Last Updated on November 27, 2025 by Bilal Hasdemir
What is the other name for fallopian tube cancer? Fallopian tube cancer is a rare condition that’s not often talked about.
This cancer hits the female reproductive system. It affects the tubes that link the ovaries to the uterus. It’s also called primary Fallopian tube carcinoma or tubal carcinoma. Knowing these names is key for understanding diagnosis and treatment.
This article provides a detailed overview to help both patients and healthcare providers make informed decisions.

Key Takeaways
- Fallopian tube cancer is a rare malignancy affecting the female reproductive system.
- It is also known as primary Fallopian tube carcinoma or tubal carcinoma.
- Understanding these terms is vital for diagnosis and treatment.
- Patients and healthcare providers must be aware of the condition.
- Comprehensive support is essential for international patients seeking medical care.
Understanding Fallopian Tube Cancer
Fallopian tube cancer is rare but affects many women’s health worldwide. It’s important to know its basics, like what it is and how common it is.
Definition and Basic Overview
Fallopian tube cancer starts in the Fallopian tubes. These tubes link the ovaries to the uterus. This cancer grows in the lining of the tubes. The exact cause is not fully known, but it’s linked to genetic changes and other factors.
We’ll look into this cancer’s details, like its effects on the body. Knowing what it is helps us understand its seriousness for women’s health.
Prevalence and Significance
Fallopian tube cancer is a rare gynecologic cancer. It’s a small part of all gynecologic cancers. Studies show it’s less common than ovarian or cervical cancer.
| Type of Cancer | Estimated Incidence | Percentage of Gynecologic Cancers |
| Fallopian Tube Cancer | 1-2 per 100,000 women | 0.5-1% |
| Ovarian Cancer | 10-15 per 100,000 women | 20-25% |
| Cervical Cancer | 7-8 per 100,000 women | 10-15% |
Even though it’s rare, Fallopian tube cancer is serious. It’s often found late and is hard to treat. Knowing about it is key for early detection and better care.
Alternative Names for Fallopian Tube Cancer
Fallopian tube cancer has many names in medical books. Knowing these terms helps doctors and patients talk clearly. Different names show the disease’s complexity and details.
Primary Fallopian Tube Carcinoma (PFTC)
Primary Fallopian Tube Carcinoma (PFTC) is a common term. It means the cancer starts in the fallopian tube. This is different from cancers that spread to the fallopian tube from elsewhere. PFTC is rare and needs careful checking to find where it started.
“The term PFTC highlights the importance of identifying the primary site of the cancer, which has implications for treatment and prognosis.”
Tubal Carcinoma
Tubal Carcinoma just means cancer of the fallopian tube. It’s a simple term but specific to the fallopian tube. Doctors often use it in medical talks.
Fallopian Tube Malignancy
Fallopian Tube Malignancy covers cancers of the fallopian tube. It includes not just carcinomas but other cancers too. Carcinomas are the most common type, though.
In summary, fallopian tube cancer has many names. But they all point to cancer in the fallopian tubes. Knowing these names helps in talking about diagnosis, treatment, and research.
The Relationship Between Fallopian Tube Cancer and Ovarian Cancer
Recent studies have shown a strong link between fallopian tube cancer and ovarian cancer, mainly in high-grade serous carcinoma (HGSC). We’re learning that these cancers share origins and traits more than we thought.
For a long time, we didn’t see the difference between fallopian tube and ovarian cancer. But, new research is clearing up these misunderstandings.
Historical Classification Differences
Before, we diagnosed these cancers based on where they were in the body. But this method missed the similarities, like in HGSC.
This old way of thinking made it hard to diagnose and treat these cancers correctly.
Modern Understanding of Origins
Now, we think many ovarian cancers, like HGSC, start in the fallopian tubes. This new knowledge helps us find and stop these cancers early.
Research shows that HGSC often starts in the fallopian tube’s fimbriated end. Then, it can spread to the ovaries.
High-Grade Serous Carcinoma (HGSC)
HGSC is a fast-growing cancer type linked to both fallopian tube and ovarian cancers. Knowing its molecular details is key to creating better treatments.
| Cancer Type | Characteristics | Common Origin |
| Fallopian Tube Cancer | Often presents with HGSC | Shared origin in the fallopian tube, mainly the fimbriated end |
| Ovarian Cancer | HGSC is a common subtype |
Understanding the connection between fallopian tube and ovarian cancer helps us get better at diagnosing and treating these diseases.
Serous Tubal Intraepithelial Carcinoma (STIC)
STIC, or Serous Tubal Intraepithelial Carcinoma, is a precursor to high-grade serous carcinoma, a common and aggressive ovarian cancer. Knowing about STIC is key for early detection and prevention of ovarian cancer.
Definition and Significance
Serous Tubal Intraepithelial Carcinoma is when abnormal cells are found in the fallopian tube lining. These cells can turn into high-grade serous carcinoma (HGSC), a fast-growing and serious cancer. STIC is important because it can lead to HGSC, giving us a chance to act early.
Identifying STIC in people at risk, like those with BRCA1 and BRCA2 mutations, is critical. Finding STIC early can stop HGSC from developing, which can greatly improve patient outcomes.
Role as Precursor Lesion
STIC is a precursor to HGSC because it has similar genetic changes. Research shows STIC often comes before HGSC, showing a path from STIC to invasive cancer. Knowing this path helps us find better ways to prevent and treat cancer.
Having STIC means a higher risk of getting HGSC. So, finding and managing STIC is key to stopping ovarian cancer. We need to check and follow up on people with STIC closely.
Detection and Implications
Finding STIC needs careful examination of the fallopian tubes, often during surgery in high-risk people. Finding STIC means big changes in how we manage patients, like more surgery or watching them closely.
When STIC is found, we must talk about all the options for managing it. This includes surgery to prevent cancer, medicine to stop cancer, or watching closely for cancer to develop.
Anatomy and Function of the Fallopian Tubes
It’s important to know about the Fallopian tubes to understand their role in reproduction and how cancer affects them. These tubes, also called oviducts, link the ovaries to the uterus. They play a key part in the female reproductive system.
Normal Structure and Purpose
The Fallopian tubes are about 10-13 cm long. They have four parts: the intramural, isthmic, ampullary, and infundibular sections. The intramural portion goes through the uterine wall. The isthmic portion is narrower and closer to the uterus.
The ampullary portion is wider, making it the best place for fertilization. The infundibular portion is the outermost, opening into the peritoneal cavity near the ovary.
The main job of the Fallopian tubes is to move the egg from the ovary to the uterus. They also help sperm reach the egg for fertilization, usually in the ampulla. The fimbriae, at the end of the tubes near the ovaries, help catch the released egg.
How Cancer Affects Fallopian Tube Function
Fallopian tube cancer can harm how the tubes work. As tumors grow, they can block the tube. This can cause fluid buildup or hydrosalpinx. Cancer can also mess with the environment needed for fertilization, affecting fertility.
- Cancerous growths can physically block the tube, hindering the passage of the egg or sperm.
- The presence of tumors can lead to inflammation and scarring, further complicating the tube’s function.
- In advanced cases, the cancer can spread to surrounding tissues and organs, such as the ovaries and uterus, complicating reproductive health.
Knowing how Fallopian tube cancer affects these tubes is key for diagnosing and treating it. We will look at more about Fallopian tube cancer in the next sections.
Types of Fallopian Tube Cancer
Fallopian tube cancer can be divided into several types. These types are based on the cell of origin and other factors. Knowing these types helps doctors choose the best treatment.
Epithelial Tumors
Epithelial tumors are the most common type of Fallopian tube cancer. They start from the lining of the tubes. These tumors can be serous, mucinous, endometrioid, or clear cell, with serous being the most common.
Serous epithelial tumors are often aggressive. They are linked to high-grade serous carcinoma (HGSC), which has a poor prognosis. Early detection and treatment are key to managing this cancer.
Non-epithelial Tumors
Non-epithelial tumors come from parts of the Fallopian tubes other than the lining. These are less common and include leiomyosarcomas and malignant mixed Müllerian tumors.
These tumors are hard to diagnose and treat. This is because they are rare and have different features.
Metastatic Tumors
Metastatic tumors in the Fallopian tubes are more common than primary cancer. They usually come from other gynecological cancers, like ovarian or endometrial cancer.
It’s important to know if a tumor is primary or metastatic. This information helps with staging and treatment planning.
| Type of Tumor | Origin | Characteristics |
| Epithelial Tumors | Epithelial lining | Most common type, includes serous, mucinous, endometrioid, and clear cell types |
| Non-epithelial Tumors | Non-epithelial components (stroma, germ cells) | Less common, includes leiomyosarcomas and malignant mixed Müllerian tumors |
| Metastatic Tumors | Other cancer sites (e.g., ovary, endometrium) | More common than primary Fallopian tube cancer, requires accurate diagnosis for treatment |
Each type of Fallopian tube cancer has its own characteristics and treatment needs. Accurate diagnosis and classification are key to creating an effective treatment plan.
Risk Factors for Developing Fallopian Tube Cancer
Knowing the risk factors for Fallopian tube cancer is key to early detection and prevention. We’ll look at the main factors that lead to this disease. This includes genetic factors and other significant risks.
Genetic Predisposition
Genetic predisposition is a big factor in Fallopian tube cancer. Some genetic mutations raise a woman’s risk. We’ll dive into the genetic factors that contribute to this disease.
BRCA1 and BRCA2 Mutations
BRCA1 and BRCA2 mutations are known risks for many cancers, including Fallopian tube cancer. Women with these mutations face a higher risk. Women with a family history of breast or ovarian cancer should consider genetic testing.
Research shows that BRCA1 and BRCA2 mutation carriers are at higher risk for breast, ovarian, and Fallopian tube cancer. This risk is so high that removing the Fallopian tubes is often discussed with these patients.
Other Risk Factors
Other factors also play a role in Fallopian tube cancer risk. These include:
- Age: The risk grows with age, more so after 50.
- Reproductive history: Women who have never given birth or have infertility issues may face higher risks.
- Family history: A family history of breast, ovarian, or Fallopian tube cancer increases risk.
Understanding these risk factors helps in creating personalized screening and prevention plans. It’s vital to talk to a healthcare provider about individual risk factors. This way, you can find the best prevention strategy.
Signs and Symptoms of Fallopian Tube Cancer
It’s important to know the signs and symptoms of Fallopian tube cancer early. This can help with early detection and treatment. We will talk about the main signs that might show you have this condition.
Early Warning Signs
Fallopian tube cancer in its early stages can be hard to spot. It often shows vague symptoms. Some early signs include:
- Abdominal pain or discomfort
- Abnormal vaginal bleeding
- Pelvic pain or pressure
- Abnormal vaginal discharge
These symptoms can also be seen in other gynecological issues. So, it’s key to get a detailed medical check-up.
Advanced Stage Symptoms
When Fallopian tube cancer gets worse, symptoms get more serious. Symptoms of advanced stages include:
- Increased abdominal girth due to ascites
- Weight loss
- Fatigue
- Bloating
It’s important to remember that these symptoms can also be from other conditions. Only a doctor can say for sure what’s wrong.
When to Seek Medical Attention
If you’re feeling any of these symptoms, and they don’t go away or get worse, you should see a doctor. You should talk to a healthcare provider if you have:
- Unexplained or persistent abdominal pain
- Abnormal vaginal bleeding or discharge
- A family history of ovarian or breast cancer
Getting diagnosed early can really help with treatment. We urge you to look after your health and get checked if you’re worried about your symptoms.
Diagnosis of Fallopian Tube Cancer
We use a detailed plan to find Fallopian tube cancer. This plan includes many ways to check for it. Finding it right is key for good treatment.
Initial Assessment
The first step is a physical examination. Doctors look at the patient’s health and check for signs of cancer in the Fallopian tubes.
Imaging Studies
Imaging studies are very important. Ultrasound, CT scans, and MRI scans help see the Fallopian tubes. They help doctors find tumors or other problems.
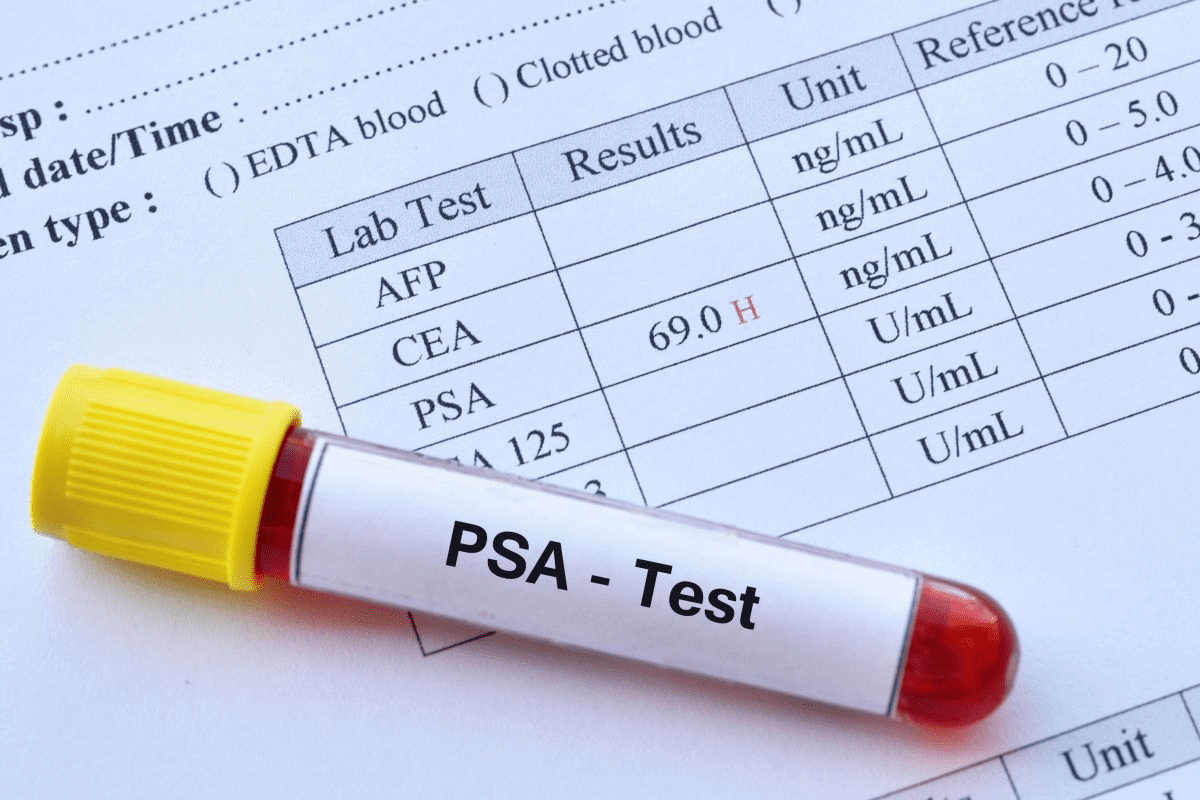
Laboratory Tests
Laboratory tests are also key. These tests include blood tests for tumor markers like CA-125. These markers can show if there’s cancer in the Fallopian tubes.
Surgical Diagnosis
Sometimes, a surgical diagnosis is needed. This means looking at tissue samples taken during surgery. It’s used when other tests aren’t clear.
Diagnostic Challenges
Finding Fallopian tube cancer can be hard. Its symptoms are not always clear and can look like other health issues. So, doctors use many tests together to be sure.
| Diagnostic Method | Description | Role in Diagnosis |
| Physical Examination | Initial assessment of patient’s health | Identifies abnormalities |
| Imaging Studies | Ultrasound, CT, MRI scans | Visualizes tumors or abnormalities |
| Laboratory Tests | Blood tests for tumor markers | Assesses for elevated markers |
| Surgical Diagnosis | Examination of tissue samples | Provides definitive diagnosis |
Staging of Fallopian Tube Cancer
Knowing the stage of Fallopian tube cancer is key to choosing the right treatment. Staging helps doctors see how far the cancer has spread. This information helps decide the best treatment and gives insight into the patient’s future.
FIGO Staging System
The International Federation of Gynecology and Obstetrics (FIGO) staging system is used for Fallopian tube cancer. It divides the disease into stages based on how far the tumor has grown. Here’s how the FIGO system works:
- Stage I: The tumor is only in the Fallopian tubes.
- Stage II: The tumor is in one or both Fallopian tubes and has spread to the pelvic area.
- Stage III: The tumor is in one or both Fallopian tubes and has spread to the peritoneum outside the pelvis and/or to nearby lymph nodes.
- Stage IV: The tumor is in one or both Fallopian tubes and has spread to distant parts of the body.
TNM Classification
The TNM classification is another way to stage Fallopian tube cancer. It looks at the size and spread of the tumor (T), if nearby lymph nodes are involved (N), and if there are distant metastases (M). This system gives a detailed view of the disease’s spread.
Importance of Accurate Staging
Accurate staging is very important. It helps doctors plan the best treatment, which could be surgery, chemotherapy, or both. It also gives a clear idea of what to expect in terms of recovery. Plus, it helps find out if a patient might benefit from new treatments being tested.
In short, staging Fallopian tube cancer is a detailed process. It uses systems like FIGO and TNM to understand the disease’s spread. Getting the staging right is essential for choosing the right treatment and knowing what to expect.
Treatment Options for Fallopian Tube Cancer
Treating fallopian tube cancer involves several steps. These steps depend on the cancer’s stage and type. We will look at the different treatments available. This will help patients and their families make informed choices about their care.
Surgical Interventions
Surgery is a key treatment for fallopian tube cancer. The aim is to remove the tumor and any affected tissue. We usually do a total hysterectomy with bilateral salpingo-oophorectomy. This means removing the uterus, both fallopian tubes, and ovaries.
Key surgical procedures include:
- Debulking surgery to remove as much of the tumor as possible
- Staging surgery to determine the extent of cancer spread
Chemotherapy Protocols
Chemotherapy uses drugs to kill cancer cells. For fallopian tube cancer, it’s often used with surgery. We might give chemotherapy before surgery to shrink the tumor. Or after surgery to kill any remaining cancer cells.
Chemotherapy regimens may include:
- Platinum-based chemotherapy, such as carboplatin or cisplatin
- Combination chemotherapy with multiple drugs
Radiation Therapy
Radiation therapy uses high-energy rays to kill cancer cells. It’s not as common for fallopian tube cancer as for other cancers. But, it might be used in some cases, like when the cancer has spread.
Targeted Therapies
Targeted therapies target cancer cells or the environment around them. For fallopian tube cancer, these therapies are used, mainly for cancers with specific genetic mutations.
Examples of targeted therapies include:
- PARP inhibitors for patients with BRCA1 or BRCA2 mutations
- Angiogenesis inhibitors to prevent the formation of new blood vessels that feed the tumor
We keep an eye on new targeted therapies. We look at how they might help treat fallopian tube cancer.
Clinical Management and Follow-up Care
Managing Fallopian tube cancer means more than just the first treatment. It’s about ongoing care and management. We focus on a full approach to help patients, not just at the start.
Surveillance Protocols
Keeping an eye on patients after treatment is key. This includes:
- Regular visits to healthcare providers
- Scans like ultrasound or CT scans
- Tests to check for tumor markers
These steps help catch any signs of cancer coming back early. This way, we can act fast.
Managing Treatment Side Effects
It’s important to handle treatment side effects well. This improves life quality for patients. This can be:
- Help for physical issues like pain or tiredness
- Support for emotional and mental health, like counseling
- Dealing with long-term issues like swelling or nerve problems
By tackling these side effects, we can make a big difference in patient outcomes and happiness.
Long-term Monitoring
Watching patients over time is critical. It helps catch late treatment effects and any cancer coming back. We suggest regular check-ups and tests as part of ongoing care.
With comprehensive clinical management and follow-up care, we make sure patients get the support they need with Fallopian tube cancer.
Research Advancements and Clinical Trials
Our knowledge of Fallopian tube cancer is growing. This growth leads to better treatments through research and trials. It brings hope to patients and their families.
Emerging Treatment Approaches
New ways to treat Fallopian tube cancer are being explored. These include targeted therapies, immunotherapies, and new surgery methods.
Targeted therapies aim to kill cancer cells without harming healthy tissue. For example, treatments targeting the HER2 protein or the PARP pathway are being studied.
Participation in Clinical Trials
Joining clinical trials is key to improving Fallopian tube cancer treatment. These trials offer new treatments not yet available to everyone.
We urge patients to talk to their doctors about joining a trial. It could give them new treatment options. It also helps us learn more about treating Fallopian tube cancer.
| Clinical Trial Phase | Focus | Potential Benefits |
| Phase I | Safety and dosage | Determining the safety of new treatments |
| Phase II | Effectiveness | Assessing the efficacy of treatments |
| Phase III | Comparison with standard treatments | Comparing new treatments to existing standards |
Future Directions in Treatment
The future of treating Fallopian tube cancer looks bright. Treatments will be more tailored and effective. This is thanks to advances in genetic sequencing and molecular diagnostics.
Also, combining data from trials will help us understand the disease better. This will lead to even better treatment plans.
Conclusion
We’ve looked into Fallopian tube cancer, a rare but serious disease often linked to ovarian cancer. It’s important to know its other names, like Primary Fallopian Tube Carcinoma (PFTC) and Tubal Carcinoma. This helps doctors diagnose and treat it correctly.
Understanding the risks of Fallopian tube cancer is key. Things like genetic risks and BRCA1 and BRCA2 mutations play a big role. Early detection is critical, thanks to imaging, lab tests, and surgery.
Treating Fallopian tube cancer involves surgery, chemotherapy, and targeted treatments. Research and clinical trials are working to make treatments better. By keeping up with new findings, we can help those dealing with this disease.
FAQ
What is Fallopian tube cancer, and what are its other names?
Fallopian tube cancer is a rare cancer that affects the Fallopian tubes. It’s also called primary Fallopian tube carcinoma or tubal carcinoma. This cancer is known as Fallopian tube malignancy.
What is the relationship between Fallopian tube cancer and ovarian cancer?
Fallopian tube cancer and ovarian cancer are closely linked. High-grade serous carcinoma (HGSC) is a common cancer in both areas. Studies show HGSC might start in the Fallopian tubes.
What is Serous Tubal Intraepithelial Carcinoma (STIC), and why is it significant?
STIC is a precursor to HGSC, a cancer that can become aggressive. Finding STIC early is key to stopping more severe cancers.
What are the risk factors for developing Fallopian tube cancer?
Genetic factors, like BRCA1 and BRCA2 mutations, increase the risk of Fallopian tube cancer. Other factors might also play a role.
What are the signs and symptoms of Fallopian tube cancer?
Early signs of Fallopian tube cancer can be vague. Symptoms in later stages include pelvic pain and abnormal bleeding. If you notice these symptoms, see a doctor.
How is Fallopian tube cancer diagnosed?
Doctors use physical exams, imaging, lab tests, and sometimes surgery to diagnose Fallopian tube cancer. These methods help find the cancer accurately.
What are the treatment options for Fallopian tube cancer?
Treatments include surgery, chemotherapy, radiation, and targeted therapies. The right treatment depends on the cancer’s stage and type.
What is the importance of accurate staging in Fallopian tube cancer?
Accurate staging is vital for planning treatment. It uses systems like FIGO and TNM classification. This helps doctors choose the best treatment.
What is the role of clinical management and follow-up care in Fallopian tube cancer?
Good management and follow-up care are key for patients. They include surveillance, managing side effects, and long-term monitoring. This ensures the best outcomes.
Are there any emerging treatment approaches for Fallopian tube cancer?
Yes, new treatments are being researched. Clinical trials offer innovative treatments. They help improve treatment options for the future.