Last Updated on November 26, 2025 by Bilal Hasdemir

A quick operation after a heart attack can greatly increase the chances of survival. Emergency steps like primary percutaneous coronary intervention (PCI) are key for treating ST-segment elevation myocardial infarction (STEMI).
Coronary artery bypass surgery is also a vital heart attack treatment option. It makes a new path for blood to the heart. This is done by using a healthy blood vessel from another part of the body to bypass a blocked artery.
Getting treatment quickly is very important for heart attack patients. There are many treatment options available. Knowing about these can help patients make better choices about their care.
Key Takeaways
- Timely operation after a heart attack improves survival rates.
- Primary percutaneous coronary intervention (PCI) is a standard treatment for STEMI.
- Coronary artery bypass surgery creates a new path for blood flow to the heart.
- Understanding treatment options is key to making informed decisions.
- Prompt treatment greatly improves outcomes for heart attack patients.
Understanding Heart Attacks and Their Immediate Impact

Heart attacks can affect the heart in different ways, depending on the type. This makes quick and proper treatment very important. Heart attacks are mainly of two types: STEMI (ST-Elevation Myocardial Infarction) and NSTEMI (Non-ST-Elevation Myocardial Infarction).
STEMI vs. NSTEMI: Different Types Require Different Approaches
STEMI heart attacks happen when a coronary artery is fully blocked. This causes a lot of damage to the heart muscle because it doesn’t get enough blood. On the other hand, NSTEMI heart attacks have a partial blockage. This results in less damage but also needs quick medical help.
Knowing the differences between these two types is key. It helps decide the best treatment for STEMI or NSTEMI.
The Critical Time Window After a Heart Attack
Time is very important when treating heart attacks. For STEMI patients, thrombolysis should start within 30 minutes of hospital arrival. If this isn’t possible, other treatments like coronary angioplasty and stenting or CABG (Coronary Artery Bypass Grafting) might be needed. Quick action greatly affects the outcome and survival rate.
| Heart Attack Type | Characteristics | Immediate Treatment Options |
| STEMI | Complete blockage of a coronary artery | Thrombolysis, Primary PCI |
| NSTEMI | Partial blockage of a coronary artery | Medical management, PCI, CABG |
The table above shows the main differences between STEMI and NSTEMI. It also lists the immediate treatments for each type. Quick and correct treatment is vital for both types to reduce damage and improve patient results.
The Golden Hour: Why Timing Is Critical for Heart Attack Treatment
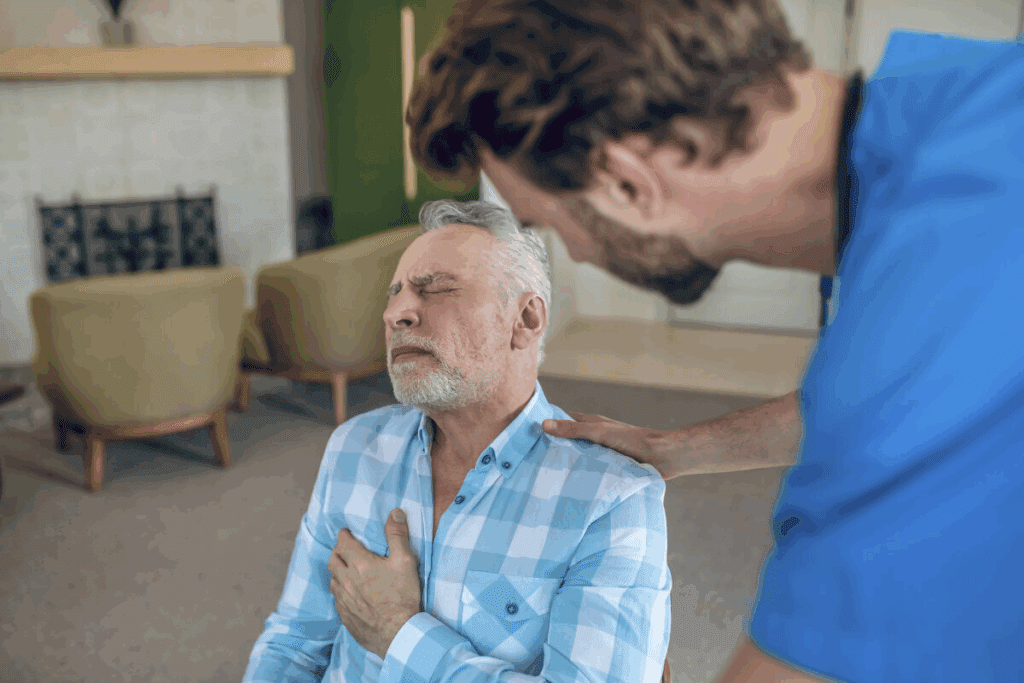
Getting medical help quickly is key for heart attack victims. It greatly affects their chances of survival. The first hour after a heart attack is called the “golden hour,” showing how urgent treatment is.
The “golden hour” idea comes from knowing that the first hour is most important. Primary Percutaneous Coronary Intervention (PCI) works best then. It’s a main treatment for STEMI (ST-Elevation Myocardial Infarction).
The 90-Minute Window for Optimal Outcomes
For STEMI patients, Primary PCI should start within 90 minutes of symptoms. This door-to-balloon time is key. It causes heart damage.
Shorter times mean lower death rates and better results. Hospitals and EMS work hard to cut down delays. They aim for quick treatment.
How Fast Treatment Impacts Survival Rates
Treatment speed after a heart attack affects survival. Rapid restoration of blood flow saves lives. It also lowers complication risks and improves long-term health.
Every minute delay in STEMI treatment raises mortality risk. So, quick treatment is not just a rule. It’s vital for patient outcomes. By focusing on the “golden hour” and the 90-minute goal, healthcare can boost survival and recovery chances.
Primary Percutaneous Coronary Intervention (PCI): The Gold Standard
Primary Percutaneous Coronary Intervention (PCI) is now the top choice for treating heart attacks, mainly STEMI. It’s key in getting blood back to the heart muscle, cutting down damage risk.
What Happens During a Primary PCI Procedure
A catheter is put through an artery in the groin or wrist during Primary PCI. It’s guided to the blocked artery. Then, a balloon angioplasty opens the artery, and a stent keeps it open.
Primary PCI greatly helps STEMI patients by quickly restoring blood flow to the heart. It’s done in a cardiac lab by skilled cardiologists and technicians.
Stent Placement and Its Benefits
Stent placement is a key part of Primary PCI. The stent, a small, mesh-like tube, is placed at the blockage. It keeps the artery open, improving blood flow to the heart muscle.
Stents help by lowering artery re-narrowing and improving long-term results. Modern stents release medication to prevent re-narrowing.
Recovery Timeline After PCI
Recovery from Primary PCI is quick, with most patients watched for hours after. Many can go back to normal activities in a few days. But they should avoid hard exercise and heavy lifting for a bit.
A comprehensive recovery plan includes doctor visits, lifestyle changes, and taking meds as directed. This helps manage risks and prevent future heart issues.
Thrombolytic Therapy: Alternative Treatment When PCI Isn’t Available
When primary PCI is not available, thrombolytic therapy is a key alternative for STEMI patients. It involves using medications to break down clots and improve blood flow to the heart. This helps reduce further damage.
Mechanism of Clot-Busting Medications
Clot-busting medications, or thrombolytic agents, activate the body’s fibrinolytic system. This dissolves the clot and restores blood flow to the heart. Tissue plasminogen activator (tPA) is a common agent used for STEMI treatment.
Risks and Benefits of Thrombolytic Agents
Thrombolytic therapy has both good and bad sides. It can greatly reduce death and illness in STEMI patients if given quickly. But it also carries a risk of bleeding, including a brain hemorrhage. It’s important to carefully choose patients and monitor them closely to lessen these risks.
- Benefits: Effective in reducing mortality in STEMI patients
- Can be given quickly in emergency settings
- Provides an alternative when primary PCI is not available
- Risks: Bleeding complications, including intracranial hemorrhage
- Not recommended for certain patients (e.g., recent stroke, major surgery)
When Thrombolytics Are the Preferred Option
Thrombolytic therapy is preferred when primary PCI can’t be done within 90 minutes. It’s also used for patients in remote areas or those who can’t reach a PCI-capable center in time.
“Thrombolytic therapy remains a vital component of STEMI management, particularly in scenarios where timely access to primary PCI is not feasible.”
— American Heart Association
In conclusion, thrombolytic therapy is a vital option for STEMI patients when primary PCI is not available. Healthcare providers need to understand its benefits and risks. This knowledge helps make informed decisions and provide the best care.
STEMI Intervention: Specialized Treatment Protocols
STEMI treatment focuses on quickly getting blood to the heart again. This is key to reducing heart damage and helping patients recover better.
Emergency Response and Initial Assessment
When a STEMI patient arrives at the hospital, they get checked right away. This includes an electrocardiogram (ECG) and tests for heart enzymes. Rapid diagnosis is key to starting the right treatment.
- ECG to confirm ST-elevation
- Biomarker testing for cardiac enzymes
- Initial assessment of the patient’s medical history
Immediate Interventions to Restore Blood Flow
The main goal is to open the blocked artery. This is done through Primary Percutaneous Coronary Intervention (PCI). PCI is the best treatment for STEMI when it’s available.
- Activation of the cath lab team
- Administration of anticoagulant and antiplatelet therapy
- Performance of Primary PCI
Post-Procedure Monitoring and Care
After the procedure, patients are watched closely in a special unit. Post-procedure care includes:
- Continuous ECG monitoring
- Assessment of renal function and possible kidney damage from the procedure
- Management of antiplatelet and anticoagulant therapy
Effective STEMI treatment needs a team effort. Cardiologists, emergency doctors, and others work together. By sticking to these protocols, doctors can greatly improve STEMI patient outcomes.
NSTEMI and Mild Heart Attack Treatment Approaches
Treating NSTEMI and mild heart attacks needs a careful plan. It mixes medical care with special procedures. The right choice depends on the patient’s health, how bad the heart attack is, and other risk factors.
Medical Management vs. Interventional Procedures
First, doctors often use medical management for NSTEMI and mild heart attacks. This helps keep the patient stable and stops further heart damage. They use medicines to stop clots, reduce heart work, and improve blood flow.
For those at higher risk or not helped by medicine, doctors might choose interventional procedures. This includes putting a stent in the artery to keep it open. This helps blood flow back to the heart muscle.
Key Considerations for Treatment Selection:
- Patient’s overall health status
- Severity of the heart attack
- Presence of comorbid conditions
- Risk of bleeding or other complications
Risk Stratification and Treatment Selection
Knowing the patient’s risk is key in choosing treatment. Tools like the GRACE score help doctors decide between medicine and procedures. This helps avoid bad outcomes.
| Risk Factor | Low Risk | High Risk |
| Age | < 60 years | ≥ 60 years |
| Troponin Levels | Normal or slightly elevated | Significantly elevated |
| Electrocardiogram (ECG) Changes | Minimal or no changes | Significant ST-segment changes |
Monitoring and Follow-Up Care Protocols
After treatment, patients need close monitoring and follow-up. This helps prevent problems and improves long-term health. They see a cardiologist regularly, have their heart checked, and adjust medicines as needed.
“The key to successful management of NSTEMI and mild heart attacks lies in a complete treatment plan that fits the patient’s needs and risk.” –
A cardiologist’s perspective
Good treatment also means making lifestyle changes. This includes eating better, being more active, and quitting smoking. These steps help lower the chance of more heart problems.
Medication Management Following a Heart Attack
Survivors of heart attacks must follow a strict medication plan to avoid future heart problems. This plan is key to recovery, preventing more heart damage and lowering the chance of complications.
Blood Thinners and Antiplatelet Therapy
Blood thinners and antiplatelet drugs are vital to stop new clots and lower heart attack risk. Antiplatelet therapy, like aspirin or clopidogrel, stops platelets from clumping. This keeps blood flowing in the heart’s arteries, cutting down on cardiac events.
Doctors often mix blood thinners with antiplatelet drugs for heart attack patients. Aspirin is often chosen for its ability to prevent platelets from sticking together. Other drugs, like warfarin, are used for their blood-thinning effects. The right mix depends on the patient’s health and medical history.
Beta-Blockers, ACE Inhibitors, and Statins
Other drugs are also key in managing heart health after a heart attack. Beta-blockers slow the heart rate and lower blood pressure, reducing heart strain and arrhythmia risk.
ACE inhibitors relax blood vessels, improving blood flow and lowering blood pressure. They’re good for those with heart failure or at risk of it. Statins, which lower cholesterol, prevent plaque buildup.
Managing Your Medication Regimen Long-Term
Long-term medication management needs dedication and planning. Patients must stay in close touch with their doctors to adjust their meds as needed. It’s important to know why each drug is used, its side effects, and how to take it right.
To stick to the plan, patients can use pill boxes, set reminders, or get help from family. Regular check-ups with doctors are also key to ensuring the treatment is working and to make any needed changes.
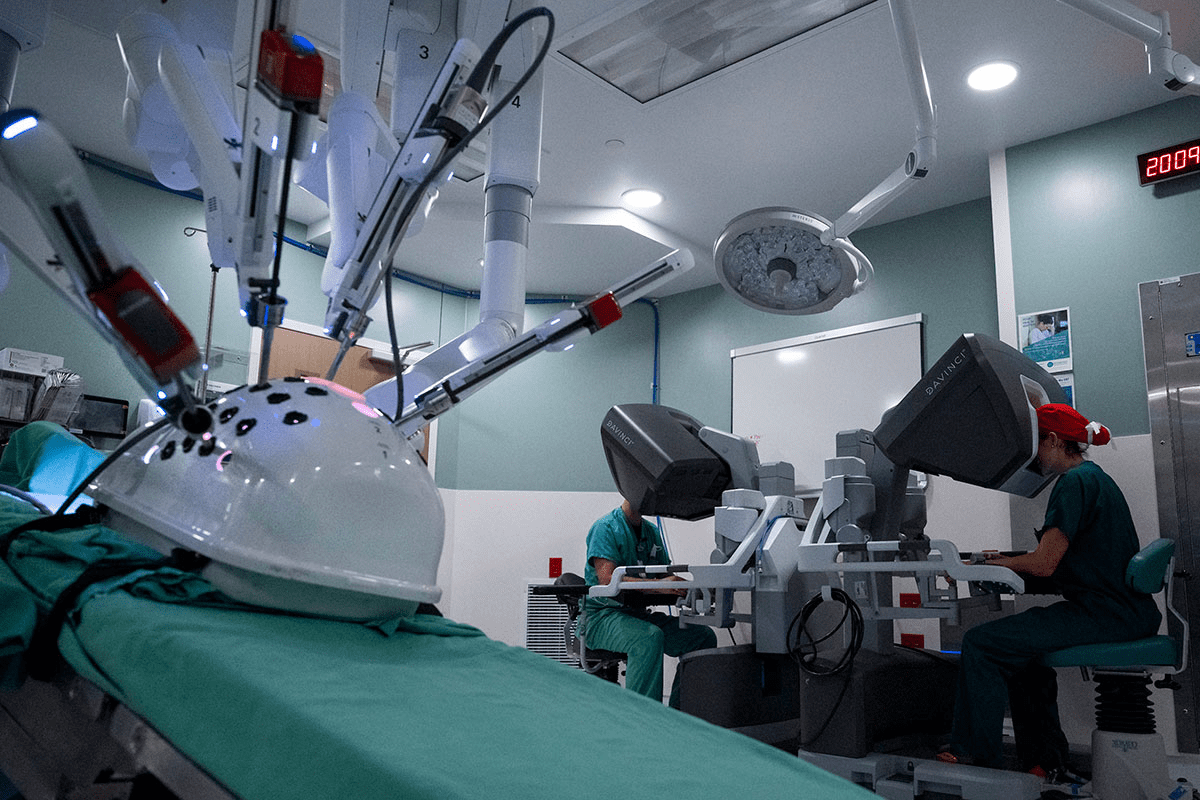
Coronary Artery Bypass Grafting (CABG): Operation After Heart Attack for Severe Cases
For those who have had a severe heart attack, CABG is a key surgery. It involves using a healthy blood vessel to bypass a blocked artery. This helps blood flow back to the heart muscle.
When CABG Is Recommended Over Other Treatments
CABG is often suggested for complex heart disease cases. It’s for those with many blockages or when other treatments like PCI don’t work.
- Patients with multiple blockages in their coronary arteries
- Those for whom PCI is not suitable
- Individuals with diabetes and multi-vessel coronary artery disease
The Surgical Procedure Explained
The CABG process includes several steps:
- The patient is given general anesthesia for comfort during surgery.
- A surgeon takes a graft from another part of the body, usually the leg or arm.
- The graft is then attached to the coronary artery, bypassing the blockage.
This surgery needs great precision and is done by skilled cardiothoracic surgeons.
Recovery and Rehabilitation After Bypass Surgery
Recovering from CABG means following a detailed rehabilitation plan. This includes:
- Monitoring in an intensive care unit right after surgery
- Slowly starting to move and doing physical therapy
- Getting advice on lifestyle changes and managing medications
Cardiac rehabilitation experts say, “A good rehabilitation program is key for the best recovery and long-term results after CABG.”
Emergency Procedures for Complications After a Heart Attack
Heart attack complications can be deadly, needing quick and effective help. It’s key to manage these issues to avoid more harm and help patients get better.
Managing Arrhythmias and Electrical Disturbances
After a heart attack, irregular heartbeats are common. Prompt treatment is essential to stop these from becoming deadly. Doctors use beta-blockers and other drugs to fix the heartbeat.
In some cases, they might need to do cardioversion or put in a pacemaker or ICD.
Mechanical Support Devices for Cardiogenic Shock
Cardiogenic shock occurs when the heart can’t pump enough blood. Mechanical support devices like IABPs and LVADs help. They’re used in the ICU to keep patients stable until they can get more treatment.
Treating Heart Failure Following Myocardial Infarction
Heart failure can happen after a heart attack if the heart gets too damaged. Doctors use drugs like ACE inhibitors and beta-blockers to help the heart work better. Changing diet and exercise habits is also key.
In severe cases, heart transplantation might be needed.
Quick and effective emergency care is vital for heart attack complications. It helps save lives and improve patients’ quality of life. Healthcare teams play a big role in making these outcomes better.
Cardiac Rehabilitation: The Path to Recovery
After a heart attack, a special program called cardiac rehabilitation helps you get better. It’s a detailed plan to help you regain your health and feel better overall.
The Three Phases of Cardiac Rehabilitation
Cardiac rehab has three main parts, each with its own goals and results.
- Phase 1: Starts in the hospital, focusing on getting moving and learning about your health.
- Phase 2: This is an outpatient program. It includes supervised workouts, advice on lifestyle, and managing risks.
- Phase 3: This is the long-term phase. Here, you keep exercising and managing your health on your own.
Exercise Protocols and Physical Therapy
Exercise is key in cardiac rehab, tailored to fit your needs. Supervised exercise programs boost heart health, build strength, and improve flexibility.
| Exercise Type | Benefits | Frequency |
| Aerobic Exercise | Improves cardiovascular health | 3-4 times a week |
| Resistance Training | Enhances muscle strength | 2-3 times a week |
| Flexibility Exercises | Increases range of motion | Daily |
Psychological Support and Lifestyle Counseling
Cardiac rehab also focuses on the mental side of recovery. It offers counseling and stress management techniques. Lifestyle counseling helps you make smart choices about diet, quitting smoking, and other health habits.
By combining these elements, cardiac rehab programs offer a complete recovery plan. They empower you to manage your health and lower the chance of future heart problems.
Advanced Treatment Options and Future Directions
The future of heart attack treatment is looking bright. New technologies and treatments are being developed. These advancements aim to improve patient care and outcomes.
Stem Cell Therapy and Regenerative Medicine
Stem cell therapy and regenerative medicine are leading the way. They aim to fix or replace damaged heart tissue. This could help reverse heart attack damage.
Regenerative medicine uses stem cells to grow new heart tissue. This could lead to better heart function and outcomes for patients.
- Stem cell therapy promotes the regeneration of heart tissue.
- Regenerative medicine offers a possible cure for heart damage.
- These treatments are being tested in clinical trials.
Innovative Devices and Technological Advances
New devices and technologies are also key in treating heart attacks. Tools like bioresorbable stents and advanced imaging are making treatments more accurate and effective.
- Bioresorbable stents dissolve over time, reducing long-term risks.
- Advanced imaging gives detailed views of the heart, helping with precise treatments.
- These technological advances are improving patient care and outcomes.
Multidisciplinary Approach at Specialized Centers Like Liv Hospital
Centers like Liv Hospital are using a team approach for heart attack treatment. A group of healthcare professionals works together to provide personalized care for each patient.
| Benefits | Description |
| Comprehensive Care | A team of specialists works together to provide holistic care. |
| Personalized Treatment | Treatments are tailored to the specific needs of each patient. |
By combining advanced treatments with a team approach, centers like Liv Hospital are improving patient outcomes. They offer new hope for those affected by heart attacks.
Conclusion: Life After Heart Attack Treatment
Effective treatment and rehabilitation can greatly improve life after a heart attack. Many patients can live active and fulfilling lives with the right care. Interventions like Primary PCI and thrombolytic therapy are key in restoring blood flow.
Cardiac rehabilitation programs help patients regain strength and manage stress. They also encourage healthier lifestyles. Long-term management is essential, including medication, lifestyle changes, and regular check-ups.
By understanding treatment options and actively participating in recovery, patients can reduce future heart risks. Medical advancements and evolving treatment methods offer new hope for recovery. This means a better outlook for life after a heart attack.
FAQ
What is the most effective treatment for STEMI?
The best treatment for STEMI is primary percutaneous coronary intervention (PCI). It quickly opens the blocked artery, restoring blood flow to the heart.
How does the type of heart attack influence treatment?
The type of heart attack matters. STEMI needs immediate treatment to open the artery. NSTEMI might get medical management first.
What is the “golden hour” in heart attack treatment?
The “golden hour” is a critical time after a heart attack. Quick treatment during this time greatly improves survival and outcomes.
What is thrombolytic therapy used for?
Thrombolytic therapy is used when PCI is not available. It dissolves clots to restore blood flow, helping STEMI patients.
How does primary PCI work?
Primary PCI uses a catheter to open blocked arteries. It often includes a stent to keep the artery open.
What medications are typically prescribed after a heart attack?
After a heart attack, patients often get blood thinners, antiplatelet therapy, and statins. Beta-blockers and ACE inhibitors are also common.
What is cardiac rehabilitation, and why is it important?
Cardiac rehabilitation includes exercise and physical therapy. It also offers psychological support. It helps in recovery and improves long-term health.
When is CABG recommended?
CABG is recommended for severe cases. It involves surgery to bypass blocked arteries when other treatments fail.
How are complications after a heart attack managed?
Complications like arrhythmias and heart failure are managed with emergency procedures. Medication and mechanical support devices are used.
What are the benefits of timely treatment for heart attack patients?
Timely treatment greatly improves survival rates. It reduces heart damage and improves prognosis for heart attack patients.
What is the role of stent placement in primary PCI?
Stent placement in primary PCI keeps the artery open. It improves blood flow and reduces the risk of further blockages.
How does the 90-minute window impact STEMI treatment?
The 90-minute window is critical for STEMI patients. Quick intervention within this time greatly improves outcomes and survival rates.
What are the treatment approaches for NSTEMI and mild heart attacks?
NSTEMI and mild heart attacks may get medical management or interventional procedures. Treatment depends on the patient’s risk and needs.
References
- Akhtar, H., Iqbal, J., Malik, M. A., et al. (2023). Experience and outcomes of primary percutaneous coronary intervention in a tertiary care hospital in South Punjab, Pakistan. Journal of the Pakistan Medical Association, (soon to be published). Retrieved from https://pubmed.ncbi.nlm.nih.gov/38186432/