Menopause is a big change in a woman’s life, ending her monthly periods. It usually happens between 45 and 55 years old. This guide to the pathology of menopause explains 7 critical changes. Learn the essential facts on hormones, labs, and diagnosis.
Menopause is when a woman hasn’t had her period for 12 months. In the US, the average age for this is 51 years.
Knowing about the pathophysiological changes in menopause is key. It helps doctors give the right care and treatments.
Key Takeaways
- Menopause is a natural biological process marking the end of menstruation.
- The clinical definition involves 12 consecutive months of amenorrhea.
- The median age of menopause in the US is 51 years.
- Understanding menopause pathophysiology is essential for symptom management.
- Hormonal changes play a significant role in the menopause transition.
Understanding Menopause: Definition and Clinical Significance
Menopause is when a woman stops getting her period for good. This happens because her ovaries stop working. It’s officially recognized when a woman hasn’t had her period for 12 months. Knowing about menopause is key for doctors and women going through it.
Clinical Definition and Age of Onset
Menopause usually happens between 45 and 56 years old, with most women experiencing it at 51. Many things can affect when a woman goes through menopause, like her genes and lifestyle. It’s a natural part of aging for women.
Doctors use a specific rule to say a woman is in menopause. They look back to see if she hasn’t had her period for 12 months. This rule helps tell menopause apart from other issues that might mess with a woman’s cycle.
Stages of Menopausal Transition
The journey to menopause starts before the last period and is called perimenopause. This stage can last for years and brings hormonal changes and irregular periods. Women might feel hot flashes and other symptoms during this time.
- Early menopausal transition: Menstrual cycles start to get irregular, but they’re not more than 60 days apart.
- Late menopausal transition: Cycles get even farther apart, lasting 60 days or more.
- Postmenopause: This is after menopause, when a woman hasn’t had her period for 12 months or more.
Knowing these stages helps doctors manage symptoms better. It’s important to treat each woman’s experience differently, based on her own needs.
The Pathology of Menopause: Fundamental Mechanisms
Menopause is a complex process that starts with the loss of ovarian follicles. This loss affects hormone levels and overall health. The balance between the hypothalamus, pituitary gland, and ovaries is disrupted as ovarian function declines.
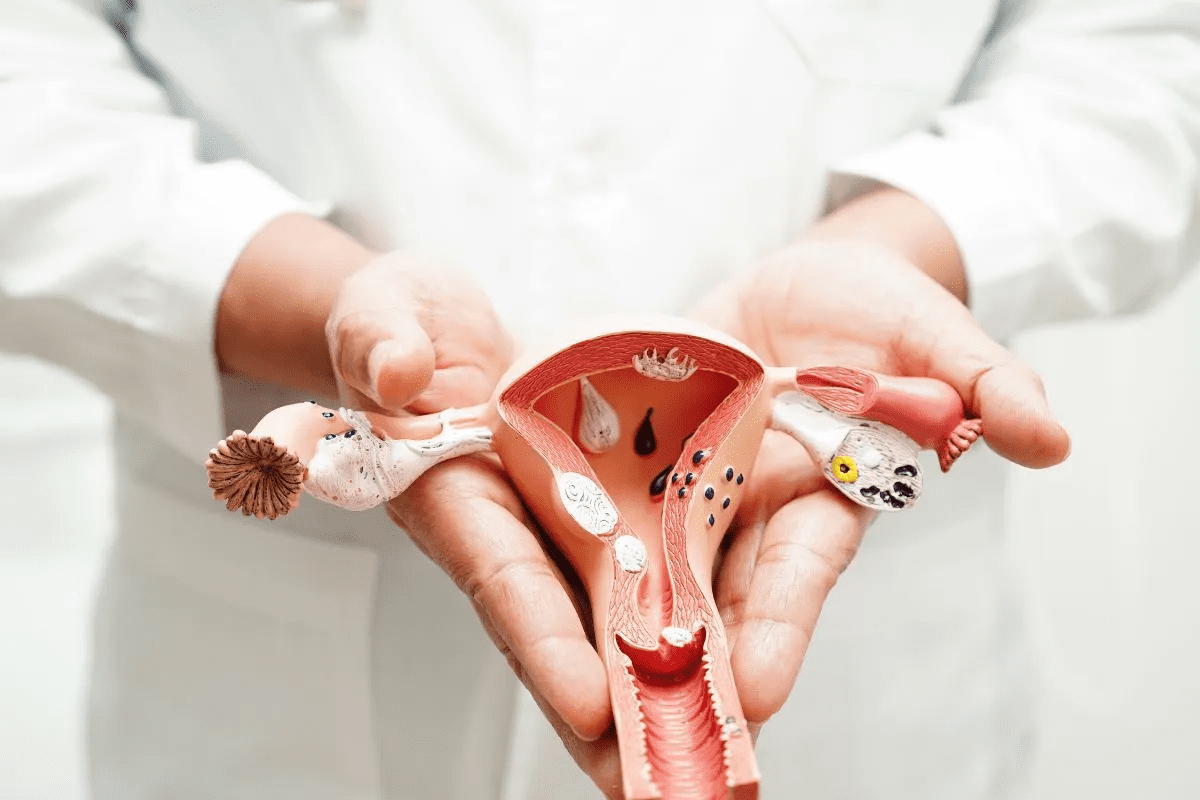
Ovarian Follicular Depletion
Ovarian follicles start to decrease in number before birth and continue to do so until menopause. This decline affects estrogen production and reproductive health. It’s a key factor in when menopause begins.
With fewer follicles, estrogen and other hormone levels drop. This change impacts the reproductive, skeletal, and cardiovascular systems. Knowing how follicular depletion works helps us understand menopause’s effects on women’s health.
Hypothalamic-Pituitary-Ovarian Axis Disruption
The HPO axis is vital for the menstrual cycle and reproductive health. When ovarian follicles decrease, the feedback loop between the hypothalamus, pituitary gland, and ovaries is disrupted. This leads to changes in hormone levels, like an increase in FSH and LH.
This disruption affects hormone balance and overall health. The drop in estrogen impacts not just reproductive health but also bone density and lipid metabolism. Understanding these changes is key to managing menopause’s health effects.
In summary, menopause is caused by the loss of ovarian follicles and disruption of the HPO axis. These mechanisms lead to hormonal changes and their effects on women’s health.
Pathophysiological Change #1: Estradiol Decline
Menopause starts with a big drop in estradiol levels. Estradiol is a key hormone that helps keep bones strong, controls body temperature, and supports heart health. As women enter menopause, lower estradiol levels cause many symptoms and health issues.
Normal vs. Menopausal Estradiol Patterns
In women before menopause, estradiol levels go up and down with their menstrual cycle. But, during menopause, this pattern changes a lot. Estradiol levels start to drop about 2 years before the last period, signaling a big hormonal change.
The drop in estradiol isn’t sudden but takes about 4 years. It levels off about 2 years after the last period. This slow drop can cause hot flashes, night sweats, and changes in bone density.
Tissue-Specific Effects of Estradiol Reduction
The drop in estradiol affects different parts of the body in different ways. For example, it can change how bones work, leading to osteoporosis or bone loss. It also affects the heart, which can impact heart health.
Parameter | Premenopausal | Menopausal Transition | Postmenopausal |
Estradiol Levels | Cyclical, peaking during ovulation | Declining, with increased variability | Low, stable levels |
Bone Density | Maintained | Beginning to decline | Significantly reduced |
Cardiovascular Health | Supported by estradiol | Potential changes due to declining estradiol | Increased risk of cardiovascular issues |
It’s important to understand how estradiol levels drop and how it affects the body during menopause. Knowing these changes helps doctors give better care and support to women going through menopause.
Pathophysiological Change #2: Gonadotropin Elevation
Menopause brings many changes to the body, including higher levels of gonadotropins like FSH and LH. These changes happen because of how the hypothalamus, pituitary gland, and ovaries work together.
FSH and LH Feedback Mechanism Alterations
When ovarian follicles run out, the feedback loop between the hypothalamus, pituitary gland, and ovaries breaks down. Normally, the ovaries make estradiol, which tells the pituitary gland to stop making FSH and LH. But as estradiol levels drop during menopause, this feedback weakens. This leads to more FSH and LH being made.
FSH levels rise a lot, which is a big sign of menopause. When FSH goes over 30 mIU/mL, it’s a clear sign of menopause.
Diagnostic Significance of FSH Levels
FSH levels are key in figuring out if someone is in menopause. High FSH levels, along with symptoms, tell doctors if someone is going through menopause. This helps doctors tell menopause apart from other conditions with similar symptoms.
In medical practice, FSH levels help confirm menopause. We use these lab values to understand a patient’s menopause status and decide on treatments.
Pathophysiological Change #3: Progesterone Dynamics
Menopause brings big changes to progesterone levels, affecting menstrual cycles and overall health. Progesterone is key for getting the uterus ready for pregnancy. As women near menopause, their progesterone levels and activity change a lot.
Anovulatory Cycles and Progesterone Decline
Menopause brings more anovulatory cycles. Anovulatory cycles are when ovulation doesn’t happen, leading to less progesterone. Normally, progesterone goes up after ovulation to get the uterus ready for pregnancy. But in anovulatory cycles, this doesn’t happen, causing lower progesterone levels.
As menopause gets closer, anovulatory cycles become more common. This leads to lower progesterone levels. This drop can affect the body in many ways, including menstrual bleeding changes.
Endometrial Effects and Bleeding Pattern Changes
Less progesterone affects the endometrium, the uterus lining. Progesterone keeps the endometrium stable, and its drop can cause irregular bleeding. Irregular bleeding patterns are common during menopause, with changes in bleeding heaviness or unpredictability.
The main effects of progesterone changes on the endometrium and bleeding include:
- Irregular menstrual cycles due to anovulatory cycles
- Changes in the heaviness or lightness of menstrual bleeding
- Unpredictable spotting or breakthrough bleeding
Knowing about these changes helps manage symptoms and keep women’s health in check during menopause. As we look into menopause’s pathophysiological changes, it’s clear that hormone level changes, like progesterone, are key to women’s health.
Pathophysiological Change #4: Androgen Balance Shifts
Menopause brings changes in androgen balance. While estrogen gets a lot of attention, androgens are also key for women’s health.
Relative Hyperandrogenism Phenomenon
Menopause sees a drop in testosterone and DHEAS levels. But, androgens to estrogens ratio goes up. This is called relative hyperandrogenism.
This change can affect libido, skin, and hair. We’ll look into these effects more below.
Clinical Manifestations of Altered Androgen Levels
Androgen level changes in menopause can cause several symptoms. These include:
- Changes in libido
- Alterations in skin and hair growth patterns
- Potential impacts on bone density
- Mood changes
The table below summarizes the key effects of androgen balance shifts during menopause:
Clinical Manifestation | Description |
Changes in Libido | Decreased libido due to altered testosterone levels |
Skin and Hair Changes | Increased facial hair, acne, or changes in skin texture |
Bone Density Effects | Potential impact on bone mineral density due to androgen level changes |
Mood Changes | Mood swings, irritability, or depression |
It’s important to understand these changes to manage menopause symptoms well. We’ll look at more changes in the next sections.
Pathophysiological Change #5: Metabolic and Inflammatory Changes
Menopause brings many changes, including shifts in how our body handles fats and inflammation. These changes can affect our heart health and increase the risk of metabolic syndrome.
Lipid Profile Alterations
Women often see changes in their cholesterol levels during menopause. This can lead to higher total and LDL cholesterol and lower HDL cholesterol. These changes raise the risk of heart disease. Monitoring lipid profiles is key to understanding heart health risks.
Inflammatory Biomarkers in Menopause
Menopause also brings changes in inflammatory markers like CRP and IL-6. High levels of these markers show more inflammation, which is linked to chronic diseases. Understanding these changes helps manage risks.
Insulin Sensitivity Changes
Menopause also affects how well the body uses insulin. Lower estrogen levels can cause insulin resistance, a step towards type 2 diabetes. Lifestyle modifications and regular checks can help manage these changes.
These metabolic and inflammatory changes are key parts of menopause. By understanding and addressing them, healthcare providers can give better care to women during this time.
Pathophysiological Change #6: Neuroendocrine Disruptions
Neuroendocrine disruptions are a key part of menopause, affecting many body functions. These changes can really impact a woman’s life, causing various symptoms that need careful handling.
Thermoregulatory Dysfunction and Hot Flashes
Hot flashes are a common and upsetting symptom of menopause. Hot flashes affect up to 80% of women during this time. They are sudden feelings of heat, often with sweating, flushing, and heart racing.
The cause of hot flashes is complex. It involves the hypothalamus, estrogen levels, and neurotransmitters like norepinephrine and serotonin. These chemicals help control body temperature and can trigger hot flashes.
Sleep-Wake Cycle Alterations
Sleep problems are common in menopause, affecting many women. These issues include insomnia, broken sleep, and poor sleep quality. Hormonal changes, hot flashes, and stress are among the causes.
Research shows that lower estrogen levels can disrupt sleep. Estrogen affects the sleep-wake cycle by influencing the hypothalamic-pituitary-adrenal axis and gene expression.
Mood and Cognitive Effects
Menopause can also lead to mood and cognitive changes. Some women feel depression, anxiety, and mood swings. They may also have trouble remembering things and focusing.
The link between menopause and mood/cognitive changes is complex. Hormonal shifts, neurotransmitter changes, and psychosocial factors all play a role. A thorough approach is needed to manage these symptoms.
Symptom | Prevalence | Possible Causes |
Hot Flashes | Up to 80% | Thermoregulatory dysfunction, hormonal changes |
Sleep Disturbances | Significant proportion | Hormonal changes, hot flashes, psychological factors |
Mood Changes | Variable | Hormonal fluctuations, neurotransmitter changes, psychosocial factors |
It’s important to understand neuroendocrine disruptions in menopause. A holistic approach, considering both physical and mental factors, is key to improving women’s lives during this time.
Pathophysiological Change #7: Bone and Calcium Metabolism
Menopause brings a big drop in estrogen levels. This affects bone density and calcium balance. These changes are key to bone health.
Calcium Homeostasis Disruption
Menopause lowers estrogen, upsetting calcium balance. Estrogen is vital for bone health. Without it, bone resorption goes up, disrupting calcium levels.
Bone Turnover Markers
Bone turnover markers show how bones are being remade. In menopause, these markers go up. Markers like C-telopeptide (CTX) and N-telopeptide (NTX) show more bone breakdown.
Accelerated Bone Mineral Density Loss
Disrupted calcium balance and more bone turnover mean faster bone loss. This is a big risk for osteoporosis and fractures. The loss is fastest right after menopause, making early action key.
Healthcare providers focus on bone health in menopause. Knowing how bones and calcium change helps us fight osteoporosis.
Conclusion: Clinical Implications and Management Considerations
We’ve looked into the changes that happen during menopause. These changes are important for women’s health. Knowing about them helps in managing and caring for women during this time.
It’s key to figure out if symptoms are from menopause or something else. This helps doctors choose the right treatment, like hormone therapy. It also helps manage other health problems.
Healthcare providers can make treatment plans that fit each woman’s needs. This approach improves her life during this big change.
FAQ
What is menopause, and at what age does it typically occur?
Menopause is when a woman’s menstrual cycle stops, usually between 45 and 55 years old.
What is the clinical definition of menopause?
It’s when a woman stops menstruating for good, confirmed after a year without a period.
What are the stages of the menopausal transition?
The menopausal transition, or perimenopause, is when hormone levels change and periods become irregular. It lasts for several years.
What is the primary cause of menopause?
Menopause happens because the ovaries run out of follicles, causing estrogen levels to drop and disrupting hormone balance.
How do estradiol levels change during menopause?
Estradiol levels drop a lot during menopause. This affects bones and heart health.
What is the significance of elevated FSH levels in menopause?
High FSH levels help doctors know if a woman is in menopause. It’s because of changes in hormone feedback loops.
How do progesterone dynamics change during menopause?
Progesterone levels go down, and periods can become irregular. This changes how often and how much women bleed.
What is relative hyperandrogenism, and how does it manifest during menopause?
Relative hyperandrogenism is when androgen levels change during menopause. It can affect sex drive and overall health.
What metabolic changes occur during menopause?
Menopause can change how the body handles fats, inflammation, and insulin. This increases the risk of heart disease and metabolic syndrome.
What are the neuroendocrine disruptions that occur during menopause?
Menopause can cause problems with body temperature, sleep, and mood. It can also affect thinking and memory.
How does menopause affect bone and calcium metabolism?
Lower estrogen levels in menopause disrupt calcium balance. This leads to faster bone loss and a higher risk of osteoporosis.
What is the definition of menopause in medical terminology?
In medical terms, menopause is when a woman stops menstruating for good. It marks the end of her reproductive years.
How do hormone levels change for menopausal women?
Menopausal women see a drop in estrogen and progesterone. FSH and LH levels go up, showing changes in hormone balance.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK507826/