Overactive bladder treatments compared. Discover amazing ways to permanently stop OAB and find a powerful cure for frequent urination. Urinary incontinence is a big problem for the elderly. 15% to 30% of community-dwelling elderly and up to 50% of nursing home residents face it. It makes life hard for those with overactive bladder.
We know finding the right treatment is key. This article will look at ways to handle overactive bladder. We’ll cover lifestyle changes, behavioral therapies, medicines, and even bladder surgery and sling procedure bladder.
Key Takeaways
- Understanding the impact of urinary incontinence on the elderly population.
- Exploring lifestyle modifications and behavioral therapies for managing overactive bladder.
- Discussing the role of medications in urinary incontinence treatment.
- Advanced therapies, including bladder surgery and sling procedure bladder, as possible solutions.
- The importance of having all the information to choose the right treatment.
Understanding Overactive Bladder Symptoms

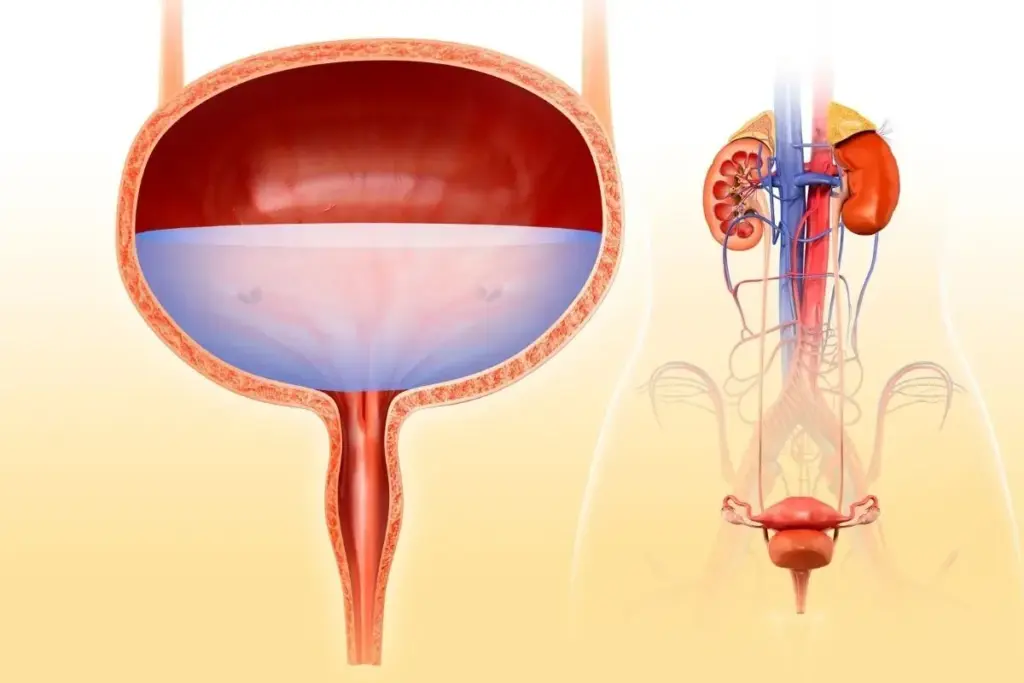
Knowing the symptoms of overactive bladder is key to managing it well. Overactive bladder (OAB) affects millions, causing distress and impacting life quality.
Common Symptoms of Overactive Bladder
The primary symptoms of overactive bladder include urgency, increased frequency of urination, and nocturia. Urgency means a sudden, strong need to urinate, often leading to involuntary urination. Frequency means needing to urinate more than usual, often over eight times in 24 hours. Nocturia is waking up many times at night to urinate, disrupting sleep.
These symptoms can be linked to different types of incontinence. Urge incontinence is when you leak urine suddenly, often with urgency. Stress incontinence is when you leak urine on effort, sneezing, or coughing.
|
Symptom |
Description |
Impact |
|---|---|---|
|
Urgency |
Sudden, intense need to urinate |
Involuntary urination, anxiety |
|
Frequency |
Needing to urinate more than usual |
Disrupted daily activities, discomfort |
|
Nocturia |
Frequent urination at night |
Disrupted sleep patterns, fatigue |
Impact on Daily Life
OAB symptoms can greatly affect daily life. They can cause embarrassment, anxiety, and disrupted sleep patterns. People with OAB may find it hard to do daily activities, interact socially, and enjoy life. The emotional impact of OAB should not be ignored, as it can lead to isolation and depression.
When to Consult a Healthcare Provider
If you have OAB symptoms, seeing a healthcare provider is important. They will help find the cause and suggest treatments. Urge incontinence treatment and stress incontinence treatment options are available.
By understanding OAB symptoms and getting medical help, you can manage your condition. There are many overactive bladder therapies to choose from, including lifestyle changes, medications, and behavioral therapies.
Overview of Treatment Options for Overactive Bladder

There are many ways to treat overactive bladder, from simple lifestyle changes to more complex medical treatments. We will look at these options to help you understand your choices.
Lifestyle Modifications
Making small changes in your daily life can greatly help with overactive bladder. These changes can make a big difference.
- Dietary changes: Avoiding irritants like caffeine and spicy foods can help.
- Fluid management: Monitoring and adjusting fluid intake can alleviate symptoms.
- Pelvic floor exercises: Strengthening the pelvic floor muscles through exercises like Kegels can improve bladder control.
A healthcare professional said, “Making these lifestyle adjustments can be challenging, but they are often the first line of defense against OAB symptoms.”
Medications for Symptom Relief
For many, taking medication is a key part of managing overactive bladder. There are different types of medications that can help.
|
Medication Type |
Function |
Examples |
|---|---|---|
|
Anticholinergics |
Reduce bladder muscle contractions |
Oxybutynin, Tolterodine |
|
Beta-3 Agonists |
Relax bladder muscle |
Mirabegron |
It’s important to work with a healthcare provider to find the best treatment for you. Everyone reacts differently to treatments.
Behavioral Therapies for Managing Overactive Bladder
Managing overactive bladder (OAB) symptoms needs a mix of approaches. Behavioral therapies are key in changing daily habits to help manage OAB. We’ll look at how these techniques can be part of your daily life to ease OAB symptoms.
Bladder Training Techniques
Bladder training helps by slowly increasing the time between bathroom visits. This makes the bladder hold more urine, cutting down on how often you need to go. To start, keep a diary of when you go to the bathroom. Then, slowly increase the time between visits.
- Keep a bladder diary to track voiding patterns.
- Gradually increase the time between trips to the bathroom.
- Practice relaxation techniques to help manage urgency.
By doing these steps, you can make your bladder hold more and reduce OAB symptoms.
Scheduled Voiding
Scheduled voiding helps by setting a regular time for urination. It’s great for those with severe OAB symptoms. To do this, set a regular time to go to the bathroom, like every 2-3 hours.
- Establish a regular voiding schedule, such as every 2-3 hours.
- Stick to the schedule, even if you don’t feel the need to urinate.
- Gradually adjust the schedule as your bladder becomes more consistent.
This method trains your bladder and lowers the chance of accidents.
Pelvic Floor Exercises
Pelvic floor exercises, or Kegels, are important for bladder control. To do Kegels right:
- Identify the correct muscles by stopping the flow of urine mid-stream.
- Contract these muscles for 5-10 seconds and then release.
- Repeat the exercise 10-15 times, several times a day.
Doing Kegels regularly can greatly improve bladder control and lessen OAB symptoms.
|
Behavioral Therapy |
Description |
Benefits |
|---|---|---|
|
Bladder Training |
Gradually increasing intervals between voiding |
Improves bladder capacity, reduces frequency |
|
Scheduled Voiding |
Creating a urination schedule |
Prevents accidents, trains the bladder |
|
Pelvic Floor Exercises |
Strengthening pelvic muscles |
Improves bladder control, reduces OAB symptoms |
By adding these behavioral therapies to your daily life, you can manage OAB symptoms better and live a better life.
Medications: Efficacy and Side Effects
Medications are key in managing Overactive Bladder. They help ease symptoms. There are many options, each with its own benefits and side effects.
Anticholinergics for Overactive Bladder
Anticholinergics are a top choice for OAB. They relax the bladder muscle, helping to control sudden urges. Drugs like oxybutynin and tolterodine are common. But, they can cause dry mouth, constipation, and sometimes affect thinking.
How well anticholinergics work varies. Some people find big relief, while others don’t. It’s important to talk to a doctor to find the right fit.
Beta-3 Agonists
Beta-3 agonists are another option for OAB. They increase bladder capacity, letting you hold more urine. Mirabegron is a well-known one. Side effects might include high blood pressure, infections, and headaches.
These drugs are good for those who can’t take anticholinergics or don’t get enough relief. The choice depends on the patient’s health and other conditions.
Considerations for Long-term Use
Long-term use of OAB meds needs careful thought. Benefits must outweigh risks. Regular check-ups are key to ensure the meds are working and safe.
Changing your lifestyle and trying behavioral therapies can also help. A well-rounded plan often works best for OAB.
Advanced Therapies for Severe Cases
Advanced therapies like Botox injections and neuromodulation therapy offer new ways to manage severe OAB symptoms. These options are for those who haven’t found relief with usual treatments. They can be a big step in their treatment journey.
Botox Injections as a Treatment
Botox injections into the bladder muscle can relax it. This reduces urgency and frequency in Overactive Bladder. This treatment is great for patients who didn’t get better with oral meds. The procedure is done in a clinic and can last several months before needing a repeat.
Neuromodulation Therapy
Neuromodulation therapy uses electrical impulses to control bladder nerves. This helps regulate bladder activity and improves symptoms. There are various types, like sacral nerve stimulation, which is effective for OAB.
Surgical Options
Surgical options are considered when all else fails. Surgical procedures include bladder augmentation or sacral nerve stimulator implantation. These are for severe cases where other treatments didn’t work. It’s important to talk about risks and benefits with a healthcare provider.
Exploring advanced therapies can seem scary. But for many, these treatments have brought relief and improved their life quality. It’s key to talk to a healthcare provider to find the best treatment plan.
The Role of Physical Therapy
Physical therapy, like pelvic floor therapy, is key in managing overactive bladder (OAB) symptoms. It strengthens the muscles around the bladder. This can greatly improve bladder control and overall life quality. We believe physical therapy is vital in treating OAB.
Benefits of Pelvic Floor Therapy
Pelvic floor therapy brings many benefits for OAB sufferers. Improved bladder control is a major plus. Strengthened muscles better support the bladder. It also helps reduce how often and urgently you need to go.
Finding a Specialized Therapist
To get the most from pelvic floor therapy, finding the right therapist is critical. Look for physical therapists with a focus on pelvic floor disorders. Asking for referrals from doctors or professional groups is a good first step.
Dietary Changes to Alleviate Symptoms
Making dietary changes can help with Overactive Bladder symptoms. Knowing which foods and drinks make symptoms worse is key. This way, people can manage their condition better.
Foods to Avoid
Some foods and drinks can irritate the bladder, making OAB symptoms worse. Here are some common ones:
- Caffeine: Found in coffee, tea, and some soft drinks, caffeine can increase bladder activity.
- Spicy Foods: Spices can irritate the bladder, making symptoms worse.
- Citrus Fruits and Juices: Oranges, lemons, and their juices can be bladder irritants.
- Carbonated Drinks: Fizzy drinks can put additional pressure on the bladder.
Avoiding these can help lessen the frequency and urgency of OAB symptoms.
Recommended Hydration Practices
Staying hydrated is key for managing OAB symptoms. But, the type of fluid and when you drink it matter a lot.
Drinking plenty of water is good. But, it’s also smart to:
- Limit fluid intake in the evening to reduce nocturia (waking up at night to urinate).
- Avoid irritants like caffeine and alcohol, which can make symptoms worse.
- Monitor and adjust fluid intake based on individual needs and activity levels.
As one expert notes,
“A balanced approach to fluid management can significantly improve OAB symptoms.”
The Importance of Patient Education
Telling patients about their condition and treatment options is key to managing OAB. When they know what’s going on, they can make better choices. This leads to better health and a better life.
Understanding Your Condition
Knowing about Overactive Bladder (OAB) is the first step to managing it. We think patient education is vital. It helps people understand their condition and the treatments out there.
OAB is a complex issue that affects many. It makes people feel a strong urge to pee, sometimes without control. Knowing why it happens helps both patients and doctors find the right treatment.
Navigating Treatment Options
Finding the right treatment options for OAB can be tough. But with the right help, patients can make smart choices. We help them look at different ways to treat OAB, like changing their diet or trying new therapies.
Understanding each treatment’s good and bad points helps patients pick what’s best for them. For example, lifestyle changes can really help. Sometimes, medications or advanced therapies like Botox are needed too.
In the end, patient education lets people take charge of their health. By working with doctors and staying informed, patients can find the best treatments. This way, they can live a better life despite OAB.
Coping Strategies and Support Resources
For those with OAB, finding the right ways to cope and get support can greatly improve life. It’s not just about medical treatment. It’s also about learning to live with OAB and finding ways to lessen its impact on daily life.
Dealing with OAB can be tough, both physically and emotionally. So, having a strong support system is key. This includes personal coping strategies and external support resources.
Joining Support Groups
Joining a support group is a great way to cope with OAB. These groups let people share their stories, learn from others, and get emotional support. You can find support groups in your community or online, making it easy to access.
Connecting with others who face similar challenges can make you feel less alone. Support groups are also a great place to learn about new treatments and strategies for managing OAB.
Seeking Professional Counseling
Seeking professional counseling is also beneficial. A counselor or therapist can help with the emotional side of OAB, like anxiety or depression. They can also help you create coping strategies that work for you.
Professional counseling is very helpful for those struggling to accept their condition or feeling a lot of distress. It’s a safe place to talk about your feelings and work through challenges with a trained professional’s help.
By using these coping strategies and support resources, people with OAB can live more fulfilling lives. Despite the challenges, they can find ways to manage and improve their situation.
Future Trends in Overactive Bladder Treatments
New treatments for overactive bladder (OAB) are coming. We’re seeing a move towards better and more tailored treatments. This is thanks to ongoing research and new ideas in the field.
Emerging Research and Innovations
New studies are looking into different ways to treat OAB. They’re focusing on new medicines and therapies that target specific causes of OAB. These new options aim to help people with OAB feel better and live better lives.
Potential Breakthroughs in Treatment
The future for OAB treatment is bright. New medicines and therapies are being developed. When these are available, people with OAB will have more choices to manage their condition. This will help them feel better and live better.
FAQ
What is Overactive Bladder (OAB) and how is it diagnosed?
Overactive Bladder is a condition where you suddenly feel a strong urge to pee. You might pee without meaning to. Doctors diagnose it by talking to you, doing a physical check, and sometimes tests like urodynamic studies.
What are the common symptoms of Overactive Bladder?
Symptoms include feeling a strong need to pee, peeing too often, and waking up to pee at night. These can really affect your daily life and how you feel.
What lifestyle modifications can help manage Overactive Bladder symptoms?
Changing your diet, managing how much you drink, losing weight, and avoiding things like caffeine can help. Also, bladder training and pelvic floor exercises are good.
What medications are available for treating Overactive Bladder?
There are medicines like anticholinergics and beta-3 agonists that help relax the bladder muscle. Your doctor will choose the best one for you based on your situation.
What are the possible side effects of Overactive Bladder medications?
Side effects can include dry mouth, constipation, and blurry vision with anticholinergics. Beta-3 agonists might cause headaches or urinary tract infections. Always talk to your doctor about these.
When are advanced therapies considered for Overactive Bladder treatment?
If regular treatments don’t work well, or if symptoms are very bad, doctors might suggest Botox, neuromodulation, or surgery.
What is the role of pelvic floor therapy in managing Overactive Bladder?
Pelvic floor therapy, like Kegels, strengthens the muscles that help control the bladder. A therapist can help you do it right.
How can dietary changes help alleviate Overactive Bladder symptoms?
Avoiding foods that irritate the bladder, like caffeine and spicy foods, and drinking the right amount of water can help.
Why is patient education important in managing Overactive Bladder?
Knowing about your condition and treatment options helps you take care of yourself better. It improves your life quality.
What coping strategies and support resources are available for individuals with Overactive Bladder?
Joining support groups and talking to a counselor can offer emotional support and advice. It helps manage symptoms and improves life quality.
What future trends and innovations are being explored for Overactive Bladder treatments?
New medicines, therapies, and technologies are being researched to better treat OAB. Keeping up with these developments can open up new treatment options.
How does stress incontinence treatment relate to Overactive Bladder?
While treatments for stress incontinence are different, they might help people with both stress and urge incontinence.
What is the urethral sphincter, and how does it relate to urinary incontinence?
The urethral sphincter is a muscle around the urethra that helps control urine flow. If it doesn’t work right, it can lead to incontinence, including stress incontinence.
Are there different types of urinary incontinence, and how are they treated?
Yes, there are types like stress, urge, mixed, and overflow incontinence. Treatment depends on the type and may include lifestyle changes, medicines, therapies, or surgery.