Last Updated on November 26, 2025 by Bilal Hasdemir
Cancer doctors often suggest chemotherapy in two main ways. It can cure some cancers, giving patients a good chance at long-term survival. But for most cancers that have spread, chemotherapy aims to reduce tumors, ease symptoms, and extend life expectancy.
When cancer has grown too far, palliative care becomes key. This type of cancer treatment aims to ease symptoms and stress from serious illness. It’s designed to enhance the quality of life for patients and their families.
Key Takeaways
- Chemotherapy can be curative for certain types of cancer.
- For advanced cancers, chemotherapy is used to prolong life and alleviate symptoms.
- Palliative care is a critical component of cancer treatment.
- Understanding the role of palliative chemotherapy is essential for patients.
- Life expectancy can be extended with appropriate cancer treatment.
Understanding Chemotherapy and Its Purpose

Chemotherapy is a key cancer treatment. It uses drugs to kill cancer cells. It helps cure cancer, slow its growth, or ease symptoms.
How Chemotherapy Works in the Body
Chemotherapy targets fast-growing cells, like cancer cells. But it also affects healthy cells that grow quickly. This can cause side effects like hair loss and nausea.
Different Types of Chemotherapy Treatments
There are many types of chemotherapy. Each has its own use and benefits. Here are a few:
- Adjuvant chemotherapy: Given after primary treatment to reduce the risk of cancer recurrence.
- Neoadjuvant chemotherapy: Administered before the main treatment to shrink tumors.
- Palliative chemotherapy: Focuses on relieving symptoms and improving quality of life.
| Type of Chemotherapy | Purpose | Common Applications |
| Adjuvant | Reduce recurrence risk | Breast, colon cancer |
| Neoadjuvant | Shrink tumors before the main treatment | Breast, lung cancer |
| Palliative | Relieve symptoms, improve quality of life | Advanced cancers |
Chemotherapy is a flexible treatment. It can be adjusted for each patient’s needs and cancer type. Knowing how it works and its types helps patients make better choices about their care.
Palliative Chemotherapy: Definition and Goals
The main aim of palliative chemotherapy is to ease the pain of cancer patients. It’s for those with advanced cancer or who can’t get curative treatments.
Palliative care aims to reduce symptoms and stress from serious illnesses. It aims to boost the quality of life for patients and their families. Palliative chemotherapy helps manage symptoms like pain and nausea, not to cure cancer.
What Makes Treatment “Palliative” Instead of Curative
Palliative and curative treatments have different goals. Curative treatments aim to get rid of cancer. Palliative treatments, like chemotherapy, focus on managing symptoms and improving life quality. They’re used when cancer is advanced or treatments don’t work anymore.
Setting Realistic Expectations for Treatment Outcomes
It’s key to set realistic hopes in palliative care. Patients and families should know that palliative chemotherapy doesn’t aim to cure cancer. It’s to make the patient more comfortable.
Understanding palliative chemotherapy’s goals and limits helps patients make better care choices. They can focus on what’s most important in their remaining time.
Life Expectancy Benefits of Palliative Chemotherapy
It’s important to know how palliative chemotherapy affects life expectancy. This treatment aims to ease symptoms, improve life quality, and possibly extend life for those with advanced cancer.
Average Survival Extension Across Cancer Types
The benefits of palliative chemotherapy vary by cancer type. For example, some cancers, like colorectal and breast cancer, respond well. But others, like pancreatic cancer, may not be as much.
Studies have shown that it can add months to life. For colorectal cancer, adding chemotherapy to care can extend life by 6-9 months.
Factors That Influence Survival Outcomes
Many things affect how long a patient lives with palliative chemotherapy. These include age, health, and the cancer’s genetics.
Age and Overall Health Considerations
Older or sicker patients might not get as much benefit from chemotherapy. It’s key to think about these when choosing treatments.
Cancer-Specific Genetic Factors
Genetic traits of the cancer also matter. Some mutations make tumors more likely to respond to chemotherapy. This can affect how long a patient lives.
“Using genetic tests to plan treatment can make chemotherapy more effective,” said a top oncologist.
Healthcare providers can improve life expectancy by understanding these factors. They can then tailor treatments to help patients live longer.
Palliative Chemotherapy Outcomes by Cancer Type
Palliative chemotherapy results differ for each cancer type. This affects treatment choices and how long patients might live. Knowing how each cancer reacts to chemotherapy is key to better care.
Lung Cancer Life Expectancy
Lung cancer patients might live longer with palliative chemotherapy. Some lung cancer types do better with chemotherapy. For example, non-small cell lung cancer (NSCLC) patients might see better results with targeted therapies, too.
Colorectal Cancer Survival Rates
Colorectal cancer patients get different survival times with chemotherapy. It helps manage symptoms and might extend life. Studies suggest adding targeted therapy to chemotherapy can help some patients live longer.
Pancreatic Cancer Treatment Outcomes
Pancreatic cancer is tough to treat. Palliative chemotherapy aims to improve life quality and survival. Some chemotherapy plans show promise in improving life and survival for some patients.
Breast and Ovarian Cancer Response Rates
Breast and ovarian cancers react differently to chemotherapy. For breast cancer, adding hormone therapy can help. Ovarian cancer also benefits from chemotherapy, improving survival and quality of life for some.
In summary, chemotherapy results vary by cancer type. This shows the importance of tailored treatments. Healthcare providers and patients need to understand these differences for better treatment plans.
Is Chemotherapy Worth It for Stage 4 Cancer?
For those with stage 4 cancer, choosing chemotherapy is a big decision. It’s influenced by many things, like the benefits, side effects, and how it affects life quality.
Weighing Benefits Against Side Effects
Chemotherapy can help extend life and ease symptoms for stage 4 cancer patients. But, it also comes with big side effects like tiredness, nausea, and hair loss. Patients need to think carefully about these points and their own situation.
Quality of Life Considerations
How chemotherapy affects life quality is key for stage 4 cancer patients. It can make symptoms better and maybe even add more time to life. But it can also make daily life harder because of side effects. Managing these side effects well is important for keeping a good quality of life.
What Research Shows About Advanced Cancer Treatment
Research on treating advanced cancer has given us important information about chemotherapy for stage 4 cancer. The results vary based on the cancer type, patient health, and treatment plan. For example, a study showed chemotherapy helped some stage 4 cancer patients live longer.
| Cancer Type | Average Survival Extension | Quality of Life Improvement |
| Lung Cancer | 6-12 months | Moderate |
| Colorectal Cancer | 9-18 months | Significant |
| Pancreatic Cancer | 3-6 months | Minimal |
In the end, deciding on chemotherapy for stage 4 cancer should be a detailed talk between the patient and their doctor. They should consider all the factors and what the treatment aims to achieve.
Common Chemotherapy Schedules and Duration
Chemotherapy plans change a lot based on the cancer type and treatment goals. The treatment’s frequency and length are set based on the patient’s needs and cancer specifics.
There are many common chemotherapy schedules. Weekly treatment protocols are used for some cancers. This schedule helps manage side effects and improve results.
Weekly Treatment Protocols
Weekly chemotherapy means getting treatment once a week. It’s often used for cancers needing frequent, lower doses.
Three-Week Cycle Treatments
The three-week cycle treatment is another common schedule. It involves one day of treatment followed by two to three weeks of rest. This helps the body recover from treatment side effects.
How Many Rounds of Chemotherapy Are Typical
The number of chemotherapy rounds varies by cancer type, stage, and treatment goals. Usually, patients get between 4 to 8 cycles.
| Cancer Type | Typical Chemotherapy Cycles | Treatment Duration |
| Breast Cancer | 4-6 cycles | 3-6 months |
| Colorectal Cancer | 6-8 cycles | 4-6 months |
| Lung Cancer | 4-6 cycles | 3-4 months |
A medical oncologist says, “The chemotherapy schedule aims to be effective while keeping side effects low.”
“Chemotherapy is a complex treatment that requires careful planning and monitoring to achieve the best possible outcomes.”
How Long Can a Patient Receive Chemotherapy?
The time a patient gets chemotherapy varies a lot. It depends on their health, how well they respond to treatment, and their condition.
Maximum Duration of Treatment Courses
Chemotherapy courses can last from a few months to several years. The length of treatment depends on the cancer type, its stage, and how well the patient responds.
Taking Breaks Between Treatments
Patients often need breaks between treatments to recover. The length of these breaks varies based on the patient’s health and the treatment plan. During these times, patients rest, and their treatment plans might be adjusted.
When Multiple Lines of Chemotherapy Are Considered
Some patients get multiple lines of chemotherapy. This happens when the first treatment stops working and new treatments are needed. Deciding on multiple lines of chemotherapy depends on the patient’s health, how the cancer has responded, and the treatment’s benefits and risks.
Knowing what affects chemotherapy duration helps patients and their families make better choices about their care.
When Palliative Chemotherapy May Not Be Recommended
Palliative chemotherapy can be helpful, but it’s not always the right choice. The decision to use it depends on the patient’s health and the treatment’s benefits and risks.
Poor Performance Status Considerations
Patients who are very weak or have a low level of functioning might not benefit from palliative chemotherapy. The treatment could be too hard, and the risks might be too high.
| Performance Status | Description | Potential for Palliative Chemotherapy |
| 0-1 | Fully active or restricted in physically strenuous activity | High |
| 2-3 | Limited in activity, capable of self-care | Moderate |
| 4 | Completely disabled, unable to carry out self-care | Low |
End-of-Life Care Transitions
When patients are close to the end of life, the focus changes. Instead of trying to cure or extend life, the goal is to improve comfort and quality of life. Palliative chemotherapy is often not recommended in these situations.
When Risks Outweigh Possible Benefits
In some cases, the risks of palliative chemotherapy, like severe side effects, might be too great. Doctors carefully weigh these factors to decide the best treatment for each patient.
The choice not to use palliative chemotherapy is made for each patient separately. It considers their condition, preferences, and goals.
Monitoring Treatment Effectiveness
Checking how well chemotherapy works involves several important signs. Doctors watch these signs closely. They help figure out if the treatment is working and if changes are needed.
Tumor Markers and Imaging Results
Tumor markers are substances made by cancer cells or in response to cancer. Blood tests track these markers to see how treatment is going. Imaging tests like CT scans, MRI, and PET scans show how big and spread out tumors are. Together, these tools give a full picture of how well treatment is working.
Symptom Improvement as an Indicator
Getting better symptoms is a key sign of treatment success. People on chemotherapy often notice less pain or more energy. Doctors look at these personal reports along with test results to understand treatment success.
How Often Is It Evaluated
How often treatment success is checked depends on the cancer type, its stage, and the treatment plan. Usually, checks happen every few rounds of chemotherapy. This helps see if treatment is working and if changes are needed.
By watching these signs, doctors can decide to keep, change, or stop chemotherapy. Their goal is to help patients get better.
When Chemotherapy Stops Working: Next Steps
When chemotherapy stops working, it’s a big moment in cancer treatment. It’s time to think about other options. Understanding treatment resistance and what to do next is key.
Recognizing Treatment Resistance
Treatment resistance happens when cancer cells find ways to avoid chemotherapy. Doctors use tests like imaging and tumor markers to spot it. Finding resistance early helps in choosing the right next steps.
Alternative Treatment Options
When chemotherapy fails, doctors might suggest other treatments. These could be targeted therapy, immunotherapy, or clinical trials. These aim to slow cancer growth and ease symptoms. It’s important to talk about the good and bad of these options with an oncologist.
Transitioning to Comfort-Focused Care
Some patients might choose comfort-focused care instead. This focuses on managing symptoms and improving life quality. It can be used with or without other treatments, based on what the patient needs.
Knowing your options and what they mean is important when chemotherapy stops working. Talk to your healthcare team about what you want. This helps decide the best next steps.
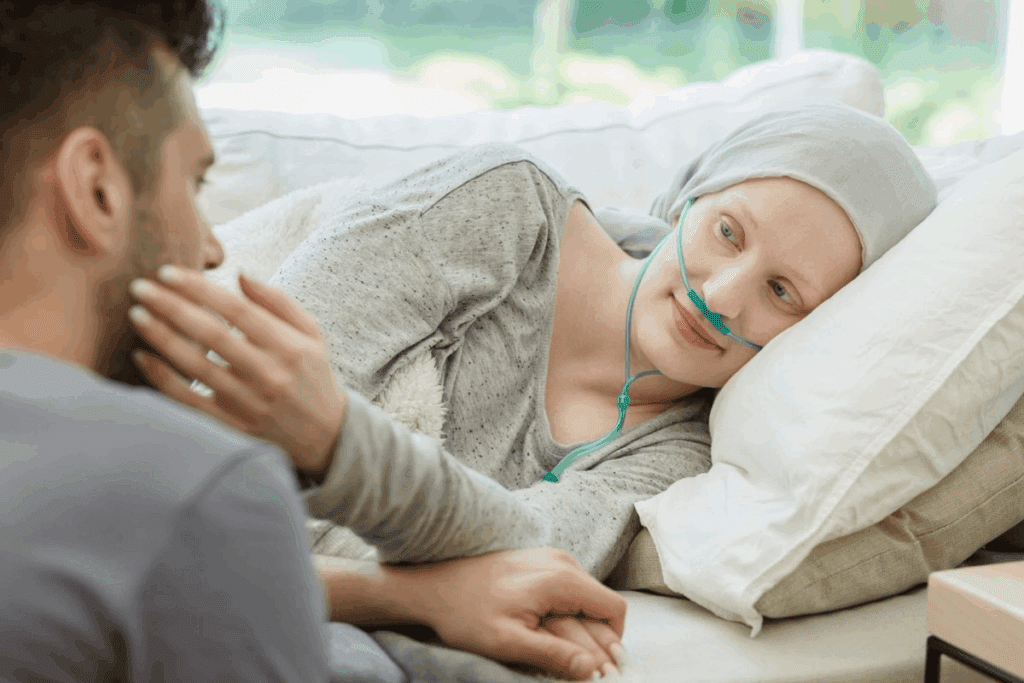
The Emotional Impact of Palliative Treatment Decisions
Palliative treatment decisions can deeply affect patients and their families. Palliative care aims to improve quality for those with serious illnesses. Yet, it also has a big emotional impact.
Coping with Uncertainty About Prognosis
Dealing with the unknown about a patient’s future is hard. Families often worry and fear about what might happen. This uncertainty can cause a lot of anxiety.
Uncertainty can be lessened by clear and caring talks from doctors. It’s key for patients and their families to talk openly with their oncologists. They should discuss the possible outcomes and what palliative care can offer.
Supporting Family Members Through Treatment
Palliative care affects not just patients but also their families deeply. It’s important to support loved ones during this time. Healthcare providers can help by giving resources and advice.
| Support Strategies | Description | Benefits |
| Family Counseling | Provides emotional support and guidance for family members | Enhances coping mechanisms, reduces stress |
| Support Groups | Connects families with others experiencing similar challenges | Fosters a sense of community, shares experiences |
| Resource Allocation | Helps families access necessary resources and services | Reduces logistical burdens, improves quality of life |
Finding Meaning During Palliative Care
Finding purpose and meaning is vital during palliative care. Patients and families can find ways to make special moments and memories. This can bring comfort and fulfillment.
Meaning-making activities might include spending time with loved ones, doing hobbies, or creating legacies. These actions can help find joy and purpose.
Financial Considerations of Ongoing Chemotherapy
Many patients worry about the cost of ongoing chemotherapy. As treatment goes on, expenses add up fast. This can hurt a patient’s money and their choices about treatment.
Insurance Coverage for Palliative Treatments
It’s key to know what insurance covers for chemotherapy costs. Most plans help pay for some of these costs. But how much help varies a lot. Patients should check their insurance to know what they’ll pay for themselves.
Patient Assistance Programs
For those struggling financially, help is available. Programs from drug companies, non-profits, and the government can offer big support. They can lower the cost of chemotherapy by giving discounts or free meds.
Balancing Cost and Benefit in Treatment Decisions
Patients and doctors must think about the costs and benefits of chemotherapy. They look at how likely treatment is to work, its effect on life quality, and the money it costs. Important things to think about include:
- The cost of treatment and what you might have to pay yourself
- The good things treatment can do, like living longer and feeling better
- Other treatment options and their costs
By thinking about these points, patients can make choices that fit their financial situation and health needs.
Life Expectancy After Stopping Chemotherapy
Life expectancy after stopping chemotherapy varies a lot. It depends on many factors. Knowing these factors and typical timelines for different cancers helps patients and families make better choices.
Typical Timelines by Cancer Type
The type of cancer greatly affects life expectancy after chemotherapy. For example, lung cancer patients might face a different outlook than those with breast cancer.
| Cancer Type | Average Life Expectancy |
| Lung Cancer | 4-6 months |
| Breast Cancer | 12-18 months |
| Colorectal Cancer | 9-12 months |
Factors That Influence Post-Treatment Survival
Many factors can affect survival after chemotherapy stops. These include the patient’s health, cancer stage, and how well the cancer responded to treatment. Overall health is key, as those with fewer health issues tend to do better.
Planning for End-of-Life Care
Planning for end-of-life care is vital after chemotherapy. It involves talking to healthcare providers, considering palliative care, and making personal and financial plans.
Understanding what affects life expectancy and making informed choices helps patients through this tough time.
Comprehensive Palliative Care Beyond Chemotherapy
Palliative care is key in managing cancer symptoms and improving patient outcomes. It focuses on easing the symptoms and stress of serious illnesses. The goal is to enhance the quality of life for patients and their families.
Symptom Management Approaches
Effective symptom management is central to palliative care. It involves treating pain, nausea, fatigue, and other symptoms that affect quality of life. Palliative care teams use various interventions, like medications, physical therapy, and counseling, to manage symptoms.
Integrating Palliative Care with Oncology
Integrating palliative care with oncology requires teamwork. Oncologists, palliative care specialists, and other healthcare professionals work together. This integration can happen at any stage of cancer treatment, from diagnosis to end-of-life care. Together, they provide care that meets all patient needs.
Supportive Therapies That May Extend Survival
Supportive therapies like nutritional support, psychological counseling, and physical therapy are vital. They help patients stay strong, manage side effects, and improve well-being. A study in the Journal of Clinical Oncology found that “integrated palliative care programs can improve patient outcomes and potentially extend survival.”
“Palliative care interventions have been shown to improve quality of life and, in some cases, survival.”
| Supportive Therapy | Benefits |
| Nutritional Support | Maintains strength, manages treatment side effects |
| Psychological Counseling | Reduces stress, improves mental well-being |
| Physical Therapy | Enhances mobility, reduces pain |
Communicating with Your Oncologist About Prognosis
Talking openly with your oncologist is key to understanding your prognosis. It helps you make smart choices about your care. Ask the right questions to get clear answers about your life expectancy and treatment options.
Questions to Ask About Life Expectancy
When asking about your life expectancy, consider a few things. Ask about the average survival rates for your cancer type. Also, find out how your health and treatment response might affect your prognosis.
You might also want to know the goals of your treatment. Make sure they match your personal values and priorities.
Understanding Survival Statistics
Survival statistics can be tricky to understand. They’re based on data from previous cases and might not apply to you. Your oncologist can help make sense of this data for you.
Shared Decision-Making Approaches
Shared decision-making is a team effort between you and your oncologist. It considers your preferences, values, and medical needs. Together, you can create a treatment plan that fits your goals and priorities.
Conclusion: Making Informed Decisions About Cancer Treatment
Understanding cancer treatment and palliative care is key for patients. It helps them make smart choices about their care. Knowing about palliative chemotherapy, life expectancy, and survival factors is important.
Palliative care is more than just chemotherapy. It includes managing symptoms, supportive therapies, and overall care. This can improve survival and quality of life. Talking openly with oncologists about prognosis and treatment goals is important.
Good decision-making in cancer treatment means weighing therapy benefits and risks. It also involves thinking about costs and planning for end-of-life care. By considering these, patients and families can understand their care better.
FAQ
What is palliative chemotherapy?
Palliative chemotherapy is a cancer treatment. It aims to ease symptoms, improve life quality, and extend life. It’s not meant to cure the disease.
How long can you be on chemotherapy?
Chemotherapy time varies. It depends on the cancer type, treatment goals, and the patient’s health. Some may get treatment for months, while others for years.
Is palliative chemotherapy worth it for stage 4 cancer?
Deciding on chemotherapy for stage 4 cancer is complex. It depends on the patient’s health, symptoms, and goals. Chemotherapy can improve life quality and extend life, but consider the side effects.
How often do you have chemotherapy?
Chemotherapy schedules differ. Treatments can be weekly, every three weeks, or monthly. The frequency depends on the cancer type, treatment plan, and patient needs.
What happens when chemotherapy stops working?
If chemotherapy stops working, patients might need new treatments. This could include switching to another chemotherapy regimen or focusing on comfort care. Talking to an oncologist about next steps is key.
How long do cancer patients live after stopping chemotherapy?
Life after stopping chemotherapy varies. It depends on the cancer type, health, and other factors. Patients should talk to their oncologist about what to expect.
What are the common chemotherapy schedules?
Common schedules include weekly, three-week cycles, and monthly treatments. The schedule varies based on the cancer type and treatment plan.
Can chemotherapy cure cancer?
Chemotherapy can cure some cancers. But for advanced cancer, it aims to extend life and ease symptoms. The goal depends on the cancer type and patient factors.
How many rounds of chemotherapy are typical?
Rounds of chemotherapy vary. It depends on the cancer, treatment goals, and patient health. Some may get a few cycles, while others may be treated for months or years.
What is the maximum duration of chemotherapy treatment?
Chemotherapy duration varies. It depends on the cancer, treatment goals, and patient factors. Some may be treated for years, while others may stop due to side effects or disease progression.
How is treatment effectiveness monitored?
Effectiveness is checked through regular assessments. This includes tumor markers, imaging, and symptom improvement. Patients should discuss their treatment response with their oncologist.
What are the financial considerations of ongoing chemotherapy?
Chemotherapy can be expensive. Patients should talk to their oncologist about insurance, patient assistance programs, and the cost-benefit balance.
How can patients cope with the emotional impact of palliative treatment decisions?
Patients can cope by seeking support from family, friends, and healthcare professionals. Discussing feelings and concerns with an oncologist is important for complete care.
What is complementary palliative care beyond chemotherapy?
Beyond chemotherapy, palliative care includes symptom management and supportive therapies. It aims to extend survival. Patients should discuss their needs with their oncologist.
How can patients communicate effectively with their oncologist about prognosis?
Patients can ask questions about life expectancy and survival statistics. Open discussions with an oncologist are key to informed decisions.
Reference
- Shaikh, S., & Asif, M. (2022). Cancer chemotherapy and beyond: current status, drug candidates & future directions. ScienceDirect. https://www.sciencedirect.com/science/article/pii/S2352304222000472
- ASCO (2024). Palliative Care for Patients With Cancer: ASCO Guideline Update. Journal of Clinical Oncology.https://ascopubs.org/doi/10.1200/JCO.24.00542