Cancer in children is rare and very sad. Kids get different cancers than adults, and they often get better faster. The word “pediatric” comes from the Greek. It means “child” and “doctor” or “healer.”
Kids’ cancers, or “pediatric cancers,” are not like adults’. Knowing what “pediatric” means helps us understand these cancers better.
Key Takeaways
- Pediatric cancer refers to cancers occurring in children.
- These cancers are different from those affecting adults.
- The term “pediatric” relates to the medical care of children.
- Children generally have better treatment outcomes than adults.
- Pediatric cancers are rare but require specialized care.
Pediatric Meaning: Understanding the Term in Medicine
The word “pediatric” comes from Greek. It’s key to understanding pediatric medicine. It combines “pais,” meaning child, and “iatros,” meaning doctor or healer.
Etymology and Historical Development of “Pediatric”
The term “pediatric” comes from “pais” (child) and “iatros” (doctor or healer). This forms “pediatrics,” the study of children’s health. Over time, pediatric care has grown a lot.
It started with a focus on high infant death rates and diseases. Now, it includes preventive care and treating many conditions in kids.
This change shows a deeper understanding of child health. It also shows how medical science and society’s views on children’s health have evolved.
Age Range Definitions in Pediatric Medicine
Pediatric medicine covers a wide age range. It goes from birth to 18 years old. Some doctors even care for young adults.
Knowing the needs of each age group is vital. It helps in diagnosing and treating children’s health issues.
Differences Between Pediatric and Adult Medicine
Pediatric medicine is very different from adult medicine. Children are not just small adults. Their bodies are developing, which changes how they get sick and respond to treatments.
There are big differences. For example, children need special doses of medicine. Their developmental stages also play a big role in diagnosis and treatment.
Defining Pediatric Cancer: An Overview

Pediatric cancer is not just one disease. It’s a group of cancers that kids get. These include leukemia, brain tumors, and more. Each type has its own treatment and outlook.
How Childhood Cancer Differs from Adult Cancer
Childhood cancer is very different from adult cancer. Pediatric cancers grow and spread in unique ways. They need special treatments that adults don’t.
Adult cancers are often carcinomas. But kids get leukemias, lymphomas, and sarcomas. This makes treatment plans different.
Terminology Used in Pediatric Oncology
Pediatric oncology uses special words for childhood cancer. Terms like “remission” and “relapse” are used. These words help explain a patient’s cancer status.
Knowing these terms helps patients and families understand cancer care better.
The Role of Pediatric Oncologists
Pediatric oncologists are experts in childhood cancers. They work with a team to treat kids. This includes chemotherapy and surgery.
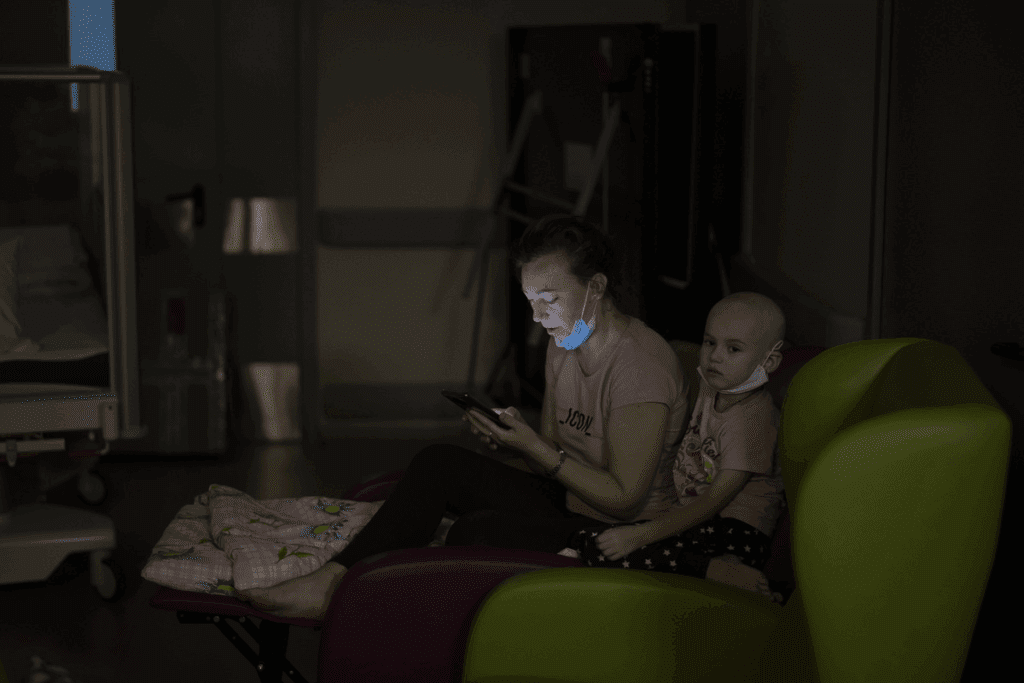
They also support patients and families emotionally. They guide them through the cancer journey.
Common Types of Pediatric Cancer
It’s key to know the different types of pediatric cancer to improve treatment plans and survival rates. Pediatric cancer includes various malignancies that differ from adult cancers in both types and treatment responses.
Leukemias in Children
Leukemia is the most common cancer in kids, making up about 30% of childhood cancers. It affects the blood and bone marrow.
Acute Lymphoblastic Leukemia (ALL)
ALL is the top leukemia type in kids, marked by the fast growth of immature white blood cells. Most children with ALL go into remission thanks to effective treatment.
Acute Myeloid Leukemia (AML)
AML is a less common leukemia in kids, but it’s serious. It’s about abnormal cells growing fast in the bone marrow.
Brain and Central Nervous System Tumors
Brain and CNS tumors are the second most common in kids. These tumors can be benign or malignant, with varying severity.
Medulloblastoma
Medulloblastoma starts in the cerebellum and is common in children. It needs aggressive treatment, including surgery, chemotherapy, and radiation.
Gliomas and Other CNS Tumors
Gliomas come from brain glial cells. Other CNS tumors include ependymomas and PNETs, each with unique features and treatment challenges.
Solid Tumors in Pediatric Patients
Solid tumors include neuroblastoma, Wilms tumor, rhabdomyosarcoma, osteosarcoma, and Ewing sarcoma. Each cancer has its own treatment needs.
Neuroblastoma
Neuroblastoma comes from immature nerve cells, often in the adrenal glands, neck, or chest.
Wilms Tumor
Wilms tumor is a kidney cancer mostly found in young children, often before age 5.
Rhabdomyosarcoma
Rhabdomyosarcoma is a soft tissue cancer that can appear anywhere in the body, as a swelling or mass.
Osteosarcoma and Ewing Sarcoma
Osteosarcoma is a bone cancer that makes immature bone. Ewing sarcoma is a very aggressive tumor that can be in bones or soft tissues. Both need strong treatment, like chemotherapy and surgery.
As the National Cancer Institute says, “Knowing the exact cancer type in a child is key to the best treatment.”
This highlights the need for accurate diagnosis and personalized treatment plans in pediatric oncology.
Incidence and Prevalence of Pediatric Cancer
It’s important to know how common pediatric cancer is to help kids and their families. The National Cancer Institute says about 1 in 285 kids will get cancer before they turn 20.
Statistical Overview of Childhood Cancer in the United States
Looking at childhood cancer in the U.S. gives us important information. The National Cancer Institute and the Surveillance, Epidemiology, and End Results (SEER) program tell us there are about 11,000 new cases each year.
The most common cancers in kids are leukemias, brain tumors, and solid tumors like neuroblastoma. These cancers make up a big part of all pediatric cancer cases.
Age Distribution and Demographic Patterns
Pediatric cancer happens more in some age groups than others. For example, acute lymphoblastic leukemia (ALL) is most common in kids aged 2-5. Brain tumors can happen at any age but are more common in younger kids.
- Age-specific incidence: Certain cancers are more prevalent in specific age groups.
- Demographic variations: Differences in incidence are observed across different ethnic and racial groups.
Risk Factors and Genetic Considerations
Some causes of pediatric cancer are not fully understood. But we know that genetic conditions and environmental exposures can increase the risk. For example, kids with Down syndrome are more likely to get certain leukemias.
Other risk factors include ionizing radiation and genetic mutations passed down in families. Knowing these risk factors helps us find cancer early and maybe even prevent it.
Diagnosis and Classification of Pediatric Cancers
Diagnosing pediatric cancer requires a mix of clinical checks, imaging, and lab tests. Early detection is key for better treatment and results.
Early Warning Signs and Symptoms
Spotting early signs of pediatric cancer is vital for quick medical help. Look out for unexplained weight loss, persistent fatigue, bone pain, and neurological symptoms. Knowing these signs helps in early diagnosis.
“The earlier the diagnosis, the better the chances for effective treatment and survival.” — A statement reflecting the importance of early detection in pediatric cancer.
Diagnostic Procedures and Testing
Diagnosing pediatric cancer involves many tests. These help confirm the cancer’s presence and type.
Imaging Studies
Imaging like X-rays, CT scans, MRI scans, and PET scans show the tumor’s size and location. They’re key for cancer staging.
Laboratory Tests and Biopsies
Lab tests and biopsies are vital for diagnosing cancer. Biopsies check tissue samples for cancer cells.
Genetic and Molecular Testing
Genetic and molecular tests reveal the tumor’s genetic makeup. This info helps choose the right treatment.
Staging and Classification Systems
After diagnosis, cancer is staged and classified. This shows how far the disease has spread. The system depends on the cancer type.
Knowing the cancer’s stage and type is essential. It helps doctors plan the best treatment and predict how well it will work.
Treatment Approaches for Pediatric Cancer
Effective treatment for pediatric cancer needs a detailed plan. It must include many different methods. The plan must consider the cancer type, its stage, and the patient’s needs.
Standard Treatment Protocols
Standard treatments for pediatric cancer often combine several therapies. These may include:
Chemotherapy Regimens
Chemotherapy is key in treating many pediatric cancers. It uses drugs to kill cancer cells.
Radiation Therapy
Radiation therapy uses high-energy rays to kill cancer cells. It’s often used with chemotherapy.
Surgical Interventions
Surgery is vital for some pediatric cancers. It aims to remove tumors and affected tissues.
Emerging Therapies and Clinical Trials
New treatments and clinical trials bring hope to pediatric cancer patients. These include:
Immunotherapy
Immunotherapy uses the immune system to fight cancer. Treatments like CAR-T cell therapy are showing great promise.
Targeted Therapies
Targeted therapies aim at specific molecules in cancer growth. They offer a more precise treatment option.
Precision Medicine Approaches
Precision medicine tailors treatment to the patient’s cancer genetics. It provides personalized care.
Multidisciplinary Care Teams
Pediatric cancer treatment works best with a team of experts. This team includes oncologists, surgeons, radiation oncologists, nurses, and support staff. They all work together for complete care.
Using different treatments and teamwork are key to better outcomes for children with cancer.
Long-term Effects and Survivorship
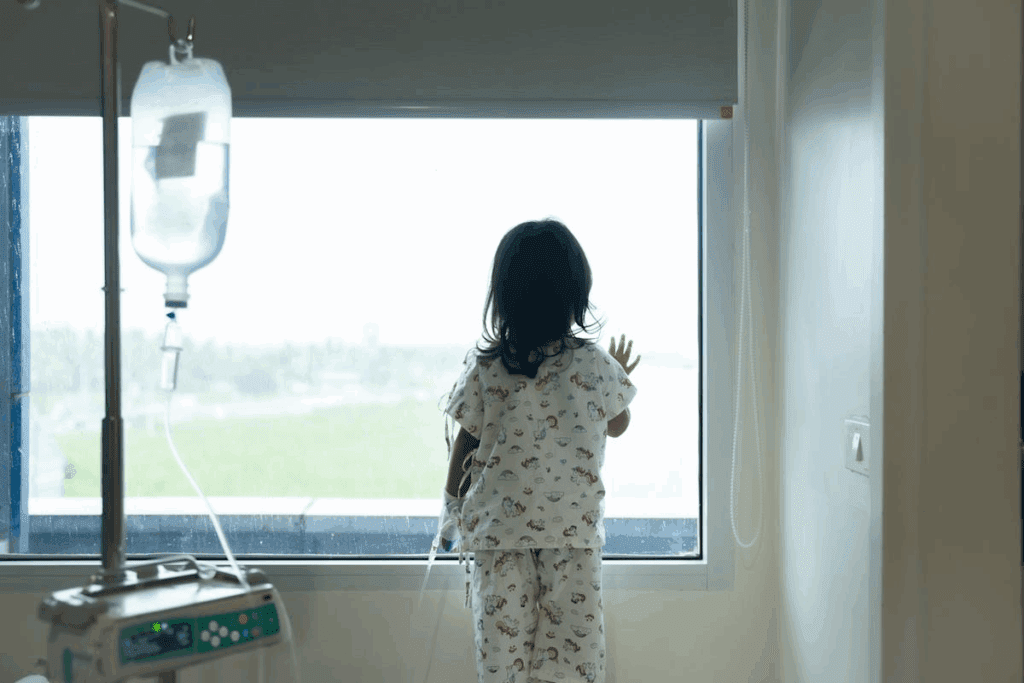
Pediatric cancer survivors face many challenges after treatment. With better survival rates, we now focus on the long-term effects of treatment.
Late Effects of Pediatric Cancer Treatment
Pediatric cancer treatment can have lasting effects. These effects fall into several categories:
Physical Late Effects
Physical effects include growth issues, organ problems, and higher cancer risks. For example, radiation can cause bone growth problems, leading to scoliosis or other skeletal issues.
Cognitive and Psychological Effects
Cognitive and psychological effects can greatly affect a survivor’s life. These may include learning disabilities, anxiety, depression, and PTSD. The emotional impact of cancer treatment is significant.
Secondary Malignancies
Developing new cancers is a major concern. Survivors of pediatric cancer are at higher risk of new cancers due to their initial treatment.
Survivorship Care Plans and Follow-up
Creating personalized care plans is key for survivors. These plans outline follow-up care, including screenings for late effects and secondary malignancies. Regular check-ups with healthcare providers are vital for early detection and management.
Quality of Life Considerations
Improving survivors’ quality of life requires a broad approach. This includes medical care, psychological support, educational help, and vocational guidance. By addressing these areas, survivors can live more fulfilling lives.
As we improve pediatric cancer treatment, we must also focus on long-term care. This ensures survivors get the support and resources they need to thrive.
Support Resources for Families Affected by Pediatric Cancer
When a family finds out their child has pediatric cancer, it can feel overwhelming. But, there are many support resources to help them through it. These resources offer help, guidance, and comfort during treatment and after.
National Organizations and Support Groups
Many national organizations support families with pediatric cancer. They offer emotional support, educational materials, and help with advocacy.
American Childhood Cancer Organization
The American Childhood Cancer Organization (ACCO) helps families a lot. They offer counseling, financial help, and advocacy. They say, “Our mission is to help families navigate the journey of childhood cancer diagnosis, treatment, and survivorship.”
Children’s Oncology Group
The Children’s Oncology Group (COG) is the biggest group for pediatric cancer research. They give info on clinical trials and treatment options. This helps families make good choices for their child’s care.
Financial Support Services
Financial help is key for families with pediatric cancer. Organizations offer different kinds of financial support. This includes help with travel, lodging, and medical costs.
“The financial burden of pediatric cancer can be overwhelming. Organizations that offer financial support services are critical in helping families navigate these challenges.”
Psychosocial Support for Patients and Families
Psychosocial support is very important for families with pediatric cancer. It includes counseling, psychological services, and support groups. These are designed to help families deal with the emotional and psychological effects of the diagnosis and treatment.
By using these support resources, families can get the help they need. This makes it easier to face the challenges of pediatric cancer.
Conclusion
Understanding pediatric cancer is key to early detection and effective treatment. This article has covered the main types of pediatric cancer. These include leukemias, brain and central nervous system tumors, and solid tumors.
Diagnosing and classifying pediatric cancers involves several steps. These include diagnostic procedures and testing, followed by staging and classification systems. Treatment options include standard protocols, emerging therapies, and clinical trials. These are managed by teams of experts.
Families dealing with pediatric cancer need a lot of support. This includes help from national organizations and support groups. They also need financial and psychosocial support for both patients and families. It’s important to consider the long-term effects of treatment and the quality of life.
In summary, pediatric cancer is a complex disease that needs a detailed approach. By understanding its diagnosis, treatment, and support, we can improve outcomes for children. This will enhance their quality of life and summarize the key aspects of their care.
FAQ
What is pediatric cancer?
Pediatric cancer is cancer that happens in kids. It’s different from adult cancers and needs special care from pediatric oncologists.
What does “pediatric” mean?
“Pediatric” means related to children’s health. It covers the care of babies, kids, and teens up to 18 or 21.
What is the age range for pediatric medicine?
Pediatric medicine covers kids from birth to 18 or 21. This age range depends on the definition used.
How does pediatric cancer differ from adult cancer?
Pediatric cancer is different in types, biology, and treatment. Kids’ cancers are often more aggressive but respond well to treatment.
What are the most common types of pediatric cancer?
Common pediatric cancers include leukemias, brain tumors, and solid tumors like neuroblastoma and Wilms tumor.
What is the role of a pediatric oncologist?
Pediatric oncologists diagnose and treat kids with cancer. They work with a team to give full care to patients.
How is pediatric cancer diagnosed?
Doctors use physical exams, imaging, and lab tests like biopsies and blood tests to diagnose pediatric cancer.
What are the treatment approaches for pediatric cancer?
Treatments include chemotherapy, radiation, and surgery. New therapies and trials are also available.
What are the long-term effects of pediatric cancer treatment?
Treatment can cause late effects like organ damage and secondary cancers. It can also affect a child’s emotional and psychological health.
What support resources are available to families affected by pediatric cancer?
Families can find help from national groups, support services, and financial aid. These resources help with the challenges of pediatric cancer.
What is a survivorship care plan?
A survivorship care plan is a plan for a child cancer survivor. It includes follow-up care and support for late effects and emotional health.
References
Siegel, R. L., & Miller, K. D. (2025). Cancer statistics, 2025. CA: A Cancer Journal for Clinicians, 75(1), 7-33. Retrieved from https://pubmed.ncbi.nlm.nih.gov/39817679/

