelligence Applications
Artificial intelligence (AI) is also changing cardiac surgery. AI looks at lots of data to help diagnose heart problems better. It also predicts how well a patient will do after surgery.
AI tools also make imaging better. They spot small issues that might be missed. This leads to better treatment plans.
Hybrid Operating Rooms and Image Guidance
Hybrid operating rooms are a big step forward. They mix traditional surgery with advanced imaging like MRI. This lets surgeons see what they’re doing in real time.
This is great for less invasive surgeries. It helps surgeons avoid mistakes and improve results. It’s safer for patients too.
As we keep using these new technologies, cardiac surgery’s future looks bright. With 3D printing, AI, and hybrid rooms, we’re getting closer to better patient care.
Conclusion
Cardiac surgery covers many complex procedures. Each one has its own challenges and details. The field keeps growing thanks to new technology and techniques.
Surgeries like coronary artery bypass grafting need a lot of skill. Heart valve replacement is also very precise. Heart transplantation is the top of cardiothoracic surgery. It requires skill, careful donor selection, and post-transplant care.
The future of cardiac surgery looks bright. New tools like 3D printing, artificial intelligence, and hybrid operating rooms are coming. These will help improve patient care and treat more heart conditions.
Cardiac surgery’s complexity shows we must keep improving. We need better surgical techniques and patient care. This will help patients get the best results from these life-saving surgeries.
FAQ
What is the most challenging type of cardiac surgery?
Heart transplantation is often seen as the most complex. It involves choosing a donor, preserving the organ, and managing after the transplant.
What are the risks associated with open heart surgery?
Open heart surgery can lead to bleeding, infection, and brain problems. It’s important to weigh these risks to decide the best treatment.
How does CABG differ from other cardiac surgeries?
CABG is a surgery that bypasses blocked arteries. It’s different from surgeries like replacing or fixing heart valves.
What is the difference between off-pump and on-pump CABG?
Off-pump CABG doesn’t use a heart-lung machine. On-pump CABG does, making it easier to operate.
What are the challenges of redo cardiac surgeries?
Redo surgeries face tough conditions. Scar tissue, adhesions, and changed heart shape make it hard for surgeons to work.
How do ventricular assist devices work?
Ventricular assist devices are pumps that help the heart in severe failure. They improve heart function and reduce symptoms.
What is the role of cardiopulmonary bypass in cardiac surgery?
Cardiopulmonary bypass is key in many surgeries. It lets surgeons work on a stopped heart by taking over heart and lung functions.
How do surgeons prepare for complex cardiac surgeries?
Surgeons get a lot of training and must master complex techniques. They also learn to assess patients and manage risks.
What are the latest technological advancements in cardiac surgery?
New tech includes 3D printing, artificial intelligence, and hybrid rooms. These improve planning, precision, and results.
What is the recovery process like after major cardiac surgery?
Recovery involves intensive care and long-term rehab. It also focuses on improving quality of life for patients.
How do surgeons manage complications during cardiac surgery?
Surgeons use their skills and new tech to handle complications. This helps reduce risks and improve outcomes.
What are the key factors that determine the difficulty of cardiac surgery?
Surgery complexity depends on patient health, comorbidities, technique, and risks. Surgeons must assess these carefully to choose the best treatment.
References
- Senst, B. (2022). Cardiac surgery. In StatPearls. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK532935/