Last Updated on November 20, 2025 by Ugurkan Demir
Understanding Childhood Leukemia
Pediatric Acute Myelogenous Leukemia (AML) is a rare and complex condition that affects children worldwide. It makes up 15-20% of childhood leukemias, making it the second most common hematologic malignancy in this population.
The incidence of AML in children is about 7 cases per million each year. Families facing a diagnosis of AML seek answers and hope. Institutions like Liv Hospital are at the forefront, combining expertise, innovation, and compassionate care to address the unique challenges of pediatric AML.

Pediatric AML is a cancer that starts in the bone marrow and quickly spreads to the blood. It can also move to other parts of the body, like the lymph nodes, liver, spleen, and brain. In boys, it can even go to the testicles.
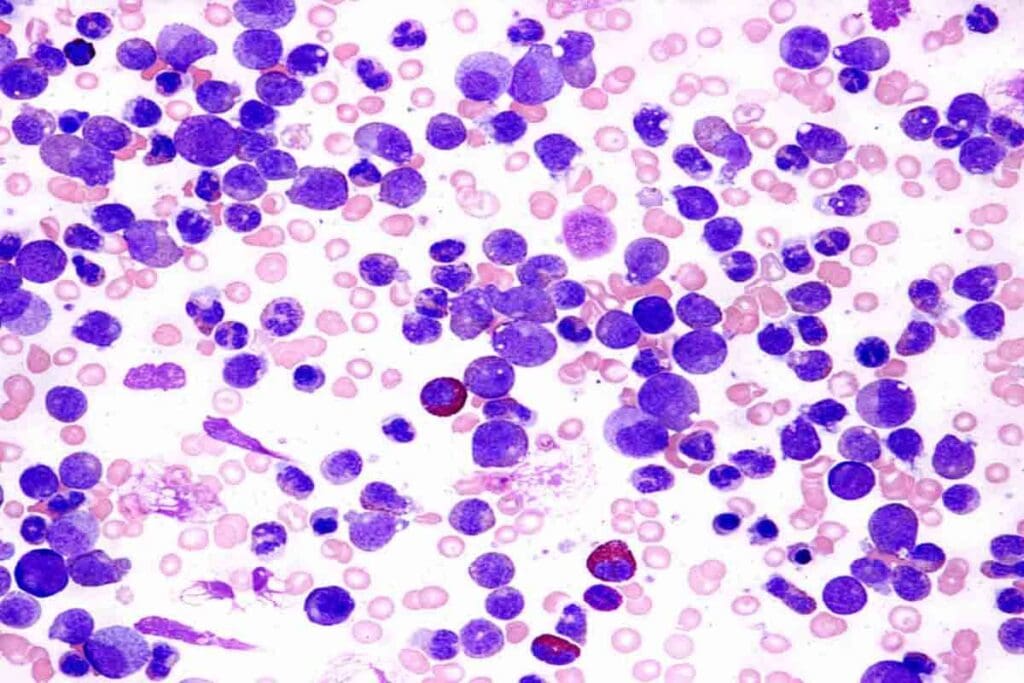
AML is a cancer caused by a bone marrow cell turning bad. This leads to a buildup of immature blood cells that don’t work properly. The National Cancer Institute says AML is diagnosed by looking at the cell’s shape, function, and genetic makeup.
AML is different from ALL because it affects myeloid cells, not lymphoid cells. The treatment and outlook for AML and ALL also differ. Experts say knowing the difference is key to choosing the right treatment and predicting how well a child will do.
| Characteristics | AML | ALL |
| Cell Lineage | Myeloid | Lymphoid |
| Common Age Group | More common in adults, but it occurs in children | Most common in children |
| Prognosis | Generally poorer than ALL in children | Higher cure rates, especially in children |
In conclusion, Pediatric AML is a serious and aggressive leukemia. It needs quick diagnosis and treatment. Knowing its unique traits is key to finding effective treatments.

Research has shown us a lot about pediatric AML. It tells us about how common it is, who gets it, and why. Pediatric AML is a big part of childhood cancers, with its own special traits.
About 7 cases of pediatric AML happen per million kids every year. This shows AML is rare in children. But it’s very serious and affects them a lot.
Pediatric AML can happen at any age in childhood. But it’s more common in some ages than others. Knowing this helps find out who’s at highest risk.
Some genetic problems increase the risk of pediatric AML. For example, kids with Down syndrome are more likely to get it. Also, having familial monosomy 7 raises the risk even more.
By knowing more about pediatric AML, doctors can do better. They can diagnose and treat it better. This helps kids with AML get better, too.
Childhood AML is a big health problem. It’s the second most common blood cancer in kids, making up 15-20% of all childhood leukemias. Knowing how common AML is in kids helps us understand its big impact on their health.
AML is the second most common blood cancer in kids, after Acute Lymphoblastic Leukemia (ALL). This shows how important AML is in treating kids with cancer.
AML makes up 15-20% of all childhood leukemias. This big number shows we need to keep learning and spreading the word about AML in kids.
Every year, about 7 kids out of a million get AML. This number shows AML is rare but very serious for the kids who get it.
To get a better idea of how common AML is in kids, let’s look at some numbers:
| Type of Leukemia | Percentage of Childhood Leukemias | Annual Incidence Rate (per million children) |
| Acute Lymphoblastic Leukemia (ALL) | 80-85% | 40-45 |
| Acute Myelogenous Leukemia (AML) | 15-20% | 7 |
This table shows how AML and ALL compare in kids. It shows their relative rates and percentages.
In short, AML is a big deal in kids’ cancers. It’s the second most common blood cancer and affects a lot of kids. We need to keep learning and spreading the word about AML.
Understanding how pediatric AML works is key to finding better treatments. Pediatric AML is when bad myeloid cells grow too much in the bone marrow and blood.
AML is known for its fast growth of bad cells. This happens because of genetic changes that help these cells grow more than normal cells. So, the bone marrow gets full of these bad cells, making it hard to make normal blood cells.
This problem with making blood cells causes symptoms like anemia and low white blood cell count. The bad cells also mess up the immune system. This makes it harder to fight off infections and can cause bleeding.
The growth of AML in kids involves many genetic and epigenetic changes. Important genes like FLT3, NPM1, and CEBPA are often changed. These changes can start pathways that help the bad cells grow and live longer, helping AML grow and spread.
The main points about how pediatric AML works are:
Pediatric Acute Myelogenous Leukemia (AML) in children shows various symptoms that need quick diagnosis and treatment. The disease affects the production of normal blood cells, causing many problems.
Children with AML often feel tired, pale, and have a fever. These signs can look like common viral infections, making it hard to diagnose early.
Common signs include bruising, petechiae, and bleeding gums. These happen because of low platelets or platelets that don’t work properly.
AML is known for high white blood cell counts. But these cells can’t fight infections well.
This makes kids with AML more likely to get serious infections. These infections can be deadly if not treated fast.
Children with AML face a higher risk of infections and bleeding. This is because their white blood cells and platelets don’t work right.
Prompt supportive care, like antibiotics and transfusions, is key to managing these risks.
Knowing the symptoms of pediatric AML is vital for early diagnosis and treatment. Healthcare providers must watch for these signs to start the right treatment quickly.
Pediatric AML has a unique genetic profile compared to adult AML. It has special karyotype patterns. Knowing these genetic features is key to diagnosing and treating childhood AML.
Pediatric AML shows specific karyotype patterns not seen in adults. These patterns include translocations and inversions. They are linked to AML in children.
About 22-26% of pediatric AML cases have normal karyotypes. This means their chromosomes look normal under the microscope. This group is fascinating for studying AML’s genetic roots.
Pediatric AML genetics are quite different from adult AML. Adult AML often has complex karyotypes and many genetic mutations. But pediatric AML has unique chromosomal translocations and fewer mutations. This affects treatment and prognosis.
In summary, childhood AML has unique genetic features like specific karyotype patterns and a high number of cases with normal karyotypes. Understanding these genetic traits is essential for creating targeted therapies. It helps improve outcomes for children with AML.
Diagnosing pediatric AML is a detailed process. It includes looking at the cells, their markers, and genes. This is key to finding the best treatment.
Here are the main steps to diagnose pediatric AML:
These steps help doctors understand the AML’s details. This guides their treatment choices.
Today’s risk systems for pediatric AML use genetics and molecular info. They sort patients into risk groups. This is vital for knowing the outlook and treatment intensity.
The systems look at several things:
Genetic testing is essential in treating pediatric AML. It finds important factors, helps classify risk, and picks targeted treatments.
Using genetic info in planning care makes treatment more tailored and effective for kids with AML.
Medical research has led to better treatment plans for pediatric AML. These plans use intensive chemotherapy, stem cell transplants, and new targeted therapies. They aim to improve patient results.
Dealing with pediatric AML requires a detailed plan. Chemotherapy is key, with plans changing based on the patient’s risk level.
Chemotherapy for kids with AML often mixes anthracyclines, cytarabine, and other drugs. The exact mix depends on the patient’s risk and how they react to treatment.
Stem cell transplants are for those with high-risk AML or who have had a relapse. It’s a chance to cure the disease by replacing the bone marrow with healthy cells.
New targeted therapies are being tested to make treatments better and safer. They target specific genes and proteins involved in AML.
| Treatment Approach | Description | Indications |
| Chemotherapy | Combination of anthracyclines, cytarabine, and other agents | Initial treatment for all patients |
| Stem Cell Transplantation | Replacement of bone marrow with healthy stem cells | High-risk disease or relapse |
| Targeted Therapies | Focus on specific molecular targets | Emerging option for improving outcomes |
Using these treatments together has greatly helped kids with AML. Research keeps going to make these plans even better. The goal is to increase survival rates and lessen side effects.
Thanks to new treatments, more kids with AML are living longer. The outlook for kids with AML is better than ever. This is due to better medical care and new ways to treat the disease.
One big win in treating AML in kids is that over 90% can reach complete remission. This means more than 90% of kids with AML can have no cancer left after treatment.
The five-year survival rate for kids with AML has also gone up. Now, about 67-68% of kids with AML can live for at least five years after being diagnosed.
Several things can change how well a kid with AML will do. These include the kid’s age, the type of leukemia, and how well they respond to treatment. Knowing these helps doctors plan the best treatment.
Even with progress, dealing with relapse is a big challenge in AML treatment. Relapse happens when the leukemia comes back after treatment. It means kids need more treatment to fight it again.
| Prognostic Factor | Impact on Survival |
| Age at Diagnosis | Younger patients tend to have better outcomes |
| Genetic Characteristics | Certain genetic features can significantly affect prognosis |
| Response to Initial Treatment | Rapid response is associated with better long-term outcomes |
Recent breakthroughs in genetics and risk classification have greatly improved the outlook for kids with Acute Myelogenous Leukemia (AML). This new understanding helps doctors create more effective treatment plans.
Thanks to these advances, kids with AML are now doing much better. They have a high chance of going into complete remission, with survival rates reaching 67-68% after five years. Researchers are working hard to make these results even better by finding new treatments and improving current ones.
The future of AML research looks bright. It will focus on better risk classification, more effective treatments, and improving long-term results. The outlook for kids with AML keeps getting better as scientists and doctors collaborate to make progress.
As we learn more about pediatric AML, treatments will likely become more tailored to each child. This personalized approach will lead to even better outcomes for kids with this disease.
Pediatric AML is a cancer that affects kids’ blood and bone marrow. It happens when abnormal cells build up too fast. This can stop normal blood cells from being made.
AML is a common childhood cancer, making up 15-20% of all leukemias in kids. It happens in about 7 cases per million children each year.
Kids with genetic conditions like Down syndrome are at higher risk. Exposure to certain toxins can also increase the risk. Some cases are linked to inherited genetic mutations.
Doctors use physical exams, lab tests, and bone marrow biopsies to diagnose AML. They also do genetic tests to find specific mutations and classify the disease.
Treatment often includes chemotherapy. Sometimes, stem cell transplantation is needed. New targeted therapies are also being tested.
Modern treatments have high success rates, with over 90% of kids achieving complete remission. Five-year survival rates are 67-68%. But, the outcome can depend on genetic factors and treatment response.
Pediatric AML has unique genetic and clinical features. It often has different genetic mutations and presents differently in kids than in adults.
Managing AML in kids is tough due to relapse risks and treatment side effects. Long-term care is also needed. Research aims to improve outcomes and reduce complications.
Genetic testing is key for diagnosing and treating pediatric AML. It helps identify mutations that guide treatment and risk assessment.
Yes, new targeted therapies and improved treatments are being developed. These aim to achieve better outcomes and reduce side effects.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!