Last Updated on November 25, 2025 by Ugurkan Demir
Atrial fibrillation (AFib) is a common heart rhythm disorder. It can greatly affect a person’s quality of life. A pacemaker can help manage AFib symptoms, like abnormal heart rates. At Liv Hospital, we focus on the latest cardiac care and tailored treatment plans.
Thinking about a pacemaker for atrial fibrillation treatment can be scary. But, this small, battery-powered device can stop the heart from beating too slow. It helps keep the heart rhythm steady. It’s used to control or increase the heartbeat when needed.
Discover 7 key facts about pacemaker for AFib, including its treatment benefits, procedure, and possible side effects.
Key Takeaways
- A pacemaker is used to manage AFib symptoms, like abnormal heart rates.
- It helps stabilize heart rhythm but does not cure AFib.
- Patients may have AFib episodes even with a pacemaker.
- Liv Hospital offers advanced cardiac care and personalized treatment.
- A pacemaker can improve quality of life for AFib patients.
Understanding Atrial Fibrillation and Its Impact on Heart Health
It’s important to know about atrial fibrillation to take care of your heart. Atrial fibrillation, or AFib, is a heart issue where the heart beats irregularly and fast. This happens when the heart’s upper chambers get mixed-up signals, causing irregular beats.
What Happens During Atrial Fibrillation?
In atrial fibrillation, the heart’s rhythm gets messed up. The upper chambers beat too fast and not in sync. This can make the heart beat too fast or irregularly, causing symptoms like palpitations, shortness of breath, and tiredness.
“Atrial fibrillation is not just a simple irregularity in heart rhythm; it’s a serious condition that can lead to significant complications if not managed properly,” says a leading cardiologist. The chaotic electrical activity in the atria can lead to blood clot formation, increasing the risk of stroke and other cardiovascular events.
Common Symptoms and Complications
The symptoms of atrial fibrillation can vary widely among individuals. Some people may experience:
- Heart palpitations or irregular heartbeats
- Shortness of breath or difficulty breathing
- Fatigue or weakness
- Dizziness or lightheadedness
- Chest pain or discomfort
Complications of AFib can be severe and include an increased risk of stroke, heart failure, and other heart-related problems. The condition can also significantly impact quality of life, causing anxiety and reducing physical capacity.
Traditional Treatment Approaches
Traditional treatments for atrial fibrillation aim to control symptoms, prevent complications, and improve quality of life. These may include:
- Medications: To control heart rate, convert AFib to a normal sinus rhythm, or prevent stroke.
- Cardioversion: A procedure that uses electrical shocks to restore a normal heart rhythm.
- Catheter Ablation: A minimally invasive procedure that destroys the abnormal electrical pathways in the heart.
Understanding these traditional treatment approaches is essential for patients to make informed decisions about their care. By working closely with healthcare providers, individuals with AFib can develop a personalized treatment plan that addresses their unique needs and improves their overall heart health.
Key Fact #1: When Is a Pacemaker for AFib Considered?
The choice to get a pacemaker for AFib depends on certain criteria. It looks at the heart’s rhythm and how well other treatments work.
A pacemaker is an option when AFib causes heart rate problems. It’s also considered when other treatments don’t help symptoms enough.
Bradycardia (Slow Heart Rate) Management
Bradycardia is when the heart beats too slowly. This can make you feel dizzy, tired, or faint. In AFib patients, it might happen because of the irregular rhythm or from medication side effects.
A pacemaker can help by keeping the heart rate steady. This can reduce symptoms and improve life quality.
Significant Pauses in Heart Rhythm
Some AFib patients have big pauses in their heart rhythm. This can cause dizziness or even loss of consciousness. A pacemaker can be set to fix these pauses and keep the heart rhythm stable.
- Monitoring heart rhythm for significant pauses
- Pacing the heart to prevent prolonged pauses
- Adjusting pacemaker settings for optimal heart function
Failed Medication Therapy
When medication therapy doesn’t work for AFib, a pacemaker might be an option. This is true if the meds cause bad side effects.
In some cases, a pacemaker can work with other treatments like ablation. This can help manage symptoms better.
Knowing when a pacemaker is considered for AFib helps patients make better choices. It’s about understanding treatment options and making informed decisions.
Key Fact #2: How Pacemakers Function in AFib Patients
Pacemakers are advanced devices that help control heart rhythm in AFib patients. They are key in managing atrial fibrillation, a condition with an irregular and fast heart rate. By sending electrical impulses, pacemakers keep the heart’s rhythm steady, improving patients’ lives.
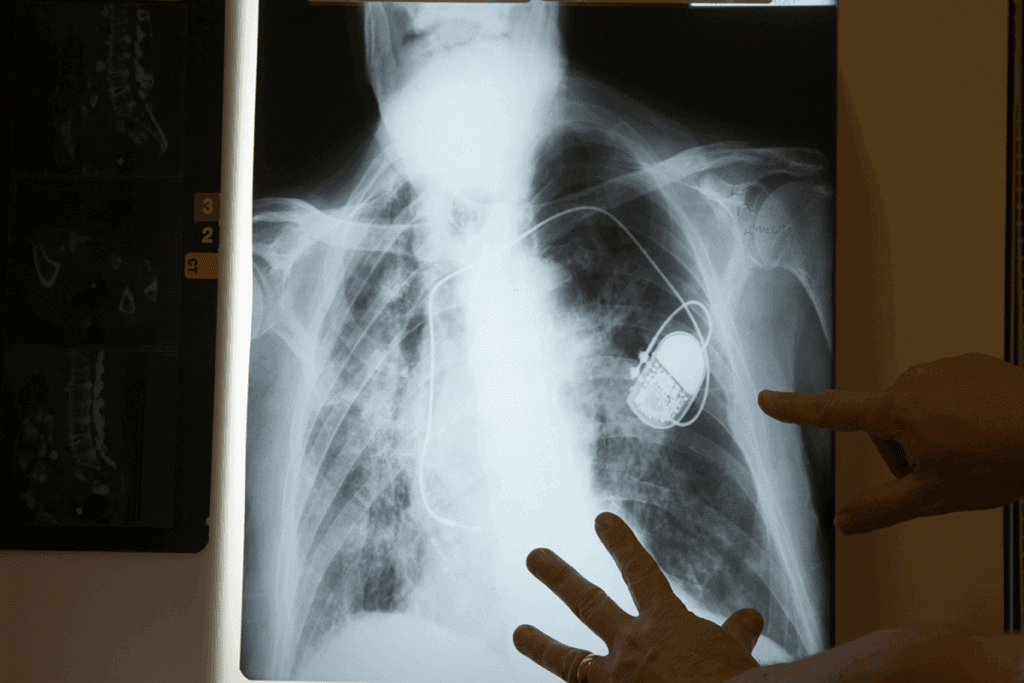
Basic Pacemaker Components and Operation
A pacemaker has two main parts: the pulse generator and the leads. The pulse generator is a small device with the battery and circuitry. It’s placed under the skin, near the collarbone. The leads are thin wires that connect the pulse generator to the heart. They send electrical impulses to keep the heartbeat regular.
When a pacemaker is put in, it’s set to meet the patient’s needs. This involves programming it to detect the heart’s rhythm and send impulses as needed.
Single vs. Dual Chamber Pacemakers
There are two types of pacemakers: single chamber and dual chamber. A single chamber pacemaker has one lead in either the right atrium or ventricle. It paces one chamber of the heart. A dual chamber pacemaker has two leads, one in each chamber. This type can pace both chambers for a more natural rhythm.
For AFib patients, dual chamber pacemakers are better. They can better coordinate the heart’s rhythm between chambers.
Specialized Programming for AFib
Pacemakers for AFib patients need specialized programming. This involves adjusting settings to handle AFib’s irregular rhythms. The programming makes sure the pacemaker sends the right impulses to keep the heart rate stable.
- Adjusting sensitivity to detect atrial fibrillation
- Setting the appropriate pacing mode
- Configuring the device to respond to changes in heart rate
This special programming is vital. It helps the pacemaker work best and gives the patient the most benefit.
Key Fact #3: Pacemaker Combined with AV Node Ablation
For managing AFib with fast heart rates, a mix of treatments is sometimes used. This includes a pacemaker and AV node ablation. This method, called “ablate and pace,” is for those who haven’t gotten better with other treatments.
Understanding the “Ablate and Pace” Strategy
The “ablate and pace” method has two parts. First, the AV node is ablated to stop irregular heart rhythms. Then, a pacemaker is implanted to keep the heart rate steady. This helps control the heart rate and reduce symptoms like palpitations and shortness of breath.
Key components of the “ablate and pace” strategy include:
- Ablation of the AV node to disrupt the irregular electrical signals
- Pacemaker implantation to regulate the heart rate
- Careful monitoring to adjust pacemaker settings as needed
Patient Selection Criteria
Not every AFib patient is right for the “ablate and pace” method. We look at several factors. These include how severe the symptoms are, how well previous treatments worked, and the heart’s overall health. Those with fast heart rates that can’t be controlled by drugs are usually considered.
Key considerations for patient selection include:
- Presence of symptomatic AFib with rapid ventricular response
- Failure of or intolerance to rate-control medications
- Significant impairment in quality of life due to AFib symptoms
Procedural Steps and Recovery
The “ablate and pace” procedure includes both AV node ablation and pacemaker implantation. These steps are done in one session. Advanced imaging helps guide the procedure for safety and success.
After the procedure, patients are watched closely for any immediate issues. Most can go back to normal activities in a few days. But, they should avoid hard exercise for a couple of weeks. Regular check-ups are needed to adjust the pacemaker and track the patient’s progress.
Recovery milestones include:
- Initial monitoring post-procedure
- Gradual return to normal activities
- Follow-up appointments for pacemaker adjustment
Can a Pacemaker Help AFib with Fast Heart Rate?
Many people with atrial fibrillation (AFib) wonder if a pacemaker can help. AFib causes irregular and fast heartbeats. Pacemakers can help manage symptoms of fast heart rates, but they don’t cure AFib.
Rate Control vs. Rhythm Control Approaches
There are two main ways to manage AFib: rate control and rhythm control. Rate control slows the heart rate to normal. Rhythm control tries to get the heart back to a normal rhythm. Pacemakers mainly help with rate control by regulating the heart’s pace.
For those with persistent AFib, rate control is often the preferred method. It can improve symptoms and quality of life. Pacemakers help keep the heart rate steady, preventing it from getting too fast or slow.
Managing Tachycardia Episodes
Tachycardia, or a fast heart rate, is common in AFib. Pacemakers can manage tachycardia by keeping the heart rate consistent. But, their success depends on the heart condition and other health issues.
In some cases, pacemakers are used with other treatments like medications or ablation therapy. The “ablate and pace” strategy, which involves ablating the AV node and implanting a pacemaker, can be effective for some patients.
Limitations in Controlling Rapid Rates
Pacemakers can control heart rate in AFib patients, but they may not always prevent rapid rates. Their effectiveness can be limited by the severity of AFib, other heart conditions, and the patient’s overall health.
A study compared rate control strategies in AFib patients. It found that pacemaker therapy can improve symptoms and quality of life. Here are some key findings:
| Treatment Approach | Symptom Improvement | Quality of Life Improvement |
| Pacemaker Therapy | 70% | 60% |
| Medication Alone | 50% | 40% |
| Ablation and Pacemaker | 80% | 75% |
The table shows that pacemaker therapy, and ablation together, can greatly benefit AFib patients with fast heart rates.
In conclusion, pacemakers can help manage AFib with fast heart rates. But, their success depends on many factors, including the heart condition and overall health. Understanding pacemakers’ role in managing AFib can help patients and doctors make better treatment choices.
Key Fact #4: Advanced Pacemaker Technologies for AFib Management
Advanced pacemaker technologies have changed how we manage atrial fibrillation (AFib). They bring new hope to people all over the world. These advancements have greatly improved life for those with AFib.
Atrial Overdrive Pacing
Atrial overdrive pacing is a feature in advanced pacemakers. It helps manage AFib by pacing the atrium at a rate slightly higher than the patient’s natural heart rate. This method can reduce AFib episodes by stopping the heart from beating too slowly or irregularly.
This pacing keeps the heart rhythm consistent. It helps reduce symptoms like palpitations and shortness of breath. It’s very helpful for those who have AFib often.
Dual-Site Pacing Techniques
Dual-site pacing involves pacing the heart at two different locations. This improves the coordination of heartbeats. It’s very effective for patients with AFib, helping to keep the heart rhythm synchronized.
By pacing both the right atrium and the coronary sinus, dual-site pacing reduces AFib episodes. It also improves heart function. This approach is customized for each patient’s needs and heart anatomy.
Algorithm-Based Rate Adjustments
Modern pacemakers use sophisticated algorithms. These adjust the pacing rate based on the patient’s activity level and other physiological parameters. This ensures the heart rate is right for the patient’s current state, whether resting or exercising.
These adjustments make pacemaker therapy more effective. They provide a natural heart rate response to activity and stress. This is very beneficial for AFib patients, helping manage symptoms and improve exercise tolerance.
In conclusion, advanced pacemaker technologies are key in managing AFib. Features like atrial overdrive pacing, dual-site pacing, and algorithm-based rate adjustments are very helpful. They offer valuable tools for treating AFib, improving symptoms and quality of life for patients and healthcare providers alike.
Key Fact #5: Benefits of Pacemaker for Atrial Fibrillation Treatment
Pacemakers help a lot with AFib. They make life better by fixing heart rhythm problems. This can lessen symptoms and maybe cut down on medication needs.
Symptom Reduction and Quality of Life Improvements
Pacemakers really help with AFib symptoms. Symptoms like palpitations, shortness of breath, and fatigue get better. This makes it easier to do daily things.
With fewer AFib episodes, life gets better. People feel more energetic. They can do things they love without worrying about AFib.
Heart Rate Stabilization
Pacemakers are key in keeping heart rates steady in AFib patients. They make sure the heart beats at a normal pace. This stops rapid heart rates that AFib can cause.
- Regulating heart rhythm to prevent extreme variations
- Improving cardiac output and overall heart function
- Reducing the risk of complications related to irregular heartbeats
Reduced Medication Dependence
Pacemakers might mean less need for AFib meds. They help keep heart rates steady and cut down on AFib episodes. This means patients need fewer medications.
This is good for those who don’t like side effects or have trouble with many meds. But, always talk to a doctor before changing meds.
Pacemakers offer big benefits for AFib patients. They improve life quality and heart health. It’s important to talk to a doctor to see if a pacemaker is right for you.
Key Fact #6: Limitations of Pacemakers in AFib
Pacemakers can help manage AFib symptoms, but they have limits. We’ll look into these to help patients know what to expect.
Can You Stil Have Atrial Fibrillation with a Pacemaker?
Yes, having a pacemaker doesn’t mean you won’t have AFib episodes. Pacemakers manage symptoms and regulate heart rhythm, but they don’t cure AFib. It’s important to keep monitoring and managing the condition.
Will a Pacemaker Fix AFib?
A pacemaker can ease some AFib symptoms by keeping the heart rate steady. But, it doesn’t fix the root cause of atrial fibrillation. So, it’s key to have clear expectations about pacemaker therapy’s benefits and limits.
Managing Expectations About Treatment Outcomes
It’s vital to manage expectations when thinking about a pacemaker for AFib treatment. Talk to your healthcare provider about:
- The possible benefits of pacemaker therapy for your condition
- The possible limits and risks of the treatment
- Strategies for ongoing AFib management
Knowing what pacemakers can and can’t do helps patients make better choices. They can then have more realistic hopes for treatment outcomes.
Key Fact #7: Risks and Complications of Pacemaker Implantation
Pacemaker implantation for AFib comes with risks and complications. Pacemakers help manage atrial fibrillation. But, the implantation process has its own set of challenges.
Surgical Risks and Infection
The surgery to implant a pacemaker carries risks. These include infection, bleeding, and damage to nearby tissue or blood vessels. Infections are serious and may need the device removed and antibiotics.
To lower these risks, the surgery is done under clean conditions. Antibiotics are used to prevent infection.
Device Malfunction and Lead Issues
There are risks of pacemaker malfunction or lead problems. Lead failure can happen due to breakage or insulation issues. This might need more surgeries for repair.
Even with new technology, these issues are a concern. They affect how well pacemakers work for patients.
Long-Term Considerations
Patients with pacemakers face long-term needs. They may need battery replacements every 5 to 15 years. This depends on the device and its settings.
They might also need device upgrades or adjustments. This ensures the device works well and meets the patient’s changing needs.
Pros and Cons of Pacemaker for AFib
Thinking about a pacemaker for AFib means looking at both the good and bad sides. A pacemaker can help manage AFib symptoms. But, it’s not perfect and can have its own set of problems.
Advantages in Specific Patient Populations
For some, pacemakers are a big help with AFib. Those with slow heart rates or heart rhythm pauses can really benefit. Also, people who haven’t gotten better with medicine might find a pacemaker helps.
New pacemaker techs like atrial overdrive pacing and dual-site pacing look promising. They might cut down on AFib episodes for some patients.
Disadvantages and Limitations
Even though pacemakers work well, they’re not without their downsides. They don’t cure AFib; they just manage some symptoms. So, patients might keep having AFib episodes.
There’s also the need for regular check-ups and maybe even battery replacements. Plus, there’s a chance of problems during or after the implant, like infection or device failure.
Weighing Benefits Against Risks
Deciding on a pacemaker for AFib needs careful thought. Patients must think about their health, how bad their AFib symptoms are, and what treatments have worked before.
Talking openly with doctors about the good and bad of pacemakers is key. This way, patients can see if the benefits are worth the risks for them.
In the end, choosing a pacemaker should be a well-informed decision. It’s about knowing the ups and downs and what’s best for each person’s situation.
Living with a Pacemaker and AFib
Living with a pacemaker for atrial fibrillation means making lifestyle changes and staying vigilant about your health. It’s important to know the precautions and monitoring needed to manage AFib safely and effectively.
Activity Restrictions and Precautions
After getting a pacemaker, you’ll need to avoid certain activities to prevent problems. You should not lift heavy things, bend, or do strenuous activities that could harm the pacemaker or its leads. Most people can go back to normal activities in a few weeks, but always listen to your doctor’s advice.
- Avoid contact sports or activities that may cause a direct blow to the pacemaker site.
- Be cautious when bending or stretching to avoid putting pressure on the pacemaker pocket.
- Gradually increase exercise levels, starting with low-intensity activities like walking.
Regular Monitoring and Follow-up Care
Regular checks are key to make sure your pacemaker is working right and to make any needed changes. Follow-up appointments typically involve checking the device’s battery life, lead integrity, and programming. You might also need to have ECGs or other tests to check your heart rhythm and health.
- Schedule regular follow-up appointments with your cardiologist or electrophysiologist.
- Keep a record of your device checks and any changes to your medication or symptoms.
- Be aware of your body’s response to the pacemaker and report any unusual symptoms or concerns.
Electromagnetic Interference Concerns
One big worry for people with pacemakers is electromagnetic interference (EMI). Certain devices or environments can potentially disrupt pacemaker function, but most modern pacemakers are made to handle common EMI sources well.
- Avoid close proximity to strong magnetic fields, such as those found in MRI machines or certain industrial equipment.
- Be cautious when using devices like cell phones, headphones, or other personal electronics near the pacemaker site.
- Inform your healthcare provider about any concerns or exposure to possible EMI sources.
By following these guidelines, people with a pacemaker for AFib can reduce risks and get the most out of their treatment. This can lead to a better quality of life.
Conclusion: Making Informed Decisions About AFib Treatment
It’s key to make smart choices about treating AFib. Knowing about different treatments, like pacemakers, helps AFib patients make good decisions. This is important for managing the condition well.
A pacemaker can be a good choice for some AFib patients. It’s helpful for those with slow heart rates or pauses in rhythm. Knowing the pros and cons of pacemakers helps patients choose the best treatment for them.
Managing AFib well means understanding all treatment options. By looking at how pacemakers help with AFib, patients can work with their doctors. Together, they can create a treatment plan that fits the patient’s needs.
Being informed about AFib treatment lets patients take charge of their health. This leads to a better life and better heart health.
FAQ
Will I stillexperience AFib episodes with a pacemaker?
Yes, you might have AFib episodes even with a pacemaker. Pacemakers can manage symptoms but can’t stop all AFib episodes.
Can a pacemaker help with fast heart rate due to AFib?
A pacemaker can manage fast heart rates from AFib. But how well it works depends on your heart condition and other health issues.
What are the risks associated with pacemaker implantation for AFib?
Risks include surgery problems, infection, device failure, and lead issues. It’s key to talk about these risks with a doctor.
How does a pacemaker work in managing AFib?
A pacemaker sends electrical impulses to the heart. This helps regulate its rhythm. It reduces symptoms and improves life quality for AFib patients.
Are there different types of pacemakers for AFib?
Yes, there are single and dual chamber pacemakers. The right one depends on your heart condition and needs.
Can I stillexperience AFib with a pacemaker?
Yes, having a pacemaker doesn’t mean you won’t have AFib episodes. But it can help manage symptoms and control heart rate.
What lifestyle adjustments are needed with a pacemaker for AFib?
You should know about activity limits, the need for regular checks, and concerns about electromagnetic interference.
Will a pacemaker fix AFib?
A pacemaker is not a cure for AFib. It’s a treatment to manage symptoms and improve life quality.
Can a pacemaker be used in conjunction with other AFib treatments?
Yes, pacemakers can be used with other treatments like AV node ablation. This can manage AFib symptoms well.
How do advanced pacemaker technologies help in AFib management?
Advanced features like atrial overdrive pacing and algorithm-based rate adjustments can reduce AFib symptoms. They improve life quality.
What are the benefits of pacemaker treatment for AFib?
Benefits include reduced symptoms, better life quality, stable heart rate, and possibly less need for medication.
Are there any long-term considerations for pacemaker implantation?
Yes, you’ll need regular follow-up care, possible battery replacement, and watch for lead issues over time.
References
- Kreimer, F., et al. (2024). Pacemaker-induced atrial fibrillation reconsidered: mechanisms, associations and prevention. [Article].https://www.ncbi.nlm.nih.gov/articles/PMC11217490/
- Parkkari, E., et al. (2023). The incidence of atrial fibrillation, new oral anticoagulation, and outcomes in patients with dual-chamber pacemakers. [Article]. https://www.sciencedirect.com/science/article/pii/S2352906723001380