Last Updated on November 4, 2025 by mcelik

Osteoarthritis flare-ups are a common concern for millions of people around the world. Osteoarthritis is a prevalent condition that causes pain, stiffness, and limits movement. In the U.S., about 27 million Americans suffer from it — and this number is expected to grow as more people age and obesity rates increase.
Understanding what triggers osteoarthritis flare-ups is key to managing the disease effectively. Many factors can contribute to these painful episodes, including lifestyle habits, environmental changes, and physical strain. Recognizing and addressing these causes can help reduce osteoarthritis flare-ups and improve overall joint health.
Key Takeaways
- Understanding osteoarthritis triggers is vital for effective disease management.
- Lifestyle and environmental factors can contribute to osteoarthritis flare-ups.
- Identifying personal triggers can help individuals take proactive steps.
- Managing osteoarthritis requires a holistic approach.
- Simple changes can significantly reduce symptoms.
Understanding Osteoarthritis and Its Symptoms
Osteoarthritis is a disease that affects joints, causing pain and disability. It’s important to know how it works and its symptoms to manage it well.
What Happens in Osteoarthritis?
In osteoarthritis, the cartilage in joints wears down. This leads to bones rubbing against each other. The Arthritis Foundation says this causes pain and inflammation. It also causes bone spurs and joint deformation.
Recognizing the Signs of Osteoarthritis
The symptoms of osteoarthritis vary. Common signs include pain, stiffness, and limited mobility. Some people might hear a crunching sound when moving a joint. Key symptoms to watch for are:
- Pain that worsens with activity
- Stiffness, mainly in the morning
- Swelling around the affected joint
- Decreased range of motion
The Role of Inflammation in Joint Damage
Inflammation is key in osteoarthritis. When cartilage breaks down, it irritates the joint. This causes more pain and damage. Controlling inflammation is vital to slow the disease.
Identifying Osteoarthritis Flare-ups
An osteoarthritis flare-up is when symptoms suddenly get worse. This can really affect how you live your day. Knowing what a flare-up is and how to spot it is key to managing it well.
Defining an Osteoarthritis Flare-up
A flare-up means a big jump in pain, swelling, and stiffness in your joints. Medical News Today says this can make simple tasks hard to do.
How to Recognize When a Flare-up is Beginning
Early flare-up signs include more pain when moving a joint, less range of motion, and swelling. Knowing these signs helps you act fast to control the flare-up.
Duration and Intensity of Typical Flare-ups
How long and how bad flare-ups are can vary a lot. Things like how bad your osteoarthritis is, your health, and triggers like injury or too much use can affect it.
Knowing this can help you get ready for and handle flare-ups better. This might make them less of a problem in your daily life.
Physical Overexertion and Joint Strain
Doing too much physical activity can worsen osteoarthritis symptoms. People with osteoarthritis should be careful when doing strenuous activities. This helps avoid making their condition worse.
Joint Overuse and Its Effects
Joint overuse happens when a joint is stressed too much. This stress can come from work or hobbies. It can cause more inflammation and pain for those with osteoarthritis. It’s important to lower the risk of joint overuse to manage osteoarthritis symptoms well.
Repetitive Movements and Osteoarthritis
Jobs or sports that involve repetitive movements can harm joints. This can make osteoarthritis worse faster. Changing or stopping these movements can lessen the damage.
High-Impact Activities to Avoid
High-impact activities like running or jumping can strain joints too much. People with osteoarthritis should avoid or change these activities. This can help prevent flare-ups.
Modifications for Common Activities
Changing daily and fun activities can help protect joints. For example, switching to swimming or cycling instead of high-impact sports is good.
Joint-Friendly Exercise Alternatives
Doing exercises that are easy on the joints is key. Activities like yoga or tai chi can improve flexibility and balance. They are also gentle on the joints.
Weather-Related Triggers
Osteoarthritis symptoms can be influenced by various weather-related factors. Many individuals with osteoarthritis report that changes in weather conditions can trigger or worsen their symptoms.
Cold Weather and Joint Pain
Cold weather is often cited as a factor that exacerbates osteoarthritis symptoms. The cold can cause the joints to become stiffer and more painful. This is because cold temperatures can increase the thickness of the fluid in the joints, making them less flexible and more prone to pain.
Humidity and Barometric Pressure Changes
Changes in humidity and barometric pressure are also believed to affect osteoarthritis symptoms. Some people find that high humidity or changes in atmospheric pressure can increase their joint pain. The exact mechanism is not fully understood, but it’s thought that changes in pressure may cause the tissues to expand, irritating the nerves around the joints.
Seasonal Patterns in Osteoarthritis Symptoms
Many people with osteoarthritis notice a seasonal pattern to their symptoms. For some, symptoms worsen in the winter due to the cold, while others may experience more discomfort in damp or humid conditions. Understanding these patterns can help individuals prepare and manage their symptoms more effectively.
Strategies for Managing Weather-Related Pain
To manage weather-related osteoarthritis pain, individuals can take several steps. Staying warm during cold weather, using heating pads, or taking warm baths can help alleviate stiffness and pain. Maintaining a healthy weight, staying physically active, and using appropriate medications as prescribed by a healthcare provider can also help manage symptoms.
Weight Management and Osteoarthritis
For those with osteoarthritis, managing weight is key, not just for looks. The Arthritis Foundation says a healthy weight is vital to ease joint strain.
How Extra Weight Impacts Joints
Extra weight adds stress to joints like knees and hips. This extra pressure speeds up cartilage wear, making osteoarthritis worse. For every pound, joints bear more weight.
The Connection Between Weight Gain and Inflammation
Weight gain also leads to chronic inflammation. Fat tissue makes substances that can make osteoarthritis symptoms worse. Keeping a healthy weight can lower inflammation.
Benefits of Weight Loss for Osteoarthritis Patients
Weight loss helps those with osteoarthritis a lot. Losing 5-10% of body weight can improve joint function and reduce pain.
“Weight loss is one of the most effective ways to manage osteoarthritis, for those who are overweight or obese.”
Sustainable Approaches to Weight Management
Effective weight management needs diet changes, more exercise, and lifestyle tweaks. Eating well and exercising regularly helps keep weight in check. It’s about making lasting lifestyle changes, not quick fixes.
Dietary Factors That Influence Osteoarthritis
Certain foods can make osteoarthritis symptoms better or worse. Knowing how diet affects osteoarthritis is key to managing it well.
Inflammatory Foods to Avoid
Some foods can make inflammation in osteoarthritis worse. Avoid processed meats, sugary drinks, and refined carbohydrates. Eating these foods often can increase joint pain and swelling.
Anti-inflammatory Diet Recommendations
Eating foods that fight inflammation can help with osteoarthritis. Foods like omega-3 fatty acids in salmon and sardines are good. Also, eating lots of antioxidants in fruits and veggies can lower inflammation.
Hydration and Joint Health
Drinking enough water is key for healthy joints. Not drinking enough can lower the fluid that keeps joints moving, making osteoarthritis symptoms worse. It’s important to drink water all day.
Supplements and Their Evidence Base
Some supplements, like glucosamine and chondroitin, are used by people with osteoarthritis. While they work differently for everyone, some studies show they can help some people feel better.
| Supplement | Potential Benefits |
| Glucosamine | May help maintain cartilage health |
| Chondroitin | May reduce joint pain and inflammation |
| Omega-3 Fatty Acids | Anti-inflammatory effects |
By choosing the right foods, people with osteoarthritis can lessen their symptoms and live better lives.
Physical Inactivity and Its Consequences
Lack of exercise can make osteoarthritis worse. It leads to less joint function and health. People with osteoarthritis who don’t move much feel stiffer and more painful joints.
How Lack of Exercise Affects Joint Health
Not moving enough makes joints stiffer and muscles weaker. This makes everyday tasks harder. Also, not exercising can cause weight gain, which adds stress to joints like hips, knees, and spine.
The Importance of Regular Movement
Regular exercise is key for joint health and overall well-being. It keeps joints moving, strengthens muscles, and can lessen pain.
| Exercise Type | Benefits for Osteoarthritis |
| Aerobic Exercise | Improves cardiovascular health, reduces pain |
| Strengthening Exercises | Builds muscle around the joints, enhances stability |
| Flexibility Exercises | Maintains or improves range of motion, reduces stiffness |
Finding the Right Balance of Activity
Finding the right balance between rest and activity is important. Too much can make osteoarthritis symptoms worse. Too little can cause stiffness and less mobility.
Building a Joint-Friendly Exercise Routine
Creating an exercise plan that’s easy on the joints is essential. Swimming, cycling, and tai chi are good choices for those with osteoarthritis.
Stress and Psychological Factors
Stress and psychological factors greatly affect how people with osteoarthritis feel pain. The connection between the mind and body is key. It shows how stress can make osteoarthritis symptoms worse.
The Mind-Body Connection in Osteoarthritis
The mind and body in osteoarthritis are closely linked. Stress can make pain feel more intense. This is why managing stress is vital in treating osteoarthritis.
How Stress Amplifies Pain Perception
Stress in osteoarthritis patients leads to the release of stress hormones like cortisol. These hormones can increase inflammation and make pain worse.
Sleep Problems and Their Impact on Joint Pain
Many with osteoarthritis struggle with sleep. Poor sleep can make pain feel worse. This creates a cycle of pain and sleep issues.
Stress Management Techniques for Arthritis Patients
Managing stress is key for osteoarthritis patients. Methods like meditation, deep breathing, and physical therapy can help. They reduce stress and ease symptoms.
| Stress Management Technique | Description | Benefits |
| Meditation | Practice mindfulness and relaxation | Reduces stress, improves pain tolerance |
| Deep Breathing Exercises | Slow, deliberate breathing | Lowers stress hormones, promotes relaxation |
| Physical Therapy | Guided exercises for joint mobility | Improves joint function, reduces pain |
By using these stress management techniques, osteoarthritis patients can lessen their pain. They can also improve their overall health.
Poor Posture and Body Mechanics
The way we move and hold our posture greatly affects osteoarthritis symptoms. Bad posture and body mechanics can strain joints more. This can make osteoarthritis symptoms worse or start them.
Impact on Joint Loading
Poor posture changes how weight is spread across joints. This uneven wear can damage joint cartilage, a key sign of osteoarthritis. For example, slouching or leaning forward can hurt hips and knees more.
Workplace Ergonomics
Many people spend a lot of time at work, often in bad positions. It’s key to make work areas ergonomic. This means using chairs with good lumbar support, setting up computer monitors right, and taking breaks to move.
Correcting Movement Patterns
Changing how we move can lessen joint strain. We should be aware of our posture and use the right lifting techniques. Physical therapy can help find and fix harmful movement habits.
Assistive Devices for Joint Protection
Using assistive devices can help protect joints. Things like canes, walkers, and ergonomic tools are good examples. They help spread weight evenly and lower the chance of making osteoarthritis symptoms worse.
| Assistive Device | Benefit |
| Canes | Reduces weight-bearing stress on lower limb joints |
| Ergonomic Tools | Minimizes strain during daily tasks |
| Walkers | Provides additional support and stability |
Managing and Preventing Osteoarthritis Flare-ups
Managing osteoarthritis needs a mix of medicine, lifestyle changes, and prevention. Knowing what triggers flare-ups and using the right strategies can help. This way, people can lessen how often and how bad flare-ups get.
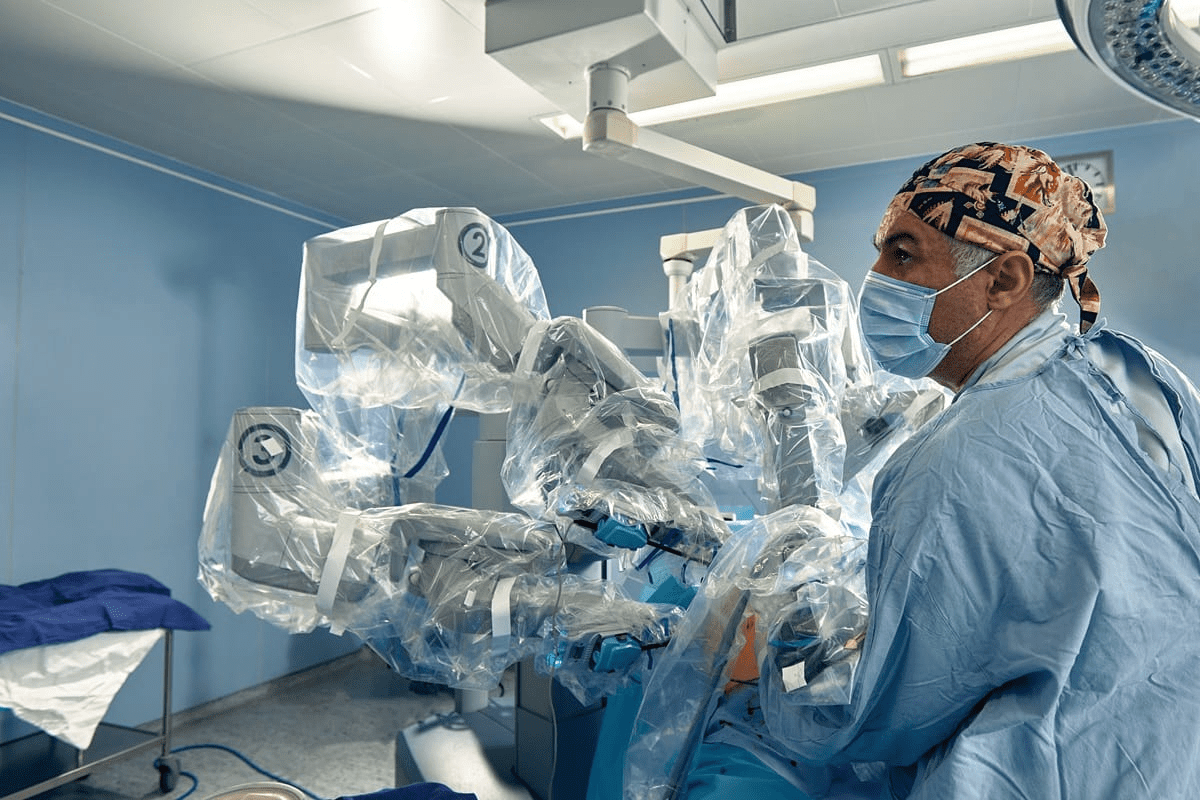
Medication Options for Acute Flares
For quick osteoarthritis flare-ups, there are many medicines. Nonsteroidal anti-inflammatory drugs (NSAIDs) are often used to cut pain and swelling. For really bad flare-ups, corticosteroid injections might be suggested.
Non-pharmaceutical Pain Management Techniques
There are also ways to manage pain without medicine. Physical therapy, acupuncture, and using heat or cold therapy can help. These methods can work better when used with medicine.
Physical Therapy Approaches
Physical therapy is key in managing osteoarthritis. It makes joints move better and muscles stronger. A custom exercise plan can lessen pain and improve how well you can move.
Creating a Personalized Flare-up Prevention Plan
Creating a plan to stop flare-ups means finding out what triggers them for you. This might include lifestyle changes like losing weight, exercising regularly, and avoiding activities that hurt your joints.
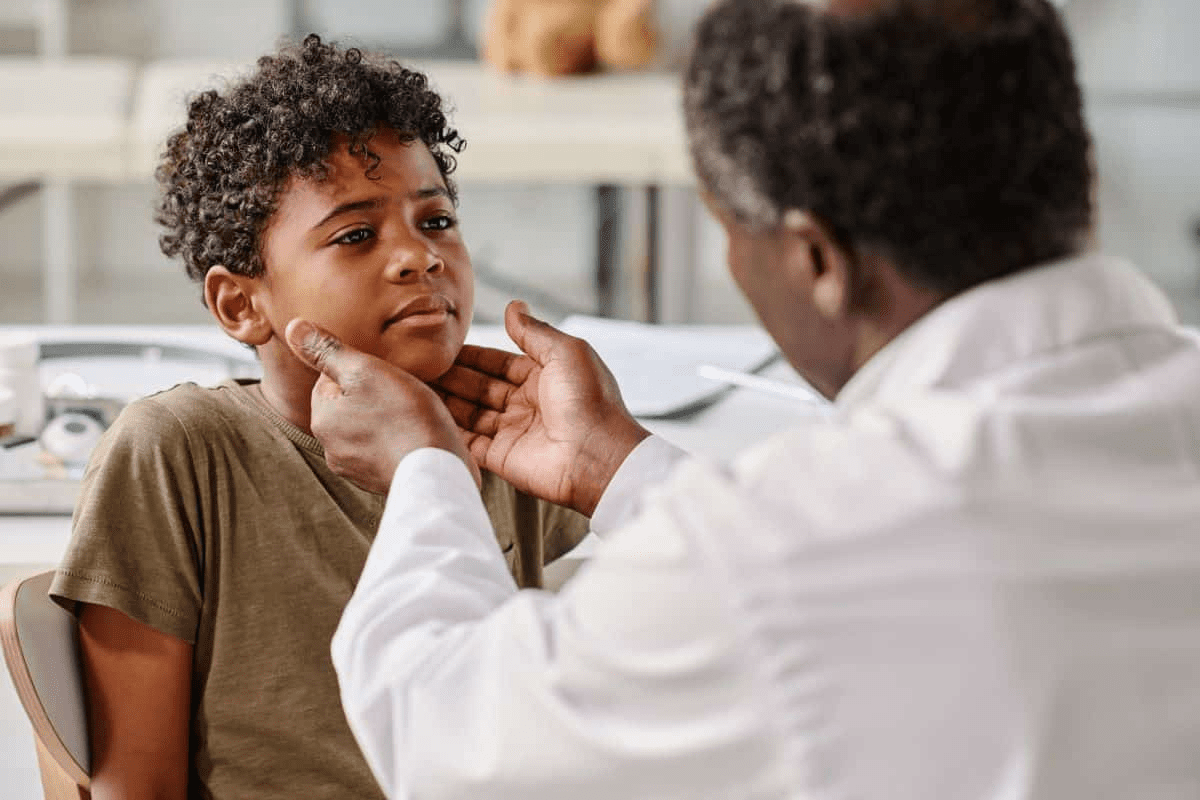
When to Seek Medical Attention
Knowing when to see a doctor is important. If a flare-up is very bad or if your joints are badly damaged, you need medical help. Regular visits to your healthcare provider can also help manage your condition well.
Conclusion
Understanding osteoarthritis flare-ups and their triggers is key to managing the disease. Knowing what causes these flare-ups helps people take steps to reduce their impact.
Many things can trigger osteoarthritis flare-ups, like too much physical activity, weather changes, weight gain, and certain foods. To manage these triggers, making lifestyle changes and practicing self-care is important.
Keeping a healthy weight, doing gentle exercises regularly, and watching what you eat can help. These actions can make flare-ups less frequent and less severe.
Being proactive in managing osteoarthritis can greatly improve your life. It helps you stay functional and active, even with the disease’s challenges.
FAQ
What are the common triggers for osteoarthritis flare-ups?
Triggers include overexertion, joint strain, and weather changes. Weight gain, repetitive movements, and stress also play a role. Poor posture and injury can also trigger flare-ups.
How does cold weather affect osteoarthritis symptoms?
Cold weather can make joint pain and stiffness worse. This is likely due to changes in barometric pressure and muscle tension.
Can diet influence osteoarthritis symptoms?
Yes, some foods can make symptoms worse. Avoiding inflammatory foods and eating anti-inflammatory foods can help manage symptoms.
How does weight gain affect osteoarthritis?
Extra weight strains joints, like hips and knees. It can also increase inflammation, making symptoms worse.
What role does stress play in osteoarthritis?
Stress can make pain worse. Managing stress can help reduce symptoms.
How can I manage osteoarthritis symptoms during weather changes?
Stay warm and use heat or cold therapy. Adjust your activity levels and use assistive devices to reduce strain.
Are there specific exercises that can help manage osteoarthritis?
Yes, low-impact exercises like swimming and cycling are good. Gentle stretching also helps maintain joint mobility and strength.
How can poor posture contribute to osteoarthritis?
Poor posture can lead to uneven joint loading. This increases strain on certain joints and can speed up osteoarthritis progression.
What are some effective stress management techniques for osteoarthritis patients?
Techniques include meditation, deep breathing, and yoga. Cognitive-behavioral therapy also helps reduce stress and improve well-being.
When should I seek medical attention for an osteoarthritis flare-up?
Seek medical help if symptoms worsen significantly. Look for a big increase in pain or a decrease in mobility or function.
References
- Valdes, A. M., Doherty, S., Zhai, G., et al. (2021). Triggers for acute flare in adults with, or at risk of, knee osteoarthritis: a web-based case-crossover study in community-dwelling adults. Osteoarthritis and Cartilage, 29(8), 1013–1022. https://pubmed.ncbi.nlm.nih.gov/33933585/