Last Updated on November 27, 2025 by Bilal Hasdemir
Every year, many women have hysterectomy surgery. It’s important to manage their pain well for a smooth recovery. Pain management with nerve block for hysterectomy. Learn how regional anesthesia reduces post-operative discomfort effectively.
Nerve blocks show promise as effective pain reduction methods.
For hysterectomy patients, nerve blocks are a big help. They make patients more comfortable and cut down on opioid use.
Regional anesthesia, like nerve blocks, is key in gynecologic surgery. It involves injecting local anesthetics around nerves to block pain signals. This method provides effective pain relief.
A nerve block is a pain management procedure that stops pain signals to the brain. In gynecologic surgery, it helps reduce pain during and after the operation. By targeting specific nerves, it cuts down the need for strong pain meds, reducing side effects.
The idea behind nerve blocks is simple. Local anesthetics are given near the nerves of the surgical area. This regional anesthesia keeps the patient comfortable during the surgery and recovery.
There are many nerve blocks used in pelvic surgery, each targeting different nerves. The choice depends on the surgical site and procedure type. Here are a few examples:
These blocks are vital for abdominal surgery pain relief. They are chosen based on the surgery and patient needs.
Knowing about these nerve blocks helps healthcare providers customize gynecologic surgery anesthesia. This improves pain management and surgical results for each patient.

Understanding the pelvic nerves is key for managing pain during hysterectomy. These nerves are vital for sending pain signals. Their complex paths need careful targeting for the best pain relief.
Several important nerve paths are touched during hysterectomy. These include:
These nerves are key in sending pain signals during and after hysterectomy. Knowing their layout is vital for targeted anesthesia.
Using nerve block procedures to target pelvic nerves can greatly cut down on pain after surgery. This makes patients more comfortable and leads to better results. By stopping pain signals at the start, nerve blocks help avoid the side effects of strong pain meds.
“Effective pain management is key for patient recovery and happiness after hysterectomy. Getting the right nerves with the right method can really help.”
Nerve block procedures offer precise pain control. This improves care for patients having hysterectomy.
After a hysterectomy, finding effective pain relief is key. Nerve blocks show promise as effective pain reduction methods. They work by injecting local anesthetics around specific nerves. This blocks pain signals to the brain.
Nerve blocks involve injecting local anesthetics around nerves that carry pain signals from the pelvic area to the brain. This blocks these signals, reducing pain for patients after hysterectomy surgery.
The duration of nerve block effectiveness varies. It depends on the local anesthetic type and the surgery type. Some blocks last hours, while others last days.
Understanding nerve blocks and their benefits helps patients and healthcare providers make informed decisions. This is for managing post-hysterectomy pain.
Many nerve block techniques are used to reduce pain after hysterectomy surgery. These blocks target specific nerves to help manage pain. This approach can lower the need for strong pain medicines and improve patient care.
The TAP block is a method of regional anesthesia. It involves injecting local anesthetic into the space between muscles. This block helps relieve pain in the front part of the abdomen.
Benefits: It’s great for post-operative pain relief and can reduce the need for opioids.
This block targets nerves in the lower abdomen and groin area. It’s very useful for surgeries in these areas.
Application: It’s often used with other blocks for better pain management.
The pudendal nerve block blocks the nerve that supplies the perineal area. It’s good for pain in the vaginal and perineal areas.
Indication: It’s very useful for vaginal hysterectomy or procedures that cause a lot of perineal trauma.
The quadratus lumborum block targets nerves in the back. It helps with pain in the abdomen and lower back.
Advantage: It provides long-lasting pain relief because the anesthetic spreads through fascial planes.
Comparing different nerve blocks helps doctors make better choices. The table below shows key details about the blocks we’ve discussed:
| Nerve Block Type | Target Area | Primary Use | Duration of Action |
| TAP Block | Anterior abdominal wall | Abdominal surgery pain | 12-24 hours |
| Ilioinguinal-Iliohypogastric Block | Lower abdominal wall | Lower abdominal surgery | 12-18 hours |
| Pudendal Nerve Block | Perineal area | Vaginal/perineal pain | 6-12 hours |
| Quadratus Lumborum Block | Posterior abdominal wall | Abdominal and lower back pain | 24-48 hours |
The right nerve block depends on the type of hysterectomy, where the pain is, and the patient’s needs. Knowing about each block helps doctors manage pain more effectively.
Medications are key in making nerve blocks work for patients having hysterectomies. Local anesthetics are the main drugs used. They have different effects on how long and well they work.
Local anesthetics are the heart of nerve block drugs. They block nerve signals, stopping pain from reaching the brain. Lidocaine and bupivacaine are common ones. The choice depends on how long the pain relief is needed and the type of procedure.
Lidocaine works for a short time, good for quick pain relief. Bupivacaine lasts longer, helping with pain after surgery.
Some additives can make nerve blocks last longer and work better. These include corticosteroids, opioids, and adjuvants like clonidine. They help reduce the need for other pain medicines and improve results.
Choosing additives depends on the surgery, patient health, and pain goals. By picking the right mix of local anesthetics and additives, doctors can better manage pain for hysterectomy patients.
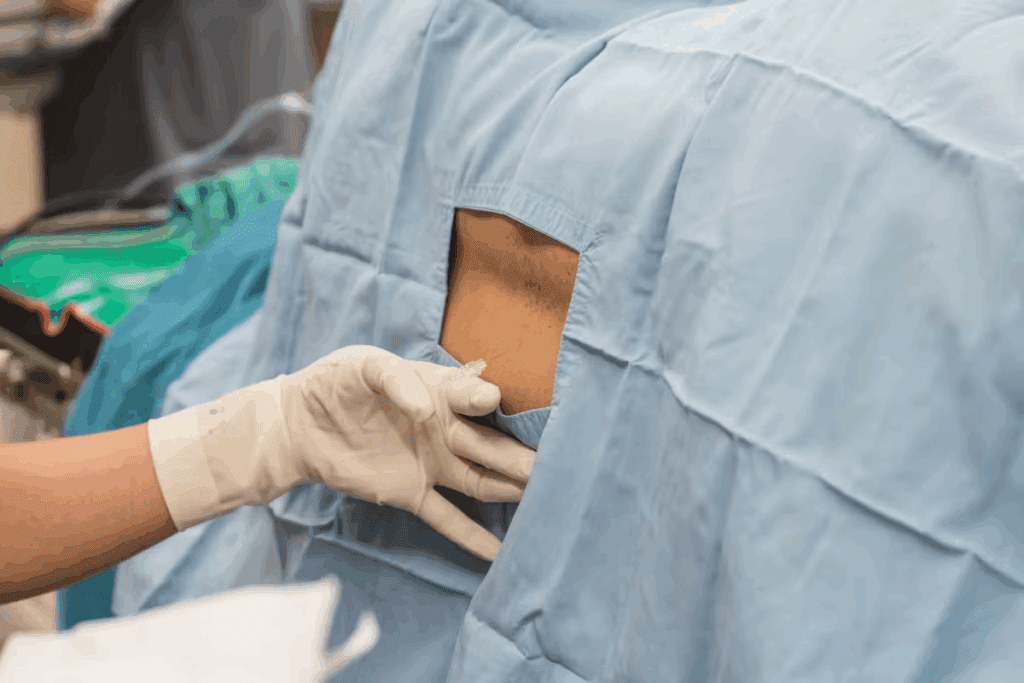
Administering nerve blocks is key for pain relief in hysterectomy patients. It involves several steps, from preparation to the actual block.
Patients get ready for a nerve block before surgery. They share their medical history, current meds, and allergies. The anesthesiologist talks about the block’s risks and benefits.
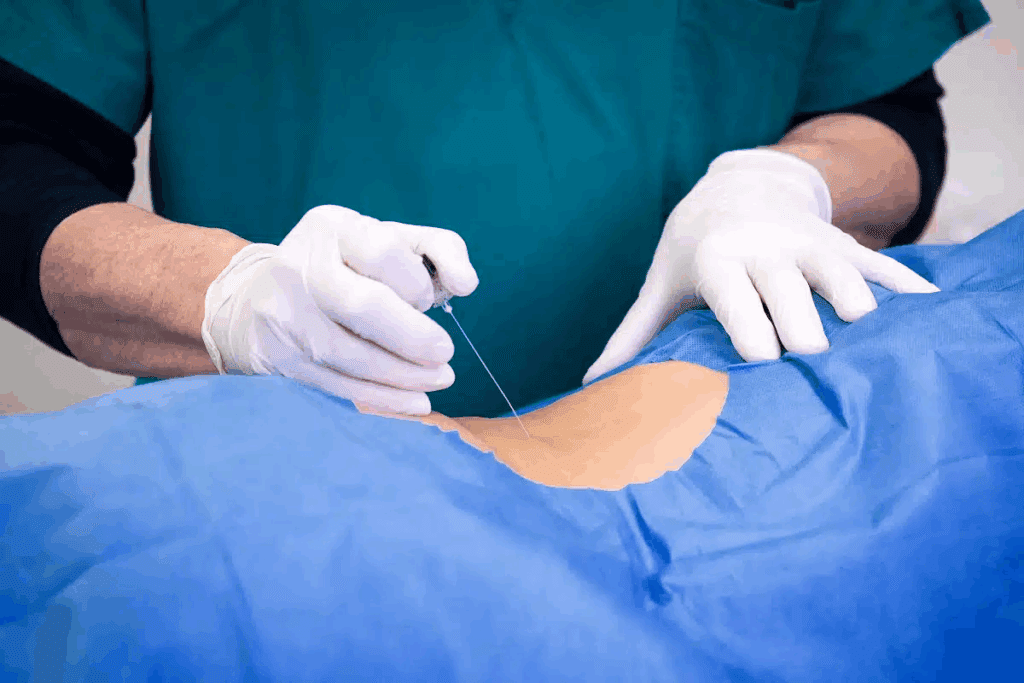
Administering nerve blocks requires special techniques. Landmark-based and ultrasound-guided methods are common. Ultrasound guidance is popular for its real-time view of the needle and anatomy.
Ultrasound is key for precise nerve block administration. It lets the anesthesiologist see the needle and nerves in real-time. This reduces risks and boosts block effectiveness.
| Technique | Advantages | Disadvantages |
| Landmark-based | Quick, no special gear needed | More risk, less precise |
| Ultrasound-guided | High precision, less risk | Needs special gear and training |
Ultrasound has changed regional anesthesia. It makes nerve blocks more precise and effective. As tech improves, so will pain management for hysterectomy patients.
Effective pain management is key after a hysterectomy. Nerve blocks are a great solution. They help manage pain well and cut down on the need for strong pain meds.
Nerve blocks give quick pain relief after surgery. This is important for comfort and recovery. They block pain signals to the brain, reducing pain for patients right after surgery.
A study showed nerve blocks greatly lowered pain scores. This quick relief helps patients recover better.
Nerve blocks also mean less need for strong pain meds like opioids. Opioids can be addictive and cause side effects like nausea and constipation.
Using nerve blocks instead helps manage pain safely and effectively. The table below shows how nerve blocks cut down opioid use.
| Pain Management Method | Opioid Consumption | Pain Relief Effectiveness |
| Nerve Blocks | Reduced | High |
| Systemic Pain Medications | High | Variable |
A medical expert says, “Nerve blocks are a game-changer in pain management. They offer a targeted approach that cuts down on systemic meds.” This method improves comfort and lowers opioid side effects.
“Regional anesthesia techniques, such as nerve blocks, are increasingly recognized for their role in reducing opioid consumption and improving pain outcomes.”
Nerve blocks are a big step forward in pain management for hysterectomy patients. They provide effective pain relief without the risks of strong pain meds. This makes them a valuable option for better patient outcomes.
The type of hysterectomy done affects the choice of nerve block for pain. Each surgery has its own pain needs. Knowing these helps manage pain better.
Abdominal hysterectomy is more invasive, needing a strong pain plan. Nerve blocks like the TAP block or Quadratus Lumborum block are used. They target nerves in the abdominal wall, helping a lot with pain.
The TAP block involves injecting anesthetic between muscles. It can greatly reduce pain and cut down on pain meds.
Vaginal hysterectomy is less invasive, but nerve blocks can help with pain. The pudendal nerve block is used for this. It targets nerves in the perineal area, giving good pain relief.
The right nerve block for vaginal hysterectomy depends on the surgery and the patient’s pain. Anesthesiologists mix nerve blocks with other methods for the best comfort.
Laparoscopic and robotic hysterectomies are less painful than open surgery. But, nerve blocks can help with pain. For laparoscopic surgeries, the TAP block might be used, though it’s not always needed.
Robotic hysterectomy, being a laparoscopic surgery with better precision, also uses a mix of pain management. Even with less pain, nerve blocks help keep patients comfortable during recovery.
A new way to manage pain in gynecologic surgery is using nerve blocks with other methods. This approach combines different pain treatments for better results. It makes patients more comfortable and helps them recover faster.
This method uses many pain management strategies at once. It mixes nerve blocks with other treatments like medicines. This way, doctors can make a pain plan that works best for each patient.
“The use of multimodal anesthesia has changed how we manage pain in surgery,” says a top anesthesiologist. “By mixing nerve blocks with other methods, we get better pain relief and better results for patients.”
Other pain control methods can also help. These include:
Adding these methods to nerve blocks makes pain management even better. It helps patients get the most out of their treatment.
Nerve blocks for hysterectomy come with risks and side effects. It’s important to know these to make good choices about pain relief.
Nerve blocks are usually safe, but some people might feel numb or weak. This feeling usually goes away by itself. Talking to your doctor about these side effects is key to understand how they might affect your healing.
Though rare, serious problems can happen with nerve blocks. These include infections, nerve damage, or allergic reactions. Knowing these risks and watching your health after the procedure is important.
| Complication | Description | Frequency |
| Infection | Bacterial infection at the site of the nerve block | Rare |
| Nerve Damage | Permanent or temporary damage to the nerves | Very Rare |
| Allergic Reaction | Reaction to the local anesthetic or other medications | Rare |
Some things can make nerve block risks higher. These include health problems like diabetes or past issues with anesthesia. Talking to your anesthesiologist about your health history is important to lower risks.
Knowing the risks and side effects helps patients choose the best pain relief. It’s about weighing the benefits of pain relief against the possible risks of nerve blocks.
Choosing nerve blocks for hysterectomy depends on a patient’s health, surgery complexity, and pain needs. They are a good pain management option but not for everyone.
Those at high risk of pain after surgery or sensitive to opioids are good candidates. People with chronic pain or complex surgeries also benefit.
Characteristics of Ideal Candidates:
| Patient Profile | Nerve Block Suitability |
| High risk of postoperative pain | Highly Suitable |
| Sensitive to opioids | Highly Suitable |
| History of chronic pain | Suitable |
| Simple surgical procedure | May be Suitable |
Nerve blocks are not for everyone. Certain conditions, infections, or anticoagulant therapy make them unsuitable.
Contraindications for Nerve Blocks:
Deciding on nerve blocks should involve an anesthesiologist. They consider the patient’s medical history and surgery needs.
Knowing what to expect and how to prepare for a nerve block is key for patients having a hysterectomy. A nerve block can greatly improve your pain management. But, it needs careful planning and a talk with your healthcare team.
Before your hysterectomy, talking with your anesthesiologist about the nerve block is vital. This talk is a big part of getting ready for surgery. You’ll learn about the benefits and risks of nerve blocks.
You’ll share your medical history and past pain management experiences. You’ll also talk about your pain control preferences during and after surgery. Your anesthesiologist will explain the types of nerve blocks available. They’ll pick the best one for you based on your needs.
On surgery day, knowing what to expect can make you feel less anxious. Before the nerve block, you’ll go to a pre-operative area. Your anesthesiologist will get you ready for the procedure.
This may include positioning you and cleaning the area for the block. They might use ultrasound to place the block accurately. You might feel some discomfort during the block, but it’s usually brief.
The pain management procedure aims to be as comfortable as possible. Your anesthesiologist will try to keep any discomfort to a minimum. After the block, you’ll be watched for a bit to see how it’s working and if there are any side effects.
Being well-prepared and informed about your nerve block and hysterectomy helps a lot. Your healthcare team will support you from the start to after you recover. They’re there to help every step of the way.
Knowing what to expect after a hysterectomy can make recovery easier. It’s important to manage pain well for a smooth recovery.
The first 24 hours after surgery are key for managing pain. Patients often feel discomfort, pain, and tiredness. Effective pain relief methods are needed to handle these feelings. Doctors use medicines and nerve blocks to keep patients comfortable.
Patients who have had a hysterectomy say having a supportive team is vital. One patient noted, “Knowing what to expect and having a dedicated team helped a lot in my recovery.”
Recovery over time means getting more comfortable and less pain. Patients should stick to a structured recovery plan. This includes resting, doing some physical activity, and seeing their doctor regularly.
| Recovery Aspect | First 24 Hours | Long-term Recovery |
| Pain Management | High reliance on medication and nerve blocks | Gradual reduction in pain medication |
| Physical Activity | Limited mobility | Gradual increase in activity level |
| Follow-up Care | Immediate post-surgery monitoring | Regular follow-up appointments |
By understanding the recovery process and following doctor’s orders, patients can recover more comfortably and quickly.
Regional anesthesia is changing how we manage pain in gynecologic surgery. New techniques and technologies are making procedures safer and more effective for patients.
New methods in regional anesthesia aim to improve pain management. Ultrasound-guided nerve blocks are now used more often. They help place local anesthetics more accurately, leading to better pain relief and fewer complications.
New local anesthetics are also being developed. These have longer-lasting effects and are safer for patients. This means better outcomes for those undergoing surgery.
The future of regional anesthesia in gynecologic surgery looks promising. Precision medicine will play a big role. This means treatments will be tailored to each patient’s needs, based on their unique characteristics.
Technology will also be key. Things like continuous nerve block catheters and advanced drug delivery systems will help manage pain better. These advancements could greatly improve recovery times for surgery patients.
Nerve blocks are now a key part of managing pain after hysterectomy. They make patients more comfortable and help them heal faster. This method targets pain in specific areas, reducing the need for strong pain medicines.
Adding nerve blocks to hysterectomy care is a big step forward. They help patients feel better and recover sooner. This leads to better results for women having this surgery.
As regional anesthesia keeps getting better, nerve blocks will play an even bigger role. New techniques and medicines will make them even more important. They will keep being a big part of how we manage pain during hysterectomy.
A nerve block is a way to manage pain by blocking nerve signals. It involves injecting local anesthetics around specific nerves. This stops pain signals from reaching the brain, helping to relieve pain after hysterectomy surgery.
There are several types of nerve blocks, like TAP blocks and ilioinguinal-iliohypogastric blocks. Pudendal nerve blocks and quadratus lumborum blocks are also used. Each targets different nerves for various surgical procedures or pain types.
Nerve blocks work by injecting local anesthetics around nerves. This blocks pain signals to the brain. The block’s duration depends on the local anesthetic used and the procedure, providing relief for hours or days.
Nerve blocks can greatly improve pain management after surgery. They reduce the need for opioids and other pain meds. This provides immediate relief, making recovery more comfortable.
Yes, nerve blocks can be used for all types of hysterectomy procedures. The type of hysterectomy affects the choice of nerve block, ensuring the right pain management strategy.
While generally safe, nerve blocks can have side effects like nerve damage or infection. Knowing these risks helps make informed decisions. Precise technique and careful planning can reduce these risks.
The right candidate for nerve blocks depends on medical history and surgery type. Those benefiting from regional anesthesia are ideal. Certain conditions or allergies may make them unsuitable.
Patients should talk to their anesthesiologist about options and understand the procedure. They should follow pre-operative instructions. On surgery day, the nerve block is administered before or during surgery, using ultrasound for precision.
Patients can expect effective pain management in the first 24 hours and during recovery. Nerve blocks reduce the need for systemic pain meds, improving comfort and recovery.
Yes, regional anesthesia is evolving with new techniques and technologies. Advances include better ultrasound guidance, new local anesthetics, and other pain relief methods. These innovations improve patient outcomes and comfort.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!