Last Updated on December 1, 2025 by Bilal Hasdemir

Neuroblastoma is a cancer that starts in the adrenal glands, neck, chest, or spinal cord. It’s most often found in kids. It’s a big deal in childhood cancer research, being the top abdominal tumor in children Pediatric Abdominal Solid Tumor.
We need to understand neuroblastoma, its diagnosis, and how it affects kids. Knowing how to diagnose it is key for treatment.
Key Takeaways
- Neuroblastoma is a cancer type that mainly hits kids.
- It starts in the adrenal glands, neck, chest, or spinal cord.
- Getting to know neuroblastoma is vital for childhood cancer studies.
- Spotting it early is essential for treatment plans.
- Neuroblastoma is the most common solid tumor outside the brain in kids.
Understanding Neuroblastoma: The Most Common Pediatric Abdominal Solid Tumor
It’s key to know about neuroblastoma to spot it early and treat it well. This tough childhood cancer comes from young nerve cells. It’s aggressive and can show up in many ways.
Definition and Origin of Neuroblastoma
Neuroblastoma is a cancer that starts in neuroblasts, young nerve cells. It mostly hits babies and young kids. It often shows up in the adrenal glands, neck, chest, or spine.
The problem starts in the early stages of growth. Neural crest cells don’t grow right.
Prevalence and Epidemiology
Neuroblastoma is a big deal in kids, making up 6% of all childhood cancers. It’s found more in some places around the world. Studies show it’s more common in kids under 5, and boys get it a bit more often.
| Age Group | Incidence Rate | Gender Predominance |
| 1 in 100,000 | Male | |
| 1-4 years | 1.2 in 100,000 | Male |
| 5-9 years | 0.5 in 100,000 | Female |
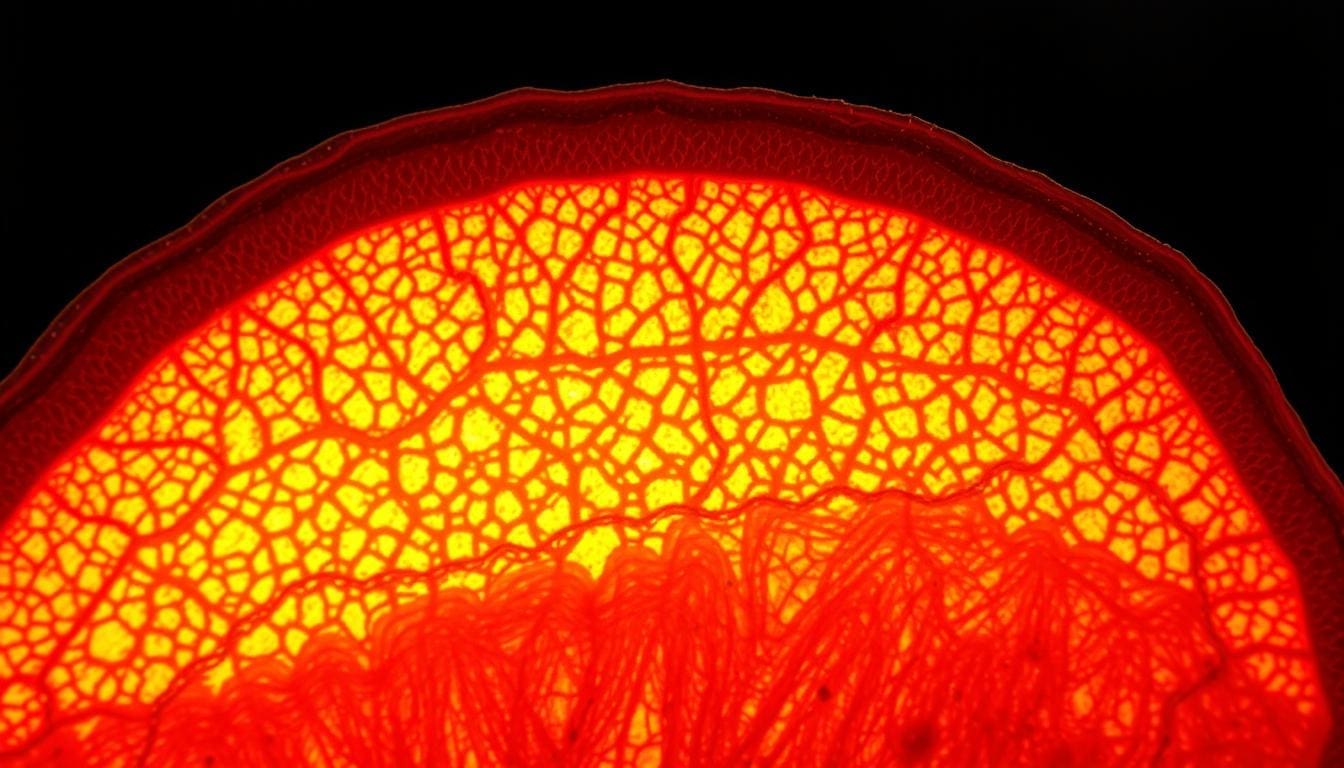
The Biology of Neuroblastoma
Neuroblastoma is a complex cancer that starts in neural crest cells. These cells are the precursors to the sympathetic nervous system. The cancer develops due to genetic mutations that disrupt normal cell function.
Cell of Origin and Development
Neuroblastoma comes from neural crest cells. These cells are important in early development and can become different types of cells. But in neuroblastoma, they grow out of control and become cancerous.
Key factors influencing neuroblastoma development include:
- Genetic mutations that affect cell growth and survival
- Epigenetic changes that alter gene expression
- Environmental factors that can affect cell behavior
Genetic Factors and Mutations
Genetics are very important in neuroblastoma. Certain genetic changes, like MYCN amplification, are linked to aggressive forms of the disease. Other changes, like ALK gene mutations, also play a role.
Knowing about these genetic changes helps doctors understand the disease better. It also guides the development of new treatments. As research grows, using genetic information in treatment plans is becoming more common.
“The genetic landscape of neuroblastoma is complex, with multiple mutations and alterations contributing to its heterogeneity. Understanding these genetic factors is critical for developing effective treatments.”
Risk Factors and Causes
Understanding the risk factors and causes of neuroblastoma is key for early detection and treatment. We look at the factors that lead to this complex disease.
Genetic Predisposition
Genetics play a big role in neuroblastoma. Certain genetic syndromes, like neurofibromatosis type 1 and Beckwith-Wiedemann syndrome, raise the risk of neuroblastoma.
Specific genetic mutations, including those in the MYCN gene, are found in neuroblastoma patients. These mutations can make the disease more aggressive and affect treatment outcomes.
Environmental Factors
Environmental factors are thought to play a role in neuroblastoma. Studies look into links between certain chemicals and radiation and neuroblastoma.
Familial Neuroblastoma
In some families, neuroblastoma runs in the genes. This rare occurrence helps us understand the disease’s genetic roots.
| Risk Factor | Description | Impact on Neuroblastoma |
| Genetic Predisposition | Presence of specific genetic syndromes or mutations | Increased risk and potentially more aggressive disease |
| Environmental Factors | Exposure to certain chemicals and radiation | Potential increased risk, though links are being researched |
| Familial History | History of neuroblastoma in close relatives | Rare, but suggests a hereditary component |
Clinical Presentation and Symptoms

It’s important to know how neuroblastoma shows up early. This helps in treating it better. Neuroblastoma can show up in many ways, making it hard to diagnose, mainly in young kids.
Common Signs in Infants
In babies, neuroblastoma often shows as a big tummy mass. This can be felt by a parent or doctor during a check-up. Early detection is key for better treatment and survival chances.
Babies might also have bulging eyes or eye bruises if the tumor spreads. These signs are scary and need quick doctor visits.
Symptoms in Older Children
In older kids, neuroblastoma symptoms are not always clear. They might feel pain in their belly, bones, or just feel tired. These signs can be mistaken for other, less serious problems, which can delay finding out what’s wrong.
Older kids might also have weakness or paralysis if the tumor presses on their spine. This is why they need to see a doctor right away.
Paraneoplastic Syndromes
Some kids with neuroblastoma have rare conditions caused by the tumor. One is opsoclonus-myoclonus syndrome (OMS). It makes their eyes and muscles move on their own. It’s important to spot these conditions to treat them quickly.
Doctors need to know how neuroblastoma can show up to diagnose it right and fast. This helps in improving cancer survival rates by starting treatment early and using the right pediatric diagnostic methods.
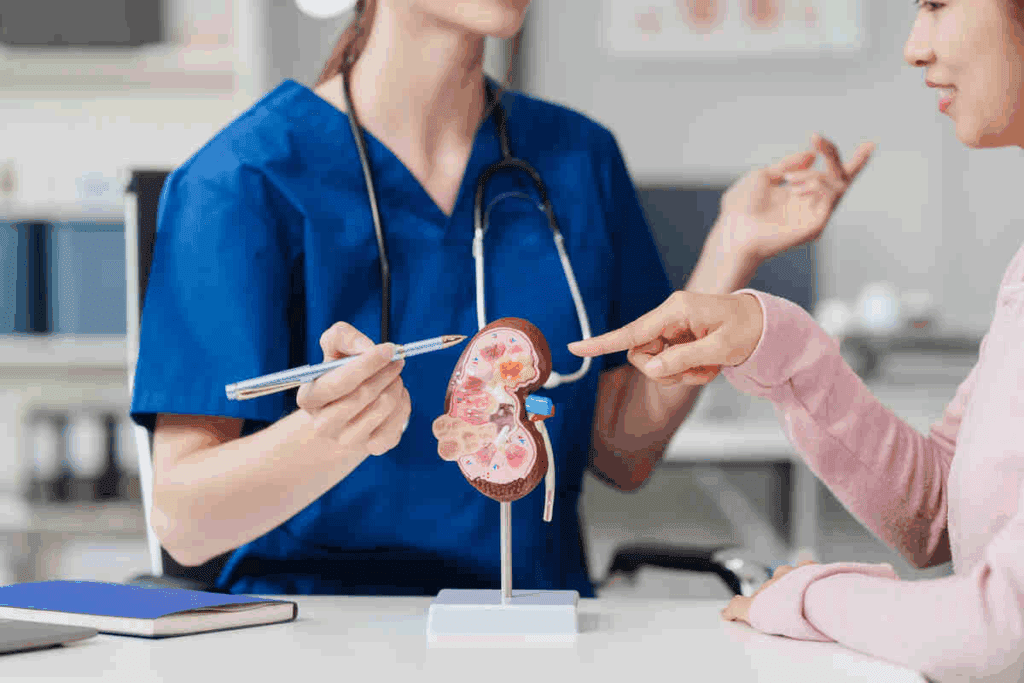
Diagnostic Approaches for Neuroblastoma
Diagnosing neuroblastoma needs a detailed plan. This includes physical exams, checking biomarkers, and using imaging. We’ll look at how these methods help find and understand this complex cancer in kids.
Initial Assessment and Physical Examination
The first step is a detailed physical check and talking about the patient’s health history. Doctors look for signs like big tumours in the belly or swelling. These could mean a tumor is present.
A careful physical check is key. It often shows the first signs of neuroblastoma. Doctors might feel for tumours in the belly or notice other signs like bulging eyes or unusual movements.
Laboratory Tests and Biomarkers
Lab tests are very important for diagnosing neuroblastoma. One key test is checking the urine for catecholamines. High levels of these substances are common in patients with neuroblastoma.
Other tests might include blood counts and liver function tests. They help see how big the tumor is and how it might affect the body.
| Laboratory Test | Purpose |
| Urinary Catecholamines | Diagnosis and monitoring of neuroblastoma |
| Blood Counts | Assess for anemia, infection, or other abnormalities |
| Lactate Dehydrogenase (LDH) | Marker of tumor burden |
Imaging Techniques
Imaging is vital for finding and understanding neuroblastoma. Common methods include ultrasound, CT scans, MRI, and MIBG scans.
Each method has its own strengths. MRI gives clear pictures of soft tissues without using X-rays. MIBG scans are great for finding neuroblastoma cells because they target cells from the neural crest.
Diagnosing neuroblastoma is a detailed process. It uses clinical checks, lab tests, and imaging. By combining these, we can accurately find and understand neuroblastoma. This helps plan the best treatment.
“The diagnosis of neuroblastoma requires a high index of suspicion and a detailed diagnostic workup, including imaging and biochemical markers.”
— Source: Pediatric Oncology Text
Advanced Diagnostic Methods
Diagnosing neuroblastoma needs advanced methods. These methods help understand the tumor’s biology and guide treatment. They also determine how far the disease has spread.
Biopsy Procedures
A biopsy is key for diagnosing neuroblastoma. Biopsy procedures take tissue from the tumor for examination. This tissue is analyzed to confirm neuroblastoma cells and assess the tumor’s characteristics.
There are several biopsy methods, like incisional, excisional, and needle biopsies. The choice depends on the tumor’s location and size, and the patient’s health.
Genetic and Molecular Testing
Genetic and molecular testing are vital in diagnosing and managing neuroblastoma. These tests find specific genetic mutations linked to the tumor. For example, MYCN amplification affects the tumor’s behavior and prognosis.
Other tests look for DNA abnormalities like deletions or gains. This information helps understand the tumor’s biology and plan treatment.
Staging and Risk Assessment
Accurate staging and risk assessment are key. They determine the disease’s extent and predict the patient’s outcome. The International Neuroblastoma Staging System (INSS) is used for staging.
Risk assessment looks at the patient’s age, tumor stage, and biological tumor characteristics. This helps categorize patients into risk groups. It guides treatment decisions and predicts prognosis.
The International Neuroblastoma Staging System
Accurate staging of neuroblastoma is key for effective treatment and prognosis. The International Neuroblastoma Staging System (INSS) and its successor, the International Neuroblastoma Risk Group Staging System (INRGSS), classify disease extent. They use clinical and radiological assessments.
Stage 1-2: Localized Disease
Stage 1 and 2 neuroblastomas are localized. They are confined to the area where they started. Stage 1 tumors are completely resectable, with no spread. Stage 2 tumors may spread to nearby lymph nodes but are mostly localized.
Stage 3-4: Advanced Disease
Stage 3 neuroblastomas are more extensive. They may cross the body’s midline or have significant lymph node involvement on the opposite side. Stage 4 indicates cancer has spread to distant parts like bones, bone marrow, or distant lymph nodes.
Stage 4S: Special Infant Category
Stage 4S is for infants under one year. They have localized primary tumors and limited dissemination to skin, liver, or minimal bone marrow. Despite spread, these infants often have a good prognosis and may not need intense treatment.
Knowing the stage of neuroblastoma helps doctors choose the best treatment. This can include surgery, chemotherapy, radiation, or a mix of these. The INSS and INRGSS staging systems help standardize disease assessment. They make it easier for healthcare providers to communicate and compare research results.
Risk Stratification in Neuroblastoma
Risk stratification in neuroblastoma helps doctors predict how well a patient will do. It also helps them choose the right treatment for each patient.
This process looks at many factors to guess how the disease will grow and how well it will respond to treatment. It’s key for making treatment plans that work best for kids.
Low-Risk Disease
Low-risk neuroblastoma is easy to treat because it’s small and can often be removed. Kids with this type usually do very well with little treatment.
Characteristics of Low-Risk Neuroblastoma:
- Localized tumor
- Favorable histology
- Absence of MYCN amplification
Intermediate-Risk Disease
Intermediate-risk neuroblastoma is more varied. It has different biology and behavior. Treatment for this type is customized based on several factors.
Key Factors in Intermediate-Risk Disease:
- Tumor stage and resectability
- Biological markers such as ploidy and MYCN status
- Patient age and overall health
High-Risk Disease
High-risk neuroblastoma is tough to treat. It’s spread out and has bad biology. Kids with this type need strong treatments like chemo, radiation, and immunotherapy.
Features of High-Risk Neuroblastoma:
| Feature | Description |
| Advanced Stage | Disease spread beyond the primary site |
| MYCN Amplification | Presence of multiple copies of the MYCN oncogene |
| Unfavorable Histology | Tumor characteristics associated with poor prognosis |
Knowing the risk level of neuroblastoma is vital for making good treatment plans. By sorting patients into low, intermediate, or high-risk groups, doctors can give the best care. This can lead to better survival rates for kids.
Treatment Approaches for Low and Intermediate Risk Patients
Treatment for low and intermediate-risk neuroblastoma patients involves several steps. These include watching the child closely, surgery, and chemotherapy when needed. We know each child is different, so we create a treatment plan that works best for them. This plan aims to be effective while also protecting against long-term side effects.
Observation Strategy
Some children with low-risk neuroblastoma might not need treatment right away. Instead, they might just be watched closely. This means regular check-ups and scans to see how the tumor is doing. Sometimes, tumors in babies can even go away on their own without treatment.
Surgical Interventions
Surgery is key in treating neuroblastoma, mainly for tumors that are in one place. For kids with low and intermediate-risk tumors, surgery is often the first step. Our goal is to remove the tumor completely without harming the surrounding tissues too much.
Deciding if surgery is needed depends on several things. These include where the tumor is, how big it is, and the child’s health. Sometimes, surgery is followed by chemotherapy to help ensure the best results.
Moderate Intensity Chemotherapy
Chemotherapy is used when the tumor has spread or might spread. For low and intermediate-risk patients, we use a specific type of chemotherapy. This type is strong enough to fight the cancer but not so strong that it causes too many side effects.
We customize the chemotherapy for each child. We consider the tumor’s type and how the child reacts to treatment. Keeping a close eye on the child and adjusting the treatment as needed is important. This helps improve the chances of a good outcome.
By using a detailed and varied treatment plan, we can help more children with low and intermediate-risk neuroblastoma. Our focus on cancer survival rates and childhood cancer treatment means we can give each child the care they need. This approach helps us tailor treatment to each child’s unique situation.
Treatment Strategies for High-Risk Neuroblastoma
High-risk neuroblastoma needs a strong treatment plan. This includes intense chemotherapy, surgery, and sometimes stem cell transplants. We will look at the different ways to treat this serious disease.
Intensive Multimodal Therapy
Intensive therapy is key for treating high-risk neuroblastoma. It combines:
- High-dose chemotherapy to kill cancer cells
- Surgical resection to remove the main tumor
- Radiation therapy to control the disease locally
The aim is to get rid of the cancer completely and stop it from coming back. We use these treatments together to attack the cancer from all sides.
Stem Cell Transplantation
Stem cell transplants are a big part of treating high-risk neuroblastoma. They let us give high-dose chemotherapy and then add stem cells to rebuild the bone marrow. There are two main types:
- Autologous stem cell transplantation, using the patient’s own stem cells
- Allogenic stem cell transplantation, using stem cells from a donor
| Treatment Aspect | Autologous Transplant | Allogenic Transplant |
| Stem Cell Source | Patient’s own cells | Donor cells |
| Graft-Versus-Host Disease Risk | Low | High |
| Treatment Intensity | High | Very High |
Immunotherapy Approaches
Immunotherapy is a new hope for treating high-risk neuroblastoma. It uses the body’s immune system to fight cancer. Some methods include:
- Monoclonal antibodies targeting neuroblastoma cells
- Checkpoint inhibitors to boost the immune response
- CAR-T cell therapy, a type of adoptive immunotherapy
These treatments are being tested in clinical trials. They show promise in helping children with high-risk neuroblastoma.
Radiation Therapy in Neuroblastoma Management
Radiation therapy is a big step forward in treating neuroblastoma in kids. It helps kill cancer cells, mainly in tough cases.
This treatment is key in fighting neuroblastoma. It’s made to fit each patient’s needs. There are two main types: External Beam Radiation Therapy and MIBG Therapy.
External Beam Radiation
External Beam Radiation Therapy (EBRT) uses a beam from outside the body to hit the tumor. It’s precise, aiming right at the tumor and sparing healthy tissues.
- Precision: EBRT fits the tumor’s exact shape and size.
- Effectiveness: It controls local disease and eases symptoms.
- Flexibility: The treatment’s dose and schedule can change based on the patient’s response and tumor details.
MIBG Therapy
MIBG (Metaiodobenzylguanidine) Therapy is a special radiation treatment for neuroblastoma. It uses a compound that cancer cells absorb, allowing for targeted radiation.
- MIBG is given through an IV and targets neuroblastoma cells.
- The radioactive part of MIBG gives a strong dose of radiation right to the tumor, protecting other parts of the body.
- This method is great for patients with high-risk or spread-out disease.
In summary, radiation therapy, including External Beam Radiation and MIBG Therapy, is essential in treating neuroblastoma. Knowing how these treatments work helps us give the best care to those with this challenging disease.
Novel and Emerging Therapies
The future of neuroblastoma treatment is bright with new therapies. Research is leading to innovative ways to fight cancer in kids. These new methods are changing how we treat pediatric cancer.
Targeted Molecular Therapies
Targeted molecular therapies are a big step forward in treating neuroblastoma. They focus on specific changes in tumor cells, aiming to protect normal cells. ALK inhibitors are showing great promise in treating certain types of neuroblastoma.
These therapies rely on genetic and molecular testing to understand tumors better. This helps doctors create treatments that fit each patient’s cancer perfectly.
Immunotherapeutic Advances
Immunotherapy is a powerful tool against neuroblastoma. It includes CAR-T cell therapy, which makes immune cells attack cancer cells better. This field is growing fast, with many trials underway to test its safety and effectiveness.
Monoclonal antibodies are also being explored. They target specific proteins on neuroblastoma cells, helping to kill them or stop them from growing. Adding immunotherapy to treatments could lead to better results for high-risk patients.
Precision Medicine Approaches
Precision medicine is changing how we treat neuroblastoma. It tailors treatments to each patient’s unique genetic and molecular profile. This involves detailed genomic testing to find specific targets for therapy.
With precision medicine, we’re moving away from one-size-fits-all treatments. As we learn more about neuroblastoma’s genetics, precision medicine will play a bigger role in improving patient care.
Current Research and Clinical Trials
Ongoing research in neuroblastoma is leading to new treatments. We’re learning more about this complex disease every day. Clinical trials are key, giving patients access to new treatments.
Promising Investigational Treatments
Several promising treatments are being tested in trials. These include new chemotherapy, targeted therapies, and immunotherapy like CAR-T cell therapy. Researchers are also exploring combination therapies.
Examples of investigational treatments include:
- New chemotherapy agents with improved efficacy and reduced toxicity
- Targeted therapies that focus on specific genetic mutations
- Immunotherapy approaches, such as CAR-T cell therapy
- Combination therapies that pair different treatment modalities
How to Access Clinical Trials
Finding clinical trials can be tricky, but help is available. Start by talking to your healthcare provider. Online platforms and registries list ongoing trials.
| Resource | Description |
| A database of privately and publicly funded clinical studies | |
| National Cancer Institute | Information on cancer clinical trials and resources |
| Pediatric Cancer Research Foundation | Support and resources for families, including information on clinical trials |
It’s vital to review trial criteria and discuss benefits and risks with your healthcare team.
Long-term Outcomes and Survival Rates
Neuroblastoma patients’ long-term outcomes depend on several factors. These include the risk category and the treatment they receive. We will look at what affects survival, survival rates by risk group, and the quality of life for survivors.
Prognostic Factors
Many factors influence a neuroblastoma patient’s long-term outcome. These include the patient’s age at diagnosis, the disease stage, and the tumor’s biological characteristics. For example, MYCN amplification and ALK mutations are important. Knowing these helps doctors predict survival and recurrence chances.
Survival Statistics by Risk Group
Survival rates for neuroblastoma vary by risk category. Low-risk patients have a high survival rate, over 95%. High-risk patients face a tougher road, but new treatments have helped improve their survival chances. We will detail the survival rates for each risk group to help understand the prognosis better.
- Low-risk: >95% survival rate
- Intermediate-risk: 80-90% survival rate
- High-risk: 50-70% survival rate, improving with newer treatments
Quality of Life Considerations
As survival rates rise, focusing on survivors’ quality of life becomes key. Survivors may face late effects from treatment, like physical disabilities and secondary cancers. We must consider these when evaluating treatment success and planning follow-up care.
Understanding neuroblastoma’s long-term outcomes and survival rates helps us support patients and their families. Our aim is to not just increase survival rates but also to improve survivors’ quality of life.
Late Effects and Long-term Follow-up
Neuroblastoma survivors need long-term follow-up to deal with late effects. These effects can affect their quality of life. As medical care gets better, more survivors are living longer. This means we need to focus on both physical and mental health challenges.
Physical Late Effects
Neuroblastoma survivors face physical late effects from their treatment. These can include:
- Hearing loss from some chemotherapy agents
- Cardiac issues from certain chemotherapies or radiation
- Endocrine problems like thyroid issues or growth problems from radiation
- Secondary cancers, a risk from radiation and some chemotherapy drugs
Early detection and management of these late effects are critical to improving the long-term health of neuroblastoma survivors.
Psychological Impact
The psychological impact on survivors should not be ignored. Going through cancer treatment can cause anxiety, depression, and PTSD. Survivors may also struggle with body image, social reintegration, and education or work.
Providing psychosocial support is key in long-term follow-up care. It helps survivors cope with these challenges and fit back into their communities.
Monitoring and Surveillance Protocols
Effective long-term follow-up means regular monitoring and surveillance. This includes:
- Regular appointments with healthcare providers
- Screening tests for early detection of late effects, like cardiac or hearing tests
- Education on healthy lifestyle choices to reduce risks
- Access to psychosocial support services
By using these protocols, healthcare providers can help survivors manage their late effects. This improves their overall quality of life.
Support Resources for Families
Dealing with neuroblastoma is tough, and families need a strong support system. This includes national groups, psychosocial services, and financial help. We know how hard it is to face a neuroblastoma diagnosis. The right resources can really help.
National Organizations and Foundations
Many national groups and foundations help families with neuroblastoma. They offer information, emotional support, and help with advocacy.
- Children’s Neuroblastoma Cancer Foundation (CNCF): Offers financial and emotional support.
- Neuroblastoma Children’s Cancer Society (NCCS): Provides financial help, emotional support, and advocacy.
- National Children’s Cancer Society (NCCS): Helps with treatment costs for children with cancer, including neuroblastoma.
Psychosocial Support Services
Psychosocial support is key for families facing neuroblastoma’s emotional and psychological effects. There are many services for emotional support, counseling, and therapy.
| Service | Description | Provider |
| Counseling | Individual and family counseling to cope with the diagnosis and treatment. | Local hospitals, cancer centers |
| Support Groups | Groups for families to share experiences and receive support from others going through similar challenges. | National organizations, local communities |
| Psychological Therapy | Therapy for children and families to manage stress, anxiety, and other emotional challenges. | Licensed therapists, child psychologists |
Financial Assistance Programs
Financial help is often needed for neuroblastoma treatment costs. There are many programs to assist with these expenses.
- Financial Assistance for Travel and Accommodation: Some organizations help with travel and accommodation costs for treatment away from home.
- Medication Assistance Programs: Programs that help with medication and treatment costs.
- Grants and Scholarships: Organizations offer grants and scholarships to help with treatment and other expenses.
We know how important a strong support system is for families with neuroblastoma. By using these resources, families can get the emotional, financial, and medical support they need during this tough time.
Conclusion
Neuroblastoma is the most common solid tumor outside the brain in kids. It’s a big challenge in treating children with cancer. We’ve looked into its biology, risk factors, how it shows up, and how to treat it.
Early detection and treatment plans that fit each child are key. This helps improve their chances of beating the disease.
Looking at childhood cancer, neuroblastoma needs a team effort. From finding out it’s there to ongoing care, it’s a long journey. New ways to treat it have given hope to many, even those with the toughest cases.
Research is vital to understand and fight neuroblastoma better. By supporting studies and giving top-notch care, we aim for better results. Our goal is to help kids and their families as much as we can.
FAQ
What is neuroblastoma, and how does it affect children?
Neuroblastoma is a cancer that starts in the adrenal glands or other areas. It’s the most common tumor in kids’ bellies. The impact depends on the child’s age and the disease’s stage.
What are the common symptoms of neuroblastoma in infants and older children?
Babies might have a lump in their belly. Older kids might feel pain, swelling, or trouble walking. Some kids may also have rare conditions caused by the tumor.
How is neuroblastoma diagnosed, and what are the diagnostic tests used?
Doctors use a physical check-up, lab tests, and imaging like ultrasound or MRI. They might also take a biopsy to confirm the cancer.
What is the International Neuroblastoma Staging System, and how does it classify the disease?
This system sorts neuroblastoma into stages. It ranges from localized (Stage 1-2) to advanced (Stage 3-4). There’s also a special stage for infants (Stage 4S).
How is risk stratification determined in neuroblastoma, and what are the different risk categories?
Doctors look at age, stage, and tumor characteristics. This helps sort patients into low-risk, intermediate-risk, or high-risk groups. This guides treatment choices.
What are the treatment approaches for low- and intermediate-risk neuroblastoma?
Low- and intermediate-risk patients might get observation, surgery, or some chemotherapy. It depends on their case.
What are the treatment strategies for high-risk neuroblastoma?
High-risk cases need strong treatments. This includes stem cell transplants and new immunotherapy methods.
What is the role of radiation therapy in neuroblastoma management?
Radiation therapy is used in some cases. It includes external beam radiation and MIBG therapy. It’s often for high-risk or relapsed cases.
What are the emerging therapies and clinical trials for neuroblastoma?
New treatments include targeted therapies and immunotherapy. Patients can find clinical trials through registries and with their doctors.
What are the long-term outcomes and survival rates for neuroblastoma patients?
Survival chances vary by risk group. Low-risk patients do better. Long-term health is affected by treatment success and late effects.
What are the late effects experienced by neuroblastoma survivors, and how are they managed?
Survivors might face physical and mental late effects. They need ongoing care to manage these effects.
What support resources are available for families dealing with neuroblastoma?
Families can find help through national groups, support services, and financial aid. These offer a wide range of care.
How can families and patients access information about neuroblastoma and its treatment?
Reliable info comes from cancer organizations, medical journals, and pediatric oncology experts. They provide accurate and helpful information.
Reference
- ScienceDirect. (2025). Abdominal and pelvic tumours in children. https://www.sciencedirect.com/science/article/abs/pii/S0263931925001073