Last Updated on November 25, 2025 by Ugurkan Demir

Atrial fibrillation (AFib) is a common heart rhythm disorder. It can lead to serious complications if not managed well. For patients with bradycardia, or slow heart rate, due to AFib or its treatment, a pacemaker might help. At Liv Hospital, we focus on patient care. We help patients find the best ways to manage AFib and improve their life quality.
Pacemakers are not a cure for AFib but can be effective for some patients. We will look into how pacemakers can help manage AFib. This can improve the life quality of patients.
Explore how a pacemaker for atrial fib works, its effectiveness, and when doctors recommend it for AFib patients.
It’s key to understand AFib to find good treatments. Atrial fibrillation makes the heart beat irregularly and fast. This can cause many health problems.
In AFib, the heart’s upper chambers don’t beat right. They don’t pump blood well into the ventricles. This can cause blood clots, leading to stroke or serious issues.
The heart’s rhythm is off because of bad electrical signals.
AFib symptoms include heart palpitations, shortness of breath, and dizziness. Some people don’t show symptoms, making it hard to diagnose. Complications can be stroke, heart failure, and other heart problems.
Traditional treatments include medicines, lifestyle changes, and procedures like electrical cardioversion or catheter ablation. Rate control and rhythm control are main strategies. Rate control slows the heart rate with medicines. Rhythm control tries to fix the heart rhythm.
AFib pacemaker therapies mainly control heart rate. Knowing the condition helps doctors create treatment plans. These plans might include pacemaker therapy.
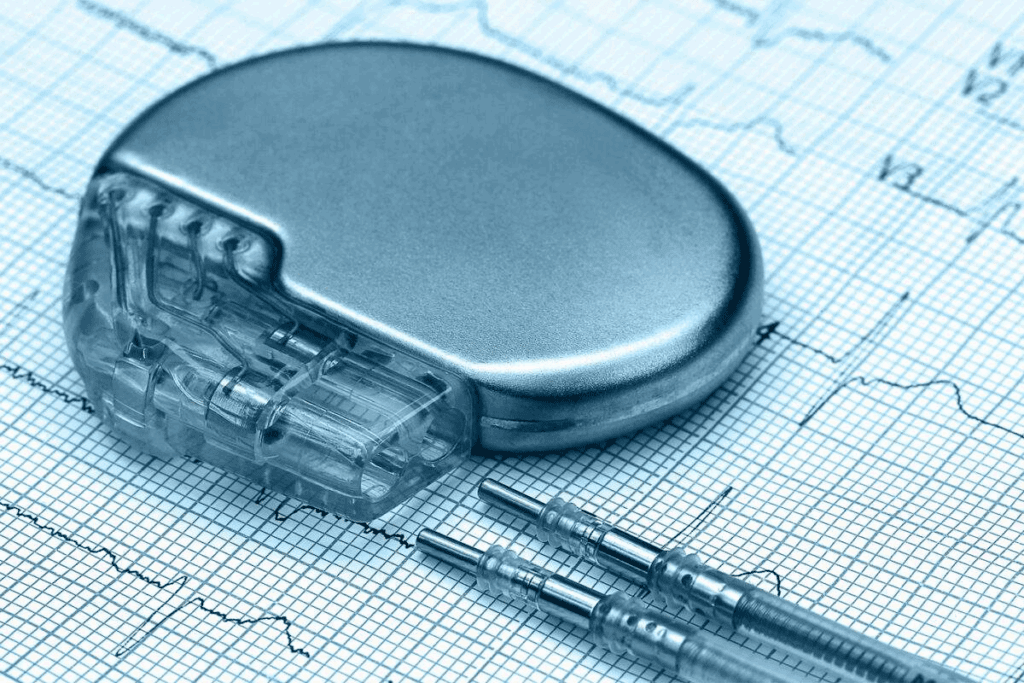
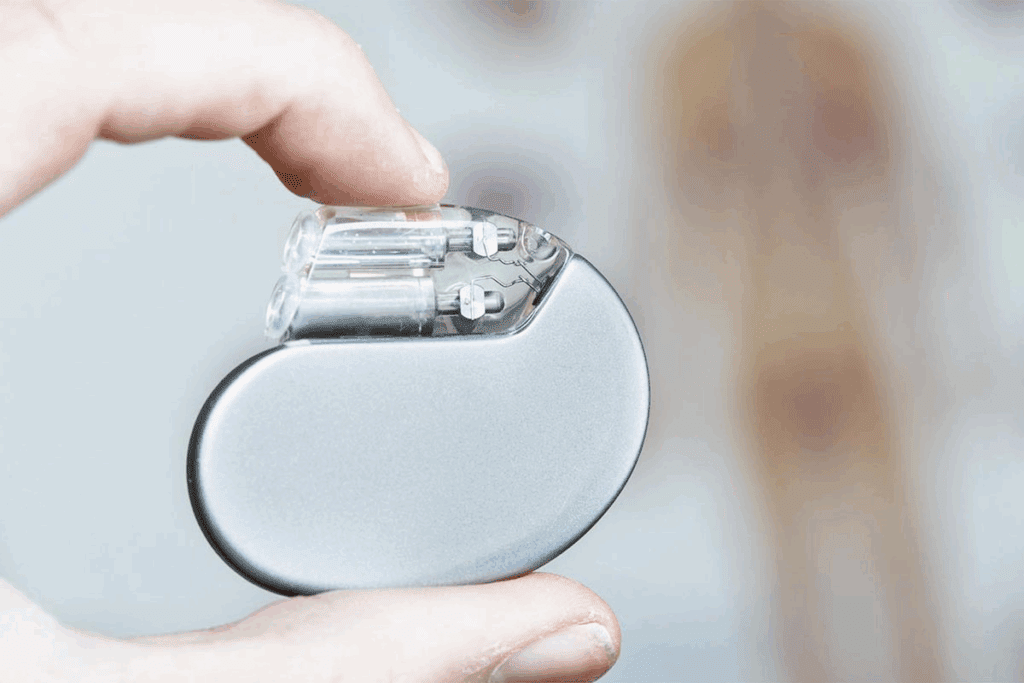
Pacemakers are key in treating heart rhythm disorders like atrial fibrillation. They help control the heartbeat by sending electrical impulses to the heart muscle.
A pacemaker is a small device put under the skin, near the collarbone. It has two main parts: the pulse generator and the leads. The pulse generator is a small metal box with the electronic circuitry and battery. The leads are insulated wires that connect the pulse generator to the heart.
We use pacemakers to treat irregular heartbeats. They ensure the heart beats at a consistent rate. The device checks the heart’s activity and sends electrical impulses when needed to keep a normal heart rate.
There are several types of pacemakers, each for different heart conditions.
| Type of Pacemaker | Description | Primary Use |
| Traditional Pacemaker | Features leads connecting the pulse generator to the heart | Treating bradycardia and other heart rhythm disorders |
| Leadless Pacemaker | Small device implanted directly into the heart | Minimally invasive treatment for certain heart conditions |
| Biventricular Pacemaker | Used for cardiac resynchronization therapy | Treating heart failure by synchronizing ventricular contractions |
The pacemaker implantation procedure is done under local anesthesia. A small incision is made near the collarbone to insert the pulse generator and guide the leads into the heart through a vein.
The procedure is quick, and most patients can go home the same day. After the implant, we monitor the device’s function and ensure the incision heals properly.
Doctors decide on a pacemaker for atrial fibrillation based on several factors. These include bradycardia or the need for AV node ablation. A pacemaker is considered when AFib causes significant symptoms or complications that harm a patient’s quality of life.
Atrial fibrillation can cause irregular heartbeats, sometimes leading to bradycardia, or a slow heart rate. In such cases, a pacemaker helps regulate the heartbeat. This ensures the heart beats fast enough to meet the body’s needs.
AV node ablation disrupts the heart’s abnormal electrical pathway causing AFib. After this procedure, patients often need a pacemaker. This is because the AV node, which regulates heartbeats, is no longer working properly.
Some medications for AFib can cause bradycardia as a side effect. In these cases, a pacemaker is needed to counteract the slow heart rate. This allows patients to keep their treatment without heart rate issues.
Tachy-brady syndrome is a condition where the heart alternates between fast and slow rates. For AFib patients with this syndrome, a pacemaker is very helpful. It manages both the fast and slow heart rate episodes.
In summary, a pacemaker is considered for AFib patients under specific conditions. These include bradycardia, after AV node ablation, when medications cause slow heart rates, or in tachy-brady syndrome. Understanding these conditions helps healthcare providers choose the best treatment for each patient.
Pacemakers are key in managing Atrial Fibrillation (AFib) symptoms. They help patients feel more in control of their condition. These devices regulate heartbeats and stop irregular rhythms, easing AFib symptoms and improving health outcomes.
Pacemakers control the heart rate during AFib episodes. The heart might beat too fast or irregularly. A pacemaker keeps the heart rate normal, reducing symptoms like palpitations and shortness of breath.
With a steady heart rate, pacemakers boost heart efficiency. This means better blood pumping and overall heart health. It also lowers the risk of AFib complications.
AFib can cause heart pauses, leading to dizziness or fainting. Pacemakers detect these pauses and keep the heartbeat steady. This is key for those with slow heart rates and AFib.
By stopping dangerous pauses, pacemakers ensure a steady rhythm. This reduces the risk of falls and other accidents caused by dizziness or loss of consciousness.
The main goal of pacemaker therapy for AFib is to enhance quality of life. Pacemakers control symptoms and maintain a normal heart rhythm. This lets people do daily activities more easily and confidently.
Modern pacemakers also offer remote monitoring and adjustments. This means doctors can tweak settings without frequent visits. It boosts patient convenience and comfort.
The “pace and ablate” method combines a pacemaker with AV node ablation. It’s a good treatment for some AFib patients.
AV node ablation destroys the AV node, a small group of cells that control the heartbeat. It stops the abnormal electrical signals that cause AFib. The procedure uses a catheter guided through a vein to the heart.
We use radiofrequency energy to destroy the AV node during the procedure. This might seem odd, but it helps control the heart rate by blocking the bad electrical pathway.
Key aspects of AV node ablation include:
AV node ablation alone can make the heart rate too slow. To fix this, we implant a pacemaker. The pacemaker keeps the heart rate normal, even after the AV node is destroyed.
This combo helps manage AFib symptoms in patients who didn’t respond to other treatments. It controls the heart rate better and improves the patient’s life quality.
Research shows the “pace and ablate” strategy works well for AFib. Patients often see less symptoms like palpitations, shortness of breath, and fatigue.
This success comes from combining AV node ablation with pacemaker therapy. It controls the heart rate and prevents dangerous pauses, boosting the patient’s well-being.
Benefits of the “pace and ablate” strategy include:
Pacemakers are a key treatment for AFib, backed by lots of clinical evidence. We’ll look at the evidence supporting pacemakers for AFib. This includes success rates, comparisons with other treatments, and what affects outcomes.
Many studies have checked how well pacemakers work for AFib symptoms. Success rates change based on who gets the pacemaker, the type of pacemaker, and other heart issues.
A study in the Journal of the American College of Cardiology found big improvements in patients with AFib and slow heart rate. Over 80% of them saw better symptoms.
| Study | Success Rate | Patient Group |
| Journal of the American College of Cardiology | 80% | AFib with Bradycardia |
| Circulation: Arrhythmia and Electrophysiology | 75% | AFib with Tachy-Brady Syndrome |
| European Heart Journal | 85% | AFib Post AV Node Ablation |
It’s important to compare pacemakers with other AFib treatments. We need to think about the patient’s specific situation and type of AFib.
In patients with AFib and slow heart rate, pacemakers work better than just medicine. They help control symptoms better.
The success of pacemakers for AFib depends on several things. These include if the patient has slow heart rate, their overall heart health, and how they’ve done with other treatments.
Key factors include:
New pacemaker technologies have made things better for AFib patients. These include leadless pacemakers and devices that can pace from multiple points.
These new technologies could make pacemaker therapy even more effective for AFib.
Many patients wonder if a pacemaker means they won’t have atrial fibrillation (AFib) anymore. The answer is no, having a pacemaker doesn’t mean you won’t have AFib episodes. We need to understand how pacemakers help manage AFib and what patients can expect.
Pacemakers are not a cure for atrial fibrillation. They are tools to manage symptoms and improve heart function. AFib is a complex condition with abnormal heart rhythms. Pacemakers ensure the heart has a proper rhythm when it’s too slow or too fast.
Pacemakers can help alleviate symptoms like dizziness, shortness of breath, and fatigue by keeping the heart rate adequate. But they don’t prevent or eliminate AFib episodes.
Managing expectations is key for patients thinking about a pacemaker for AFib. A pacemaker can greatly improve quality of life but isn’t a standalone solution for AFib. We must work closely with healthcare providers to understand how a pacemaker fits into the overall treatment plan.
Realistic expectations help patients cope better with their condition. A pacemaker can manage symptoms, but it may not solve all AFib-related issues. Patients should be ready to continue managing their condition with lifestyle changes and possibly other treatments.
Modern pacemakers have advanced features for monitoring AFib episodes. These devices track the frequency and duration of AFib episodes, giving valuable data for healthcare providers to adjust treatment plans.
Monitoring capabilities of modern pacemakers help manage AFib more precisely. By understanding AFib episode patterns and characteristics, healthcare providers can make better decisions about medication, lifestyle changes, and other interventions.
By using pacemaker data, we can improve patient care and outcomes for those living with AFib.
Having a pacemaker for AFib is a big step in managing your condition. It’s a significant advancement, but there are important things to know. These help ensure you get the best from your treatment.
After getting a pacemaker, you’ll need to make some changes. Avoid heavy lifting or bending on the arm where the pacemaker is for a few weeks. This helps prevent discomfort or complications.
Also, be careful around strong magnetic fields. These can come from MRI machines or certain industrial equipment. They might affect how your pacemaker works.
While some activities might need to change, most people can get back to their usual routines quickly. It’s smart to keep a list of your medications and device info handy. This is useful in case of emergencies.
Regular check-ups are key to making sure your pacemaker works right. Your healthcare provider will check the device’s settings and battery life during these visits.
Many pacemakers can be monitored remotely. This lets doctors check on the device without needing to see you in person. It’s great for catching any issues early.
Key aspects of follow-up care include:
Pacemakers are made to last a long time, but they’re not permanent. The battery life varies based on the device, its settings, and your heart condition. On average, a pacemaker battery lasts 5 to 15 years.
When the battery is almost gone, you’ll need a new pacemaker. This replacement is usually less invasive than the first implantation.
For many with AFib, a pacemaker is just part of their treatment. They might also need medications, lifestyle changes, and other treatments to manage their condition well.
It’s important for patients to work closely with their healthcare providers. This ensures all treatments work together well. It also helps manage any interactions between the pacemaker and other treatments.
By understanding life with a pacemaker, people with AFib can better manage their treatment. This improves their quality of life.
Pacemakers can be a great help for people with Atrial Fibrillation. It’s important to know the good and bad sides of pacemaker therapy for AFib. This helps patients decide if a pacemaker is right for them.
Pacemakers can help control AFib symptoms and improve life quality. They can also prevent serious problems. But, it’s key to remember that pacemakers don’t cure AFib. Patients need to understand both the benefits and limits to make the best choice for their treatment.
Looking at the research and talking to doctors can help patients make good decisions about pacemakers. This teamwork lets patients play a big part in managing their AFib. It leads to better health and quality of life.
No, a pacemaker can’t cure atrial fibrillation. But, it can help manage symptoms. This is true for patients with slow heart rates.
Yes, you might have atrial fibrillation symptoms with a pacemaker. The device manages heart rate. But, it doesn’t get rid of the arrhythmia.
A pacemaker can control heart rate and prevent dangerous pauses. It improves life quality for atrial fibrillation patients. This is true for those with slow heart rates or after AV node ablation.
Yes, some pacemakers can manage fast heart rates from atrial fibrillation. The “pace and ablate” strategy is very effective. It combines AV node ablation with pacemaker implantation.
Modern pacemakers can track atrial fibrillation episodes. This lets healthcare providers manage the condition better. They can adjust treatment plans as needed.
Patients with a pacemaker for atrial fibrillation need to make lifestyle changes. They should avoid strong magnetic fields and tell healthcare providers about their pacemaker. Regular follow-up appointments are also important.
Yes, pacemaker therapy can be used with other treatments for atrial fibrillation. The “pace and ablate” strategy is an example. It combines pacemaker implantation with AV node ablation.
Pacemaker longevity depends on several factors. These include the device type, settings, and patient condition. Pacemakers can last from 5 to 15 years or more before needing replacement.
Pacemaker implantation carries some risks, like infection or device malfunction. But, these are rare. Healthcare providers take steps to minimize risks.
Pacemakers can be very effective for managing atrial fibrillation symptoms. They are best used in the right patient population. Clinical evidence supports their use for rate control and improving quality of life.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!