Last Updated on October 31, 2025 by
We are seeing big changes in treating prostate cancer and BPH with new minimally invasive prostate surgeries like TULSA and MRgFUS. These new methods are making a big difference. They help patients recover faster, have fewer side effects, and maintain their urinary and sexual functions. Learn about the new, amazing way to operate prostate issues. Discover the latest minimally invasive surgery that is revolutionizing patient care.
Studies are showing great results. Over 90% of patients have controlled disease after a year. Also, only 5% of patients have urinary incontinence issues at 30 days, and less than 1% at 6 months. This is a big step forward in treating prostate issues, giving patients safer and more effective options.
Prostate health is key to men’s health. As men get older, their prostate gland can change, leading to health issues. We’ll look at common prostate conditions that might need surgery, including symptoms, diagnosis, and treatment.
BPH is common in men over 50. It’s when the prostate gland gets bigger. This can cause urgency, frequency, and a weak urinary stream. If these symptoms are bad and meds don’t help, surgery might be needed.
To diagnose BPH, doctors look at medical history, physical exams, and tests like an ultrasound or cystoscopy. Knowing how bad BPH is helps decide the best treatment.
Prostate cancer is another serious issue that might need surgery. The choice to operate depends on the stage and aggressiveness of the cancer. Surgery tries to remove the cancerous tissue while keeping as much normal tissue as possible.
Finding prostate cancer early is very important. Treatment choices depend on the cancer’s stage and the patient’s health. Surgery is often chosen for early-stage prostate cancer.
Prostate surgery has changed a lot. It moved from old open surgeries to new, less invasive methods. These changes aim to make treatments safer, more effective, and with less pain and quicker healing.
Older surgeries for prostate issues like Benign Prostatic Hyperplasia (BPH) and cancer were open prostatectomies. They involved big cuts to reach the prostate. But they caused a lot of postoperative pain, longer hospital stays, and more risks.
Transurethral Resection of the Prostate (TURP) was a big step forward. It removes prostate tissue through the urethra, avoiding big cuts. It’s used for BPH and has less pain and quicker healing than old surgeries. For more info, check out PubMed Central.
New tech has led to even less invasive surgeries like Holmium Laser Enucleation of the Prostate (HoLEP). HoLEP uses a laser to remove tissue, cutting down on bleeding and shortening recovery. These new methods are a big leap forward, making treatments safer and faster.
As we keep improving prostate surgery, we focus on making it less painful and quicker to heal. Moving to less invasive methods shows how far medical science has come. It brings hope and better results for patients everywhere.
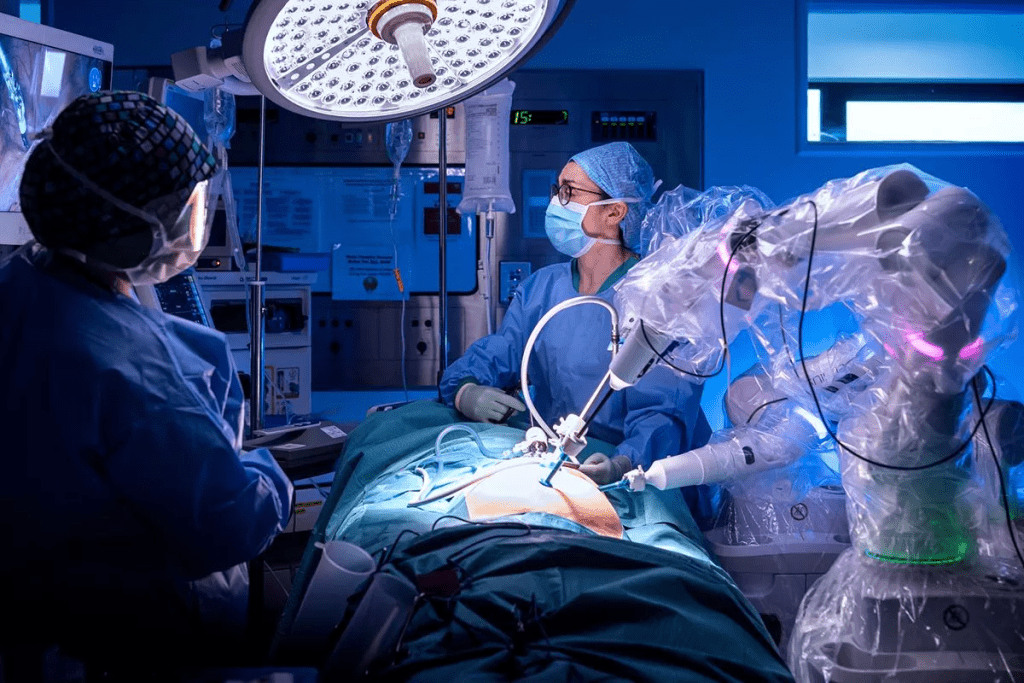
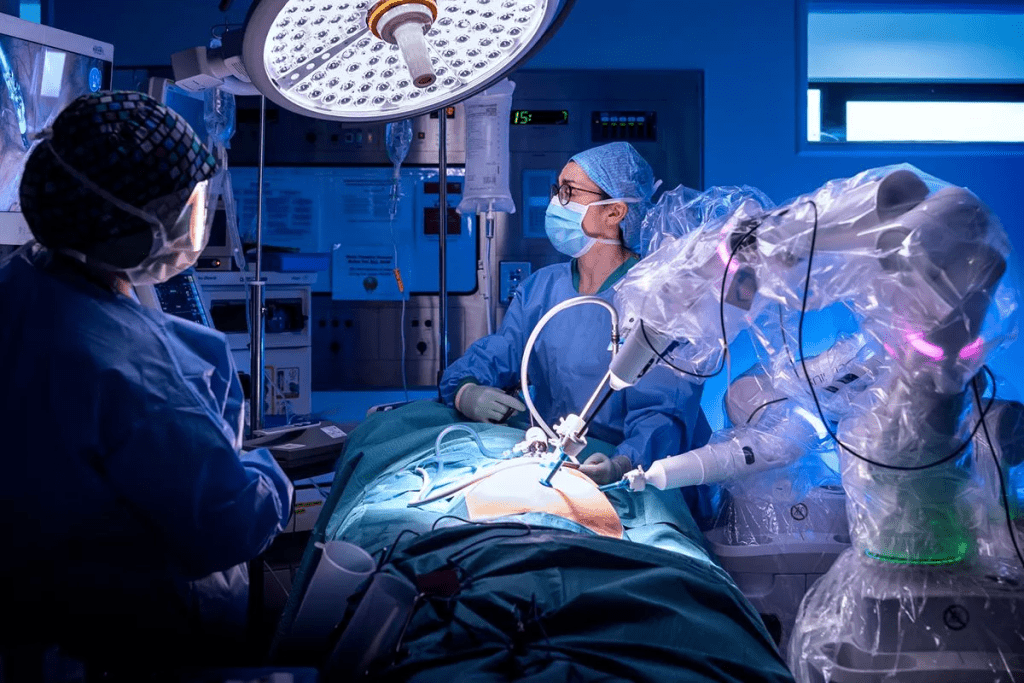
Prostate surgery has seen big changes. Now, doctors can operate more accurately and with less harm to nearby tissues. This shift towards precise and less invasive methods is making recovery times shorter and outcomes better.
Image-guided precision is changing prostate surgery. It lets surgeons see the prostate and nearby areas live during surgery. This makes it easier to remove or treat the right part, cutting down on risks.
Advanced imaging, like MRI and ultrasound, is used more often now. They give a clear view of the prostate. This helps surgeons:
Tissue-preserving technologies are also big steps forward. They aim to cause less damage to nearby tissues. This lowers the chance of problems and speeds up healing.
Some key technologies include:
Many prostate surgeries can now be done without staying in the hospital. This is good for patients because it means less time in the hospital and quicker recovery.
Outpatient surgery is possible because of:
By using these new advances, we can give our patients the best results. We aim to reduce complications and help them get back to their lives faster.
TULSA, MRgFUS, and HoLEP are leading the way in prostate surgery. They offer new options beyond traditional surgery. These methods help with BPH and prostate cancer, leading to better results and quicker recovery.
TULSA uses ultrasound to remove prostate tissue. This method is great for treating localized prostate cancer. It targets cancer cells well while keeping healthy tissue safe. TULSA is effective with few side effects, making it a good choice for many patients.
A top urologist says,
“TULSA is a big step forward in prostate cancer treatment. It’s a highly effective and less invasive option for patients with localized disease.”
MRgFUS uses ultrasound waves to treat prostate cancer. It’s guided by MRI imaging, allowing for precise treatment. This method is effective for localized prostate cancer and is non-invasive.
HoLEP treats BPH with a holmium laser. It improves urine flow and lowers risks from traditional TURP. HoLEP is great for larger prostates, making it efficient for removing blockages.
These new techniques offer faster recovery, less pain, and fewer complications than traditional surgery. As technology improves, we’ll see even more progress in treating prostate issues.
Minimally invasive prostate surgeries have changed how we treat prostate issues. They offer different options for each patient’s needs. Knowing the differences between these surgeries is key when deciding on treatment for an enlarged prostate or prostate cancer.
The right surgery depends on the condition. For Benign Prostatic Hyperplasia (BPH), Holmium Laser Enucleation of the Prostate (HoLEP) is often chosen. It’s great for bigger prostates because it removes tissue that blocks urine flow.
For prostate cancer, TULSA (Transurethral Ultrasound Ablation) and MRgFUS (MRI-guided Focused Ultrasound Surgery) are better. They precisely kill cancer cells.
For BPH, the prostate’s size is important. HoLEP is best for larger prostates. It removes tissue without the need for big surgeries.
Several things decide if a surgery is right for a patient. These include the prostate’s size, how bad the symptoms are, and the patient’s health. For example, HoLEP is good for those with bad urinary problems. It removes tissue that blocks urine flow.
When talking to a urologist, ask important questions. This helps make a good choice. Some key questions are:
Understanding each surgery and talking to a doctor helps patients choose wisely. This ensures they get the best treatment for their needs.
Minimally invasive prostate surgery has changed how we treat prostate issues. It offers better results, shorter recovery times, and a better quality of life. We’ve looked at the newest advancements in prostate surgery.
Techniques like TULSA, MRgFUS, and HoLEP are now top choices for BPH and prostate cancer. These new methods let us tailor care to each patient. Getting help from a skilled urologist means patients can enjoy these modern treatments.
We’re always looking to improve medical care, with a focus on top-notch healthcare for everyone. Minimally invasive surgery is making a big difference in prostate care. We’re here to help patients understand and use these new options.
HoLEP is a minimally invasive surgery. It uses a holmium laser to remove prostate tissue blocking urine flow. This treats Benign Prostatic Hyperplasia (BPH) by removing the prostate tissue.
HoLEP has many benefits. It reduces the risk of urinary incontinence and erectile dysfunction. It also causes less bleeding and has shorter hospital stays. It’s good for larger prostates and for those at risk from traditional surgery.
HoLEP mainly treats BPH, not prostate cancer. But it might be used with other treatments like radiation for urinary symptoms.
HoLEP recovery is quicker than traditional surgery. Most patients can get back to normal in a few weeks. They see big improvements in urine symptoms in a few months.
Each procedure has its own benefits. HoLEP works well for larger prostates and severe BPH. TULSA and MRgFUS use different technologies. We’ll help choose the best for you.
Like any surgery, HoLEP has risks like bleeding and infection. But these are rare. We’ll talk about these risks and benefits with you.
See a qualified urologist for a check-up. They’ll look at your health, prostate size, and symptoms. They’ll suggest the best treatment for you.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!