Last Updated on November 4, 2025 by mcelik

Nearly 80% of patients who have spinal fusion surgery face a lot of pain after the operation. This makes it very important to manage pain well for a good recovery. Find out what pain during scoliosis surgery feels like and how anesthesia and meds help manage it.
Dealing with scoliosis surgery can seem scary, but knowing what to expect can help. Learning about the pain levels and how to manage it can make recovery easier.
Key Takeaways
- Effective pain management is key after scoliosis surgery.
- Spinal fusion surgery can lead to a lot of pain after.
- Knowing your pain management options can help you recover better.
- Talking to your doctor about pain is important.
- A good pain management plan can make surgery better.
Understanding Scoliosis and Surgical Intervention
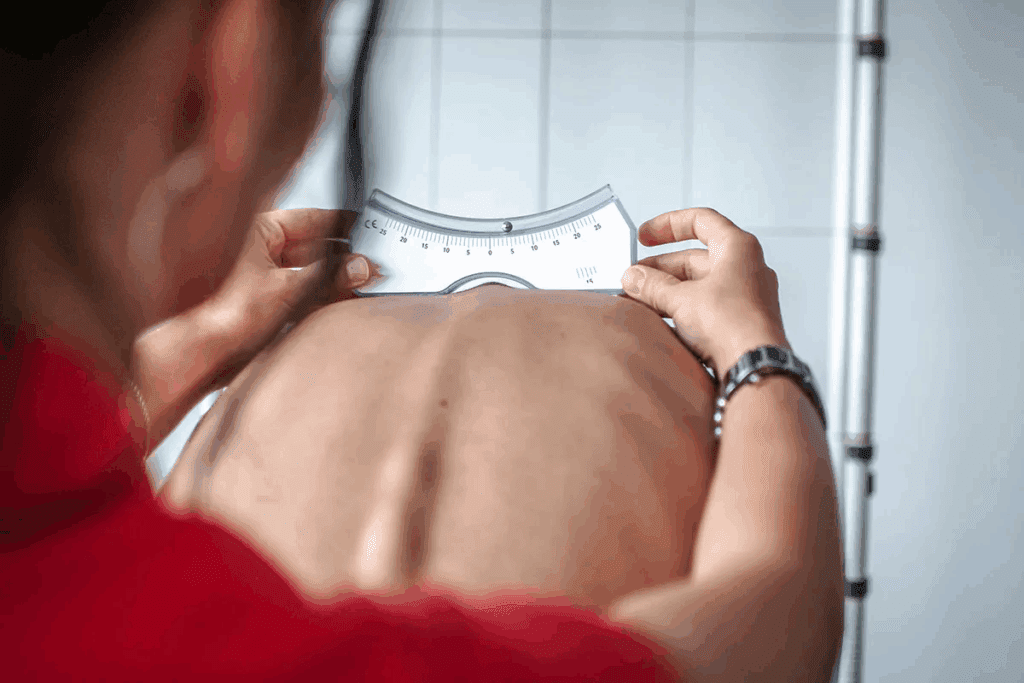
Learning about scoliosis surgery starts with knowing what scoliosis is and when surgery is needed. Scoliosis is a condition where the spine curves abnormally. The curve can be mild or severe, affecting people differently.
We will dive into the details of scoliosis, including its types and when surgery is needed. Knowing this helps patients make the right treatment choices.
What is Scoliosis and When is Surgery Recommended?
Scoliosis often shows up in late childhood or early teens, but it can also happen in adults. It can be caused by genetics, neuromuscular conditions, or spine degeneration. Surgery is considered when the curve is very large (over 45-50 degrees) and is likely to get worse.
Choosing surgery depends on the patient’s health, the curve’s size, and the surgery’s risks and benefits. We’ll look at what makes surgery necessary.
Common Types of Scoliosis Requiring Surgical Correction
There are many types of scoliosis, each with its own cause and features. The most common ones needing surgery are:
- Adolescent Idiopathic Scoliosis (AIS): The most common form, occurring in late childhood or early adolescence without a known cause.
- Congenital Scoliosis: Present at birth due to abnormal spinal development.
- Neuromuscular Scoliosis: Associated with neurological or muscular diseases, such as cerebral palsy or muscular dystrophy.
- Degenerative Scoliosis: Occurring in adults due to degenerative changes in the spine.
Knowing the type of scoliosis is key to choosing the right treatment.
Goals of Scoliosis Surgery
The main goals of scoliosis surgery are to fix the spine’s shape, stabilize it, and stop it from curving more. Surgery techniques have improved to make recovery faster and reduce risks.
| Goal | Description |
| Correct Deformity | Reduce the abnormal curvature of the spine to improve appearance and reduce discomfort. |
| Stabilize Spine | Use instrumentation like rods and screws to hold the spine in place while it heals. |
| Prevent Progression | Prevent the curvature from worsening over time, reducing the risk of future complications. |
Understanding the goals and types of scoliosis surgery helps patients make informed decisions about their care.

Types of Scoliosis Surgical Procedures
Scoliosis surgery offers different options to fix spinal curves. The right surgery depends on the scoliosis’s severity, the patient’s health, and the surgeon’s opinion.
Posterior Spinal Fusion
Posterior spinal fusion is a common scoliosis surgery. It involves an incision in the back to reach the spine. The surgeon uses rods, screws, and other tools to straighten the spine and fuse the vertebrae.
Benefits: This method is good for big curvatures. It makes the spine very stable.
Anterior Spinal Fusion
Anterior spinal fusion goes through the chest or abdomen to fix the spine. It works well for some types of scoliosis.
Advantages: This surgery might cause less muscle damage. It could also lead to a quicker recovery than posterior fusion.
Combined Anterior-Posterior Procedures
Sometimes, surgeons use a combined approach. This means they operate on the front and back of the spine at the same time or in two steps.
Considerations: This method is for very complex or severe scoliosis cases.
Minimally Invasive Options
Minimally invasive scoliosis surgery uses small incisions and might cause less damage. It’s not for everyone but can lead to a faster recovery.
| Surgical Procedure | Description | Benefits |
| Posterior Spinal Fusion | Corrects curvature through the back | Strong stabilization |
| Anterior Spinal Fusion | Approaches spine from the front | Less muscle damage, faster recovery |
| Combined Anterior-Posterior | Operates on both front and back | Comprehensive correction for complex cases |
| Minimally Invasive Surgery | Smaller incisions, less tissue damage | Quicker recovery |
Pre-Surgical Considerations and Preparation
Getting ready for scoliosis surgery is more than just the surgery. It’s about thorough preparation beforehand. Knowing what to do before surgery can really help your outcome and recovery.
Physical Preparation for Surgery
Being physically fit is key before surgery. Patients should:
- Do exercises that boost overall health, like walking or swimming.
- Eat a healthy diet full of nutrients to aid in recovery.
- Stay away from smoking and limit alcohol to lower surgery risks.
Getting in shape can make recovery faster and cut down on complications.
Mental and Emotional Readiness
Being mentally and emotionally ready is just as important. We suggest:
- Try stress-reducing activities, like meditation or deep breathing.
- Get support from loved ones or support groups for emotional help.
- See a counselor or therapist to deal with surgery-related anxiety or fear.
Being mentally strong can make facing surgery easier.
Setting Realistic Pain Expectations
It’s important to understand what pain you might feel after surgery. Patients should:
- Talk to their doctor about pain management options.
- Know that some pain is normal but can be managed with the right treatment.
- Watch for signs of complications that need quick medical help.
Having realistic pain expectations can help you handle recovery better.
Pain During Scoliosis Surgery
Anesthesia and pain management strategies keep patients comfortable during scoliosis surgery. This surgery is complex and needs careful pain control for the patient’s comfort and safety.
Anesthesia and Intraoperative Pain Management
Anesthesia is key in managing pain during scoliosis surgery. General anesthesia makes sure the patient is asleep and pain-free. Our anesthesiologists work with the surgical team to adjust anesthesia levels as needed.
Choosing the right anesthesia is a detailed process. It involves a thorough check before surgery to find the best anesthesia for each patient.
What Happens During the Procedure
The patient is placed on the operating table for easy access to the spine. The surgery corrects the spine’s curve through spinal fusion. Intraoperative pain management is ongoing, with the anesthesiologist watching the patient’s vital signs and adjusting anesthesia as needed.
“The key to successful scoliosis surgery lies in the effective management of pain during the procedure, ensuring that the patient remains comfortable and safe throughout the operation.”
Monitoring Pain Levels During Surgery
Even though patients are under general anesthesia, it’s important to monitor pain levels. We use medical tools and techniques to check the patient’s responses to surgery. Our team is ready to act if there’s a sign of pain not being managed well.
By watching these responses closely, we can adjust anesthesia and pain management. This keeps the patient comfortable and ensures the surgery goes smoothly.
Immediate Post-Operative Pain Experience
Right after scoliosis surgery, the first 24-48 hours are key for managing pain. During this time, patients are watched closely in the hospital. They also get treatment for pain.
First 24-48 Hours After Surgery
The first 24-48 hours after surgery are usually the most painful. After scoliosis surgery, patients often experience discomfort, pain, and tiredness. Effective pain management is very important for a good recovery.
We make sure patients get the right pain relief medicine. The type and amount of medicine depend on the patient’s needs and medical history.
Hospital Pain Management Protocols
Hospitals have set pain management plans to help patients. These plans use both medicine and other methods.
Some common methods include:
- Patient-controlled analgesia (PCA) pumps
- Regional anesthesia techniques
- Oral pain medications
- Non-pharmacological methods such as deep breathing exercises and relaxation techniques
Common Pain Locations and Sensations
Patients may feel pain in different places after surgery, like the back, shoulders, and hips. The pain can feel sharp, dull, or aching.
Common pain spots include:
- The surgical site
- The shoulders and upper back from surgery position
- The hips and lower back from spinal changes
Knowing where and how pain feels can help patients prepare. It also helps them work with their healthcare team to manage pain.
Pain Management Techniques and Medications
Managing pain well is key for a smooth recovery after scoliosis surgery. There are many ways to handle post-operative pain. This helps patients feel better and get back to their daily life sooner.
Pharmaceutical Approaches
Medicines play a big role in managing pain after surgery. Opioids are often used for pain that’s not too bad. But, there are risks like addiction and side effects.
Doctors are now looking at other options like NSAIDs and acetaminophen. These can be used alone or with opioids to help control pain better.
Patient-Controlled Analgesia (PCA)
Patient-Controlled Analgesia (PCA) lets patients give themselves pain medicine when they need it. It’s used right after surgery and helps control pain well. Patients use a button to get a set amount of medicine through their IV.
Regional Anesthesia Options
Regional anesthesia blocks pain in certain areas by using local anesthetics. Epidural analgesia and nerve blocks are examples. They can cut down on the need for strong pain medicines.
For scoliosis surgery patients, regional anesthesia can really help. It can make pain less and help recovery go faster.
Healthcare providers use these methods to make pain relief plans for each patient. This makes recovery better for scoliosis surgery patients.
The First Week of Recovery: Pain Progression
The first week after scoliosis surgery is key for managing pain and getting used to new limits. Knowing how pain usually changes and what affects it can ease worries and better outcomes.
Transitioning from Hospital to Home
Leaving the hospital is a big step in recovery. But moving from hospital care to home can be tough. Patients feel both relief and worry as they manage their pain on their own. Good communication with doctors and understanding post-op instructions are very important.
At home, patients need to rest but also move a bit. Gentle movement helps avoid blood clots and pneumonia. But, they must not push too hard, as it can make pain worse.
Activity Restrictions and Their Impact on Pain
Not doing too much is important for healing, but it can also hurt. Patients are told not to lift heavy, bend, or do hard activities in the first week. Following these rules is hard, mainly for those who are active or have family duties.
These rules affect pain in many ways. Rest is good for healing, but too much rest can make muscles stiff and sore. Moving a bit, as doctors suggest, can help avoid this and make recovery smoother.
Warning Signs of Abnormal Pain
Some pain is normal after scoliosis surgery, but there are signs of trouble. Look out for severe or getting worse pain that meds can’t fix. Also, pain with fever, swelling, or nerve problems is a red flag.
Spotting these signs early can stop serious problems. If you see any, get in touch with your doctor right away for help.
Weeks 2-6: Mid-Term Recovery Pain
Understanding pain during the mid-term recovery after scoliosis surgery is key. In weeks 2-6, the pain changes as the initial pain from surgery fades.
Expected Pain Timeline
Pain during this time can differ for everyone. Most people see their pain lessen as they get closer to the end of this period. Yet, some might feel pain, mainly after being active or at the end of the day.
| Week | Typical Pain Level | Activities |
| 2-3 | Moderate | Limited mobility, gentle stretching |
| 4-5 | Mild to Moderate | Increased mobility, introduction to physical therapy |
| 6 | Mild | Gradual return to daily activities |
Physical Therapy and Rehabilitation Pain
Physical therapy is vital for recovery, helping you regain strength and mobility. Yet, it can also cause pain, mainly in the first sessions.
Tips for Managing Physical Therapy Pain:
- Communicate openly with your physical therapist about your pain levels.
- Start with gentle exercises and gradually increase intensity.
- Use pain management strategies as advised by your healthcare provider.
One patient said, “Physical therapy was tough, but it was needed for recovery. I learned to manage my pain by pacing and talking to my therapist.”
Returning to Daily Activities
Getting back to daily life is a big step in recovery. By weeks 2-6, many can start doing some normal things again, but with limits.
It’s key to follow your surgeon’s advice on what activities to do to avoid problems and heal right.
As you get better, listen to your body. If pain gets worse or doesn’t go away, tell your doctor.
Long-Term Pain Considerations After Spinal Fusion
After spinal fusion surgery, long-term pain is a key concern. It’s important to know what can affect pain levels. Understanding these factors helps us see the long-term effects.
Residual Pain After Complete Healing
Residual pain is pain that stays even after the spine heals. It can come from the body’s reaction to the surgery hardware or how the spine adjusts.
Causes of residual pain include:
- Incomplete fusion or pseudarthrosis
- Hardware irritation or malfunction
- Adjacent segment disease
Hardware-Related Discomfort
Discomfort from the hardware used in surgery is another concern. The rods, screws, and other devices can sometimes cause irritation. This is more likely if they are noticeable or if the patient is sensitive.
Hardware discomfort can be caused by:
- Prominent hardware that irritates surrounding tissues
- Hardware malfunction or failure
- Allergic reactions to certain materials used in the hardware
Adjacent Segment Disease and Late-Onset Pain
Adjacent segment disease (ASD) is wear and tear in the spinal segments next to the fused area. It can cause pain that starts months or years after surgery.
Factors that lead to ASD include:
- Pre-existing degenerative conditions
- Biomechanical changes following fusion
- Genetic predisposition
Knowing about these pain concerns is key to managing expectations after spinal fusion. By understanding these issues, patients can work with their doctors to find effective pain management.
Potential Complications and Their Pain Implications
It’s important to know about the possible problems after scoliosis surgery. This helps manage pain and expectations. While surgery is usually effective, risks exist. Knowing these can help patients get ready for recovery.
Infection and Inflammatory Pain
Infection is a big risk after scoliosis surgery. It can cause more pain, swelling, and redness at the incision site. We do everything we can to avoid infections, but they can affect recovery and pain.
Infection management often means antibiotics and sometimes more surgery. It’s key for patients to watch their incision and tell their doctor if they see signs of infection.
Hardware Failure or Misplacement
Hardware like rods and screws is used to stabilize the spine during surgery. But, there’s a chance it might not work right or could fail. This might need more surgery to fix.
We use special imaging to make sure the hardware is placed correctly. But, patients should know about the chance of hardware problems and the pain they can cause.
Nerve Damage and Neuropathic Pain
Nerve damage is another risk of scoliosis surgery. It can cause sharp, shooting pain that’s hard to manage. We carefully check nerve function during surgery to lower this risk.
If nerve damage happens, we help patients find ways to manage pain. This might include medicine, physical therapy, and other treatments.
Pseudarthrosis (Failed Fusion)
Pseudarthrosis is when the bone doesn’t heal or fuse as hoped. This can cause ongoing pain and might need more surgery to fix. We talk to patients about this risk and how to help bones heal well.
By knowing about these complications and their effects on pain, patients can better prepare for surgery and recovery. We aim to give full care and support to reduce risks and improve results.
Patient Experiences and Testimonials
Real-life stories from patients who have had scoliosis surgery offer a glimpse into recovery. These stories are key for those considering surgery. They show the personal effects of the surgery.
Adolescent Patient Perspectives
For teens, scoliosis surgery is a big deal. Many feel a mix of emotions, from fear before surgery to relief afterward. Teens talk about how important emotional support is during healing.
- Pre-surgery anxiety and preparation
- Immediate post-surgery recovery experiences
- Returning to normal activities and sports
Adult Patient Experiences
Adults face different concerns and experiences than teens. The decision to have surgery is often about chronic pain and wanting a better life. Adults share the challenges and benefits of surgery.
- Expectations versus reality of pain levels
- The role of physical therapy in recovery
- Long-term outcomes and satisfaction
Comparing Expected vs. Actual Pain Levels
Pain is a big worry for patients. Comparing expected versus actual pain levels offers insights. Many say the pain was different than they thought.
| Aspect | Expected | Actual |
| Pain Level | High | Manageable with medication |
| Recovery Time | Longer | Varies by individual |
Looking at patient stories helps us understand scoliosis surgery and recovery. These accounts show the need for full care and support during the journey.
Non-Pharmacological Pain Management Strategies
Non-pharmacological strategies are key in managing pain after scoliosis surgery. They help reduce pain and improve life quality without medication. This way, they avoid side effects and dependency.
Physical Therapy Techniques
Physical therapy is a big part of non-pharmacological pain management. It includes gentle exercises and stretches. These help improve flexibility, strengthen muscles, and aid in healing.
We suggest starting with low-intensity activities. Then, increase the intensity as the patient gets more comfortable and progresses.
Physical therapy techniques may include:
- Gentle stretching to improve flexibility
- Strengthening exercises for core and back muscles
- Posture correction and body mechanics education
- Low-impact aerobic exercises like walking or swimming
Complementary and Alternative Approaches
Along with physical therapy, other approaches can help manage pain. These include:
- Acupuncture to stimulate healing and reduce pain
- Massage therapy to relax tense muscles
- Chiropractic care for spinal alignment
- Mind-body therapies like meditation and yoga
These methods can boost pain relief and overall well-being when used with traditional treatments.
Psychological Support and Pain Coping Strategies
Psychological support is vital for managing pain’s emotional side. Techniques like cognitive-behavioral therapy (CBT) help patients cope and improve their mental state.
Coping strategies may include:
- Relaxation techniques like deep breathing
- Visualization and guided imagery
- Journaling to express feelings and track progress
- Support groups to connect with others who have experienced similar challenges
By using these non-pharmacological strategies, patients can actively participate in their recovery. They may also reduce their need for pain medication.
Conclusion: Balancing Pain Expectations with Surgical Benefits
It’s key for patients to know about the pain in scoliosis surgery before deciding. We’ve looked at the different surgery types, what to do before surgery, and ways to manage pain.
It’s important to weigh the pain against the surgery’s benefits. Surgery can improve spinal alignment and reduce future problems. These benefits often make the temporary pain worth it.
Setting realistic pain expectations and using good pain management helps patients recover well. Being physically and mentally ready is key for a smooth recovery.
Scoliosis surgery can change lives, making them better for patients. Knowing about the pain and managing it leads to a good outcome. Patients can then enjoy the surgery’s lasting benefits.
FAQ
What is the typical pain experience like after scoliosis surgery?
Pain after scoliosis surgery varies. Most people feel a lot of pain in the first 24-48 hours. This pain is usually managed with medication.
How is pain managed during scoliosis surgery?
Anesthesia is used to block pain during surgery. This way, patients don’t feel pain. Techniques are also used to reduce pain during the operation.
What are the common pain locations and sensations after scoliosis surgery?
Pain often hits the back, shoulders, and hips. It can feel like dull aches or sharp pains. The worst pain usually happens in the first few days.
How long does it take to recover from scoliosis surgery?
Recovery time varies. Most people take weeks to months to fully recover. The first week is usually the toughest, with pain slowly getting better.
What are the possible long-term pain issues after spinal fusion surgery?
Long-term pain issues include pain that doesn’t go away, discomfort from hardware, and disease in other segments. These problems can show up months or years later.
Can scoliosis surgery cause nerve damage and neuropathic pain?
Yes, nerve damage is a risk. It can lead to neuropathic pain. This is a serious issue that needs quick medical help.
How can I manage pain after scoliosis surgery?
Managing pain involves several steps. This includes medicines, patient-controlled analgesia, and physical therapy. You can also try alternative methods.
What are the warning signs of abnormal pain after scoliosis surgery?
Watch for severe pain, numbness, or tingling, and pain that gets worse. If you notice these signs, call your doctor right away.
Can physical therapy help manage pain after scoliosis surgery?
Yes, physical therapy is key. It helps by improving movement, strength, and flexibility. This can reduce pain.
Are there any non-pharmacological pain management strategies for scoliosis surgery recovery?
Yes, there are. Non-pharmacological strategies include physical therapy, alternative methods like acupuncture, and psychological support.
How can I prepare myself for the pain associated with scoliosis surgery?
Prepare by setting realistic pain expectations. Practice relaxation techniques and follow your doctor’s pre-surgery advice.
What are the risks of infection after scoliosis surgery, and how can it affect pain?
Infection is a risk. It can cause pain, swelling, and redness. Quick medical care is needed to treat it and prevent damage.
Can I return to my normal activities after scoliosis surgery?
Yes, most people can go back to normal activities. But, follow your doctor’s advice and slowly increase your activity to avoid problems.
Reference:
PMC. (2025). Anesthesia and Pain Management for Scoliosis Surgery. , https://pmc.ncbi.nlm.nih.gov/articles/PMC12180691





