Last Updated on December 2, 2025 by Bilal Hasdemir
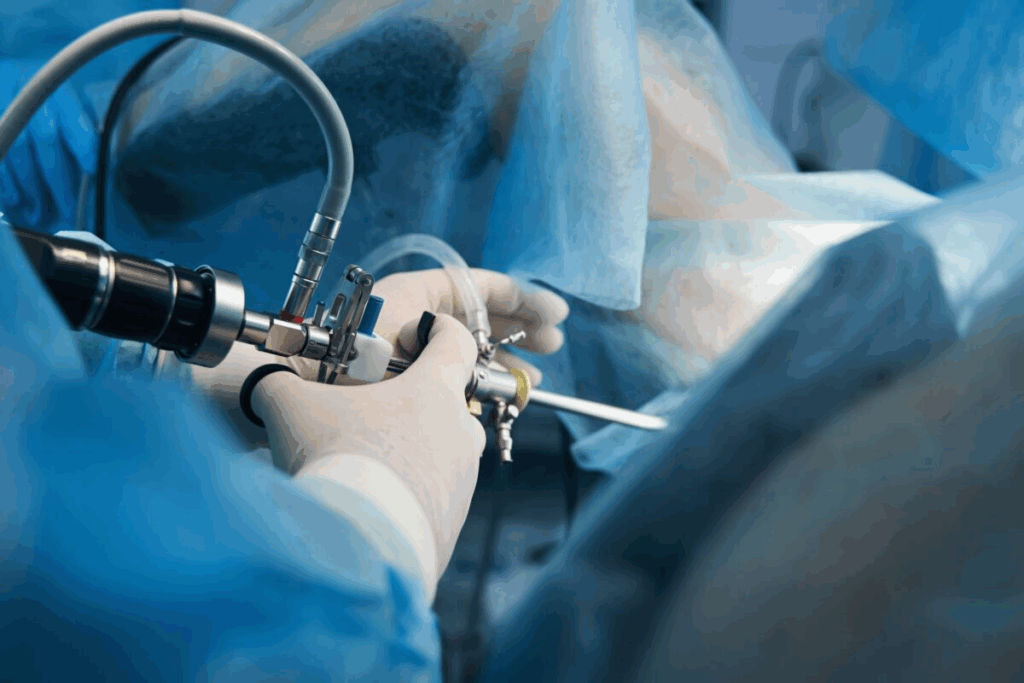
Laparoscopic surgery has changed the medical world a lot. It cuts down recovery time and reduces body trauma. Medical Expert, a top laparoscopic and fertility surgeon, says new laparoscopic techniques allow for complex surgeries with little muscle damage.
So, do muscles get cut in laparoscopic surgery? The answer depends on knowing how the surgery works and its effects on the body. This article will dive into the details of laparoscopic surgery and its effects.
Key Takeaways
- Laparoscopic surgery is designed to minimize trauma to the body.
- Advancements in laparoscopic techniques have reduced muscle damage.
- The procedure involves making small incisions to insert surgical instruments.
- Understanding the impact on abdominal muscles is key.
- Laparoscopic surgery offers a quicker recovery time compared to traditional surgery.
Understanding Laparoscopic Surgery
Laparoscopic surgery is a big step forward in surgery. It offers many benefits over old methods. It cuts down on recovery time and scarring.
Definition and Basic Principles
Laparoscopic surgery, or minimally invasive surgery, uses small cuts. These cuts let in tools and a camera for the surgery. It’s all about less damage and faster healing.
The muscle-sparing technique is key in laparoscopic surgery. It tries to avoid big muscle cuts. This means less pain and quicker healing.
Aspect | Laparoscopic Surgery | Traditional Open Surgery |
Incision Size | Small (typically 0.5-1.5 cm) | Large (often 10-30 cm) |
Recovery Time | Generally shorter | Generally longer |
Scarring | Minimal | More pronounced |
History and Development
Laparoscopic surgery started in the early 20th century. But it really took off in the 1980s. The first laparoscopic gallbladder removal was in 1987. This was a big step forward.
Comparison with Traditional Open Surgery
Laparoscopic surgery is different from old surgery methods. It causes less damage, less pain, and faster healing.
- Reduced risk of complications
- Shorter hospital stays
- Faster return to normal activities
But, it needs special training and tools. Not all surgeries can be done this way.
Anatomy of the Abdominal Wall
Knowing the anatomy of the abdominal wall is key for surgeons doing laparoscopic procedures. It’s a complex structure with many layers. These layers, including muscles and fascial planes, are vital for the success of laparoscopic surgery.
Layers of the Abdominal Wall
The abdominal wall has several layers:
- The skin, the outermost layer.
- The subcutaneous tissue, with fat and connective tissue.
- The fascia, a fibrous tissue layer around the muscles.
- The muscle layer, with several muscles.
- The peritoneum, the innermost layer lining the abdominal cavity.
Each layer must be carefully navigated during laparoscopic surgery to avoid complications.
Major Muscle Groups Involved
The abdominal wall has several major muscle groups:
- Rectus Abdominis: A long, flat muscle from the pubic crest to the xiphoid process.
- External Obliques: Muscles on either side of the rectus abdominis, involved in rotating and bending the torso.
- Internal Obliques: Muscles beneath the external obliques, also involved in torso rotation and bending.
- Transversus Abdominis: The deepest muscle layer, wrapping around the spine and pelvis.
These muscles work together to support and stabilize the abdominal cavity.
Fascial Planes and Their Importance
Fascial planes are layers of fibrous tissue that separate the muscle groups and other structures within the abdominal wall. Understanding these planes is key for:
- Navigating the abdominal wall during laparoscopic entry.
- Minimizing tissue trauma and bleeding.
- Reducing the risk of complications.
The fascial planes are vital in laparoscopic surgery. They provide a roadmap for surgeons to access the abdominal cavity safely.
Laparoscopic Entry Techniques
Surgeons use different laparoscopic entry techniques. Each has its own benefits and risks. The technique chosen can greatly affect the surgery’s success and the patient’s recovery.
Veress Needle Technique
The Veress needle technique is a common way to inflate the abdominal cavity with gas. This makes the space clearer for surgery. It involves inserting a Veress needle through the abdominal wall.
Advantages: This technique is quick and can be less invasive than others.
Potential Risks: There’s a chance of harming organs or major vessels if done wrong.
Open (Hasson) Technique
The Open or Hasson technique involves a small cut in the abdominal wall. It lets the surgeon see directly into the cavity. This method is safer for those with past abdominal surgery.
Benefits: It allows for direct vision, lowering the risk of organ damage.
The table below compares the Veress needle technique with the Open (Hasson) technique:
Technique | Advantages | Potential Risks |
Veress Needle | Quick, less invasive | Risk of organ or vessel injury |
Open (Hasson) | Direct visualization, safer in patients with previous surgery | More invasive, longer setup time |
Direct Trocar Insertion
Direct trocar insertion involves putting the trocar straight into the cavity without gas first. It needs careful handling to avoid injury.
Optical Access Technique
The optical access technique uses a trocar with a camera. It lets the surgeon see the layers of the abdominal wall as they insert the trocar. This helps avoid injuries.
Each technique has its role in surgery. The choice depends on the patient, the surgeon, and the procedure’s needs.
Muscles Cut During Laparoscopic Surgery
It’s important for patients and surgeons to know how laparoscopic surgery affects abdominal muscles. This surgery tries to cut down on muscle damage. This helps reduce pain after surgery and speeds up recovery.
The Truth About Muscle Cutting in Laparoscopy
Laparoscopic surgery uses small cuts for instruments and a camera. It’s designed to avoid cutting muscles. Instead, it uses natural paths to reach the surgery area.
“The laparoscopic approach significantly reduces the trauma to the abdominal wall, leading to less post-operative pain and quicker recovery times.”
Muscle Splitting vs. Muscle Cutting
In laparoscopic surgery, muscle splitting is used. It separates muscle fibers without cutting. This method reduces muscle damage and speeds up healing.
Technique | Description | Impact on Muscles |
Muscle Cutting | Involves cutting through muscle fibers | Higher risk of muscle damage |
Muscle Splitting | Separates muscle fibers without cutting | Less muscle trauma, faster recovery |
Tissue Displacement Techniques
Tissue displacement techniques gently move tissues apart. This creates a clear path to the surgery area without harming muscles.
Minimizing Muscle Trauma
Reducing muscle trauma is a main goal in laparoscopic surgery. Using smaller cuts and precise tools helps achieve this.
Strategies for Minimizing Muscle Trauma:
- Using minimally invasive techniques
- Employing muscle-splitting instead of cutting
- Utilizing advanced surgical instruments
By using these strategies, surgeons can lessen the effects of laparoscopic surgery on abdominal muscles. This leads to better results for patients.
Trocar Placement and Muscle Impact
The way trocars are placed in laparoscopic surgery affects how much muscle trauma patients feel. It’s important to place them carefully to reduce trauma and help patients recover faster.
Common Trocar Locations
Doctors usually put trocars in spots that give them the best view of the area they’re working on. They try to avoid hurting muscles too much. Common spots include:
- The umbilical region, which often serves as the primary access point.
- The lower midline or suprapubic area for additional ports.
- Lateral positions, such as the left or right lower quadrants.
How Trocars Interact with Muscle Tissue
Trocar placement can affect different muscle layers in the abdominal wall. The amount of muscle damage depends on:
- Angle of insertion: A more oblique angle can increase muscle trauma.
- Size of the trocar: Larger trocars tend to cause more significant tissue disruption.
- Technique used: Methods like the “Z-track” technique can help minimize trauma.
Minimizing Muscle Trauma During Port Placement
To lessen muscle trauma, doctors use several strategies, including:
- Muscle splitting instead of cutting.
- Using smaller trocars when possible.
- Careful planning of trocar sites to avoid major muscle groups.
Understanding how trocar placement affects muscles and using techniques to lessen trauma helps surgeons. This improves patient outcomes and shortens recovery times.
Specific Muscles Affected in Laparoscopic Procedures
Laparoscopic surgery affects certain muscles. It involves small cuts in the abdominal wall, which has many muscle layers. Knowing these muscles helps understand how laparoscopy impacts the abdominal wall.
Rectus Abdominis (Are Abs Cut?)
The rectus abdominis, or “abs,” is a key muscle in the abdominal wall. In laparoscopic surgery, the “abs” are not usually cut. Instead, small tools are inserted around it. Sometimes, the muscle is moved aside for access.
This muscle is vital for core strength. Keeping it intact is a main goal in laparoscopic surgery.
External and Internal Obliques
The external and internal oblique muscles are also important. They help with rotational movements and add strength to the abdominal wall. During surgery, these muscles may be touched by tools but are not cut.
These muscles help keep the core stable. Keeping them intact is key to avoiding complications after surgery.
Transversus Abdominis
The transversus abdominis is the deepest muscle in the abdomen. It helps compress the abdominal contents and supports the spine. This muscle is not directly involved in the usual entry points of laparoscopic surgery.
Yet, it is affected by the changes in the abdominal wall after surgery. It plays a big role in core strength and stability.
Impact on Core Strength
The effect of laparoscopic surgery on core strength is a big worry for patients. Even though laparoscopic methods try to avoid muscle damage, the muscles are stressed during the surgery. The impact on core strength depends on the surgery type, the surgeon’s skill, and the patient’s health before surgery.
Generally, laparoscopic surgery causes less muscle damage than open surgery. This might lead to a faster recovery of core strength.
Laparoscopic Incisions and Their Size
Laparoscopic incisions are key in minimally invasive surgery. They affect both the surgery’s success and the patient’s recovery. The size and number of these incisions change based on the surgery type.
Typical Incision Sizes
Laparoscopic incisions are usually small, between 0.5 to 1.5 cm long. These small sizes help reduce tissue damage and speed up healing. The exact size depends on the surgery, the surgeon’s choice, and the tools used.
Single-Incision vs. Multiple-Port Laparoscopy
Laparoscopic surgeries can be done with one or multiple incisions. Single-incision laparoscopy uses one larger incision, usually at the belly button, for all tools. This method can make the scar less noticeable. In contrast, multiple-port laparoscopy uses several small incisions, allowing for better tool movement.
Incision Placement Considerations
Surgeons plan where to make laparoscopic incisions carefully. They aim to hide scars and avoid complications. They consider the organ’s location, the patient’s body, and past scars when deciding.
Cosmetic Outcomes
Cosmetic results are important in laparoscopic surgery. Smaller incisions mean less visible scarring. Techniques like single-incision laparoscopy can improve looks by reducing scars.
Muscle-Sparing Techniques in Modern Laparoscopy
Modern laparoscopy has made big strides in muscle-sparing techniques. This has greatly improved patient recovery and results. It’s all about reducing the harm caused by surgery.
Advancements in Port Technology
New port technology is key in muscle-sparing laparoscopy. Ports with bladeless trocars and radially dilating systems cause less muscle damage. This leads to quicker healing.
Here’s a look at old and new port tech:
Feature | Traditional Ports | Modern Ports |
Trocar Type | Bladed | Bladeless |
Muscle Damage | Higher | Lower |
Healing Time | Longer | Shorter |
Muscle-Preserving Entry Methods
Surgeons use new ways to enter the body, like the Open (Hasson) Technique and Optical Access Technique. These methods aim to lessen muscle damage during entry.
Surgeon Training and Technique Importance
The success of these techniques depends a lot on surgeon training and using the right methods. Surgeons need ongoing education to keep up with new methods.
Training programs now stress the value of muscle-sparing techniques. They highlight how it reduces muscle trauma and boosts patient results.
Healing Process of Muscles After Laparoscopy
Laparoscopic surgery starts a healing process in the body’s muscles. This process has different stages, from right after surgery to long-term recovery.
Immediate Post-Operative Changes
Right after laparoscopic surgery, the body’s muscles go through big changes. The surgery causes inflammation, which is part of healing. This first stage includes swelling, pain, and limited movement in the affected area.
The use of minimally invasive techniques in laparoscopic surgery causes less damage than open surgery. This leads to less pain and faster recovery times.
Short-Term Healing (1-4 Weeks)
In the short-term healing phase, the body starts to fix the muscle tissue damaged during surgery. This involves turning on various cellular processes that help repair and grow new tissue.
- The inflammation starts to go down as the tissue heals.
- Patients usually feel less pain and can move better.
- Doctors often suggest gentle exercises to keep blood flowing and prevent muscle loss.
Long-Term Muscle Recovery
Long-term muscle recovery after laparoscopic surgery can take months. During this time, the muscle tissue gets stronger, and the abdominal wall gets back to its pre-surgery strength and function.
Proper post-operative care and following the doctor’s advice are key for the best long-term recovery.
Factors Affecting Healing Speed
Several things can affect how fast and well muscles heal after laparoscopic surgery. These include:
Factor | Description | Impact on Healing |
Age | Older patients may heal slower because their cells regenerate less. | Slower recovery |
Overall Health | Medical conditions before surgery can affect healing. | Variable impact |
Surgical Technique | The surgeon’s skill and technique used can affect tissue damage and healing. | Faster recovery with minimally invasive techniques |
The healing process after laparoscopic surgery is influenced by these factors. This shows why personalized post-operative care is so important.
Potential Muscle Complications After Laparoscopy
Muscle problems after laparoscopic surgery are rare but serious. Laparoscopy is seen as a minimally invasive method. Yet, it can cause muscle issues due to entry points and tissue manipulation.
Muscle Weakness
Muscle weakness is a possible complication. It can happen when muscle fibers are disrupted during trocar insertion. Muscle weakness might make the abdominal wall weaker, affecting posture and physical activities.
A study in the Journal of Surgical Research showed significant abdominal wall weakness after laparoscopic cholecystectomy. This weakness was mostly gone by 3 months. But, recovery times can differ for everyone.
Trocar Site Hernias
Trocar site hernias are another issue. They happen when intestine or tissue bulge out through a trocar site. These hernias are more common at larger trocar sites or in people with obesity or past abdominal surgeries.
Risk Factor | Description | Prevention Strategy |
Large Trocar Size | Increased risk of herniation | Use of smaller trocars when possible |
Obesity | Increased intra-abdominal pressure | Closure of fascia at trocar sites |
Previous Abdominal Surgery | Weakened abdominal wall | Careful selection of trocar sites |
Abdominal Wall Hematomas
Abdominal wall hematomas are blood collections outside blood vessels. They can happen when vessels are injured during trocar placement. These hematomas can cause pain, swelling, and might lead to infection if not treated right.
“The incidence of abdominal wall hematomas can be minimized by careful technique during trocar insertion and by selecting appropriate entry sites.” – Medical Expert, Surgical Expert.
Managing abdominal wall hematomas usually involves watching the condition, controlling pain, and sometimes draining the hematoma.
In summary, muscle complications after laparoscopy are rare but important to know. Understanding these risks helps surgeons and patients. By knowing the risks and taking steps to prevent them, we can lower the chance of these complications.
Recovery and Rehabilitation of Muscles
Recovering well after laparoscopic surgery is key to getting back to normal. Good care and exercises help patients get back to their daily lives fast and safely.
Post-Operative Activity Guidelines
Patients need to follow certain rules after surgery. They should avoid lifting heavy things, bending, or doing hard activities for a while.
- Avoid heavy lifting for 4-6 weeks
- Gradually increase physical activity
- Follow the surgeon’s specific instructions
Exercises to Restore Muscle Function
There are special exercises to help muscles recover after surgery. These might include:
- Deep breathing exercises
- Gentle stretching
- Core strengthening exercises, once cleared by the surgeon
Example Exercise Routine
Exercise | Day | Repetitions |
Deep Breathing | 1-5 | 10 times/hour |
Gentle Stretching | 3-7 | 5 repetitions, 2 times/day |
Core Strengthening | 14+ | 10 repetitions, 3 times/day |
Timeline for Return to Normal Activities
How long it takes to get back to normal varies. It depends on the surgery and the person’s health. Usually, most people can get back to normal in a few weeks.
When to Seek Medical Attention
Knowing when to get help is important during recovery. If you have:
- Increasing pain
- Fever
- Unusual discharge or bleeding
By following the right steps, doing the right exercises, and knowing when to get help, patients can recover well after laparoscopic surgery.
Common Laparoscopic Procedures and Their Impact on Muscles
It’s important to know how laparoscopic surgery affects muscles. This type of surgery is less invasive and has changed how we treat many conditions in the abdomen and pelvis. The effects on muscles can affect how quickly a patient recovers and their long-term health.
Laparoscopic Cholecystectomy
The removal of the gallbladder through laparoscopic surgery is very common. It uses three to four small cuts in the belly. This method is kind to the muscles because it doesn’t cut them but moves them aside.
The rectus abdominis and oblique muscles are usually not cut. Surgeons use special techniques to split the muscles instead. This helps reduce pain and speeds up recovery for patients.
Gynecological Laparoscopic Procedures
Gynecological surgeries, like removing the uterus or ovaries, also affect muscles. These surgeries need careful trocar placement to avoid muscle damage.
Doctors might choose between single-incision laparoscopy or the traditional multi-port method. The choice affects how much the muscles are impacted and how fast the patient recovers.
Laparoscopic Hernia Repair
Laparoscopic hernia repair fixes weak spots in the abdominal wall to prevent hernias from coming back. This surgery can be tricky because it involves moving the hernia sac and placing mesh.
The placement of mesh behind the muscles requires careful work and can cause temporary weakness. But, it’s less damaging than open surgery.
In summary, different laparoscopic surgeries affect muscles in different ways. Knowing these differences helps doctors manage patient expectations and improve surgical techniques to reduce muscle damage.
Patient Experiences and Expectations
Laparoscopic procedures are becoming more common. This has sparked interest in what patients go through and what they expect. It’s important to know their concerns and how they do after surgery.
Common Patient Concerns About Muscle Damage
Many patients worry about muscle damage during laparoscopic surgery. They fear that the surgery might cut or harm their muscles.
Some common worries are:
- How much muscle damage might happen during the surgery
- How it will affect their recovery after surgery
- If it could weaken their muscles in the long run
Real Patient Testimonials
Real stories from patients who’ve had laparoscopic surgery offer valuable insights. These stories can help ease worries and set realistic hopes.
“I was worried about muscle damage from laparoscopic surgery, but my surgeon explained that the procedure is designed to minimize trauma to the abdominal muscles. The recovery was smoother than I expected.”
— Sarah, Laparoscopic Cholecystectomy Patient
These stories show how important it is for doctors to talk clearly with their patients. They also highlight the need for patients to be well-informed.
Managing Expectations
It’s key to manage what patients expect for a good outcome. This means talking openly about the surgery, its risks, and what to expect after.
Expectation | Reality |
Significant muscle damage | Laparoscopic surgery minimizes muscle cutting, reducing trauma |
Severe post-operative pain | Most patients experience manageable pain with appropriate medication |
Long recovery time | Typically, patients recover within a few weeks, depending on the procedure |
Knowing the truth about laparoscopic surgery helps patients prepare better. It makes them more ready for what’s to come.
Conclusion
Laparoscopic surgery has changed the way we do surgery. It uses small cuts and tools to fix problems inside the body. This method is kinder to muscles, leading to faster healing times.
The way laparoscopic surgery works is smart. It splits muscles and moves tissues aside. This means less pain after surgery and a quicker comeback to daily life. It’s a big win for those who have to go through it.
In short, laparoscopic surgery is a top choice for many surgeries. It’s less invasive, which is good for patients. Knowing how it works helps both patients and doctors choose the best option for each case.
FAQ
Are muscles cut during laparoscopic surgery?
Laparoscopic surgery makes small cuts in the belly. How much muscle is cut depends on the surgery and the method used. Surgeons try to split muscles to cause less damage.
What is the difference between muscle cutting and muscle splitting in laparoscopic surgery?
Muscle cutting means cutting through the muscle. Muscle splitting means separating the muscle fibers without cutting through. This way, the muscle is less damaged.
How do laparoscopic entry techniques affect muscle tissue?
Different ways to start laparoscopic surgery affect muscles differently. Some methods are designed to hurt muscles less.
What are the most common muscles affected during laparoscopic surgery?
The main muscles affected are the rectus abdominis, external and internal obliques, and transversus abdominis. The impact varies based on where the trocars are placed and the surgery type.
How do trocar placements affect muscle tissue during laparoscopic surgery?
Where trocars are placed matters a lot. Placing them carefully can reduce muscle damage. This is done by placing them between muscle fibers or in less muscular areas.
What are the benefits of muscle-sparing techniques in laparoscopic surgery?
Muscle-sparing techniques minimize muscle damage.They also lower post-operative pain and speed up recovery. This is thanks to better port technology and surgeon training.
How long does it take for muscles to heal after laparoscopic surgery?
Muscle healing after laparoscopic surgery varies. Immediate changes happen in the first few days. Short-term healing takes 1-4 weeks. Long-term recovery can take months.
What are the possible muscle complications after laparoscopic surgery?
Muscle complications include weakness, hernias at trocar sites, and hematomas. Knowing these risks helps manage expectations and prevent them.
What are the guidelines for post-operative activity after laparoscopic surgery?
Guidelines suggest a slow return to normal activities. Avoid heavy lifting and strenuous exercises at first. Specific guidelines depend on the surgery and surgeon’s advice.
Are there exercises to restore muscle function after laparoscopic surgery?
Yes, there are exercises to help muscles recover. These include gentle stretching and core strengthening. Physical therapy is tailored to the individual and surgery type.
How do different laparoscopic procedures impact muscle recovery?
Different procedures affect muscle recovery differently. The extent of muscle trauma and techniques used influence recovery. This varies between procedures like cholecystectomy, gynecological surgeries, and hernia repair.
What are common patient concerns about muscle damage during laparoscopic surgery?
Patients worry about muscle damage, pain, and losing core strength. Educating them about muscle-sparing techniques helps manage these concerns.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/8433390/