Pediatric Neurology: Conditions, Symptoms, and When to See a Specialist
Pediatric neurology focuses on the diagnosis and treatment of nervous system conditions in infants, children, and adolescents. If your child has frequent headaches, unexplained spells, developmental delays, seizures, movement issues, or learning and behavior changes, a pediatric neurology evaluation can help you find answers and a clear care plan. Parents often seek pediatric neurology care because they need a trusted, family centered resource that explains symptoms in plain language and offers practical next steps. Clear guidance helps families understand whether symptoms might be related to epilepsy, migraine, tic disorders, neuromuscular weakness, or functional neurological disorder.

Children’s nervous systems are still developing, so their symptoms often look different from adults. Early diagnosis and treatment can improve outcomes and quality of life. In this article, we explain common pediatric neurological disorders, what to expect during a neurological exam, and how to handle referrals, testing, and treatment options. This information can help you feel confident when advocating for your child. It’s also important to know the warning signs and when to seek urgent help, especially for a first seizure, severe headache, sudden weakness, or loss of skills.
Pediatric Neurology Near Me: How to Choose the Right Clinic for Your Child
Choosing a pediatric neurology clinic is about more than convenience. Consider:
- Experience with your child’s symptoms: headache, epilepsy, tics, developmental delay, or neuromuscular concerns.
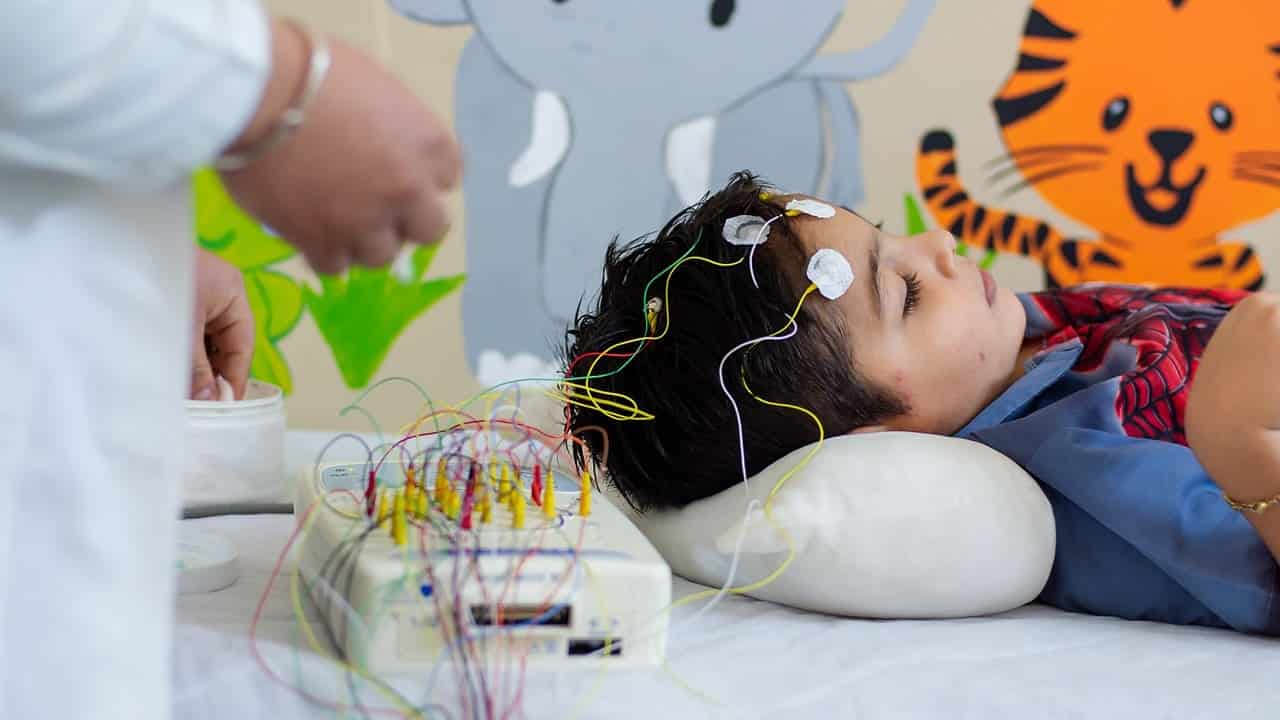
- Access to diagnostic tools: EEG for seizures, MRI when needed, and age appropriate pediatric neurological examination.
- Coordinated care: a team that can involve sleep medicine, neuropsychology, physical therapy, and behavioral health as needed.
- Family centered communication: clear explanations, written plans, and follow up support.
- Practical access: appointment availability, communication portals, and a child friendly environment.
What to bring to your first visit:
- A symptom diary (dates, duration, triggers, what helped).
- Video clips of events (staring spells, unusual movements, nocturnal behaviors).
- Medication list, allergies, and previous test results.
- Birth and developmental history, school observations, and any prior therapy reports.
A clinic with coordinated care and a welcoming environment helps children feel at ease and gives parents clear guidance. You can ask about EEG testing, how urgent symptoms are handled, and if the team offers written action plans for seizures or headaches to help you make your choice.

Pediatric Neurological Disorders: Most Common Conditions Explained for Parents

Parents commonly ask about these conditions:
- Epilepsy and seizures: Unprovoked seizures, febrile seizures, absence spells, focal seizures. Signs include staring, unresponsiveness, jerking, sudden falls, or confusion after events. Not every spell is epileptic, so careful history and EEG review matter.
- Headache and migraine: Throbbing pain, light/sound sensitivity, nausea, or dizziness. Triggers can include stress, dehydration, skipped meals, sleep loss, or screen overuse. Keeping a diary helps identify patterns and preventive strategies.
- Tic disorders and Tourette syndrome: Sudden, repetitive movements or sounds (blinking, throat clearing). Often wax and wane; stress can increase tics. Behavioral strategies and reassurance are often helpful.
- Developmental delay and regression: Delays in motor skills, language, or social milestones; loss of previously gained skills requires urgent evaluation.
- Neuromuscular concerns: Low muscle tone (hypotonia), weakness, frequent falls, trouble climbing stairs, or fatigue.
- Functional neurological disorder (FND): Real symptoms (weakness, tremor, non epileptic spells) linked to nervous system function rather than structural damage. Requires careful diagnosis and rehabilitation focused care.
- Sleep related issues and neurological symptoms: Nighttime events can be seizures, parasomnias, or sleep apnea; sleep quality affects headaches, mood, and attention.
Some warning signs mean your child should see a pediatric neurologist quickly. These include a first seizure, the worst headache your child has ever had, headaches with morning vomiting, sudden loss of speech or movement skills, ongoing weakness or changes in walking, and fainting that leads to injury or long confusion. Getting help early can lower risks and lead to better treatment.
Pediatric Neurology Center: What to Expect at Your Child’s First Visit
Your first appointment starts with a detailed history. The pediatric neurologist will ask about symptoms, triggers, sleep patterns, school functioning, and family history. A pediatric neurological examination is gentle and play-based for younger children and structured for teens.
It evaluates:
• Alertness, attention, and memory appropriate to age.
• Eye movements, vision, facial strength, and sensation.
• Muscle tone, strength, reflexes, coordination, and gait.
• Sensory responses and balance.
Possible tests:
• EEG (electroencephalogram): Looks for patterns that suggest a seizure tendency. Often used when epilepsy is suspected.
• MRI brain or spine: Ordered selectively based on exam findings, headache red flags, seizures with focal signs, or developmental regression.

• Blood tests or genetic testing: Considered when there are metabolic, neuromuscular, or inherited concerns.
• Sleep study: For snoring, daytime sleepiness, nighttime events, or suspected sleep apnea.
Care plans are personalized. Many conditions improve with a mix of lifestyle changes, therapy, and, when needed, medication or procedures. Your team will review risks and benefits and agree on concrete steps and follow-up timing. Families receive clear instructions for home and school, including seizure action plans or headache strategies.
Pediatric Neurology and Epilepsy: Recognizing Seizures and Getting Help
Not every spell is a seizure, but it’s important to capture details. Seizures can look like:
• Staring with unresponsiveness (often brief, repeated episodes).
• Rhythmic jerking of one side or both sides.
• Sudden loss of tone (drop attacks), falls, or head drops.
• Confusion, sleepiness, or headache after an episode.
What to do if your child has a seizure:
• Stay calm, time the event, and keep your child safe from injury.
• Place your child on their side if possible; do not place anything in the mouth.
• Call emergency services if a seizure lasts more than 5 minutes, if there are repeated seizures without recovery, or if breathing is impaired.
Diagnosis and treatment:
• An EEG can help confirm seizure tendency and seizure type.
• MRI may be considered based on history and exam.
• Treatment options include antiseizure medications, home seizure action plans, sleep optimization, and avoidance of personal triggers (fever, missed doses, sleep loss).
Many children outgrow certain seizure types or achieve seizure freedom with appropriate care.
Pediatric Neurological Examination: How Doctors Evaluate the Nervous System in Children
A child friendly neurological exam blends observation and play with medical assessment:
- Developmental screening: age appropriate speech, motor, and social milestones.
- Cranial nerves: tracking toys with the eyes, making faces, checking hearing, and gag reflex when appropriate.
- Motor system: muscle tone (floppy or stiff), strength (pushing and pulling games), endurance (jumping, hopping), and fine motor (pincer grasp, drawing).
- Reflexes: gentle taps to assess nerve pathways.
- Coordination and gait: heel to toe walking, finger to nose, balance tasks.
- Sensory testing: light touch and vibration as appropriate for age.
The exam helps doctors decide if your child needs imaging or other tests, which can prevent unnecessary procedures. It also shows which therapies, like physical, occupational, or speech therapy, could best support your child’s development.
Pediatric Headache and Migraine in Children: Signs, Triggers, and Treatment Options

Migraine can affect children as young as preschool age. Symptoms include moderate to severe headache, nausea, sensitivity to light or sound, abdominal pain, dizziness, and, sometimes, an aura (visual changes or tingling) before the headache. Early recognition allows families to implement routines that reduce frequency and intensity.
Common triggers:
- Irregular sleep or late nights.
- Dehydration and skipped meals.
- Stress, anxiety, or school workload.
- Screen time and eye strain.
- Specific foods in some children.
Home strategies that help:
- Regular sleep schedule (age appropriate total hours).
- Hydration (water goal by weight/age; your clinician can guide).
- Balanced meals and protein at breakfast.
- Limiting ultra processed snacks and excessive caffeine in teens.
- Breaks from screens and consistent physical activity.
Treatment options:
- Acute pain relief with age appropriate medications as directed by your clinician.
- Preventive strategies (sleep hygiene, hydration, stress management).
- For frequent or disabling migraines, your clinician may consider preventive medications, supplements, or behavioral therapy.
- Headache diary to track triggers and response to treatments.
Parents should seek prompt care for red flag headaches, including new severe headache with fever or neck stiffness, morning vomiting, or neurological changes such as weakness or vision loss.
Pediatric Neurology and Sleep: Why Sleep Matters for Seizures, ADHD, and Headaches

Sleep is central to brain health. Poor sleep can increase seizure risk, worsen headaches, and affect attention and mood. Signs of sleep problems include snoring, breathing pauses, frequent night waking, restless legs, and daytime sleepiness or irritability. Nighttime events may resemble seizures, and careful evaluation helps distinguish parasomnias from epileptic episodes.
What helps:
- Consistent bedtime and wake time, even on weekends.
- Wind down routine without screens 60–90 minutes before bed.
- Cool, dark, quiet sleep environment.
- Address nasal allergies or congestion that may affect sleep quality.
- Discuss sleep studies if there are pauses in breathing, gasping, or nightly events that could be seizures.
Better sleep can often reduce headaches, improve mood, and help your child focus during the day. That’s why sleep is an important part of many pediatric neurology care plans.
Pediatric Functional Neurological Disorder: Symptoms, Diagnosis, and Care

Functional neurological disorder (FND) in children can present with real and distressing symptoms such as weakness, tremor, gait problems, non epileptic episodes, or sensory changes. FND is a problem in how the brain functions and processes signals, not a sign of permanent damage.
Diagnosis:
- Careful history, observation, neurological examination, and appropriate testing to rule in functional features and rule out other causes.
- Video and EEG can help distinguish non epileptic events from epileptic seizures.
Care approach:
- Education for families to reduce fear and stigma.
- Rehabilitation focus: physical and occupational therapy to retrain movement patterns.
- Psychological support to address stress, anxiety, or chronic pain cycles.
- School collaboration to support a gradual return to activities.
With a clear plan, many children make strong progress. Parents can help by supporting new skills at home, keeping routines steady, and celebrating each small step forward.
Pediatric Neurology Specialists: Multidisciplinary Care and Family Support
Children benefit from a coordinated team:
- Pediatric neurologist: leads diagnosis and medical management.
- EEG and sleep technicians: support testing and monitoring.
- Therapists (physical, occupational, speech): build strength, coordination, and skills.
- Behavioral health: strategies for anxiety, tics, pain, or adherence.
- Nutrition: headache prevention, growth, and energy.
- Care coordinators: scheduling, school forms, and seizure or headache action plans.
Family centered care includes clear communication, shared decisions, and written plans you can use at home and at school. Follow up visits help track your child’s progress and update the plan as needed. You can prepare by keeping a symptom diary, noting sleep and hydration, recording videos of events when safe, and bringing school feedback to appointments.
When to Seek Urgent Care vs. a Routine Appointment
Urgent:
- A seizure lasting more than 5 minutes.
- Repeated seizures without full recovery.
- Severe head injury with loss of consciousness or worsening symptoms.
- Sudden weakness, difficulty speaking, or facial droop.
- Severe headache with neck stiffness, fever, or persistent vomiting.
Routine (soon):
- Recurrent headaches affecting school or activities.
- New spells of staring, falls, or unusual movements.
- Developmental regression or loss of skills.
- Persistent tics with distress or impairment.
- Low tone, weakness, or frequent falls.
Knowing when to seek urgent care and when to schedule a routine visit helps families respond quickly when needed and plan regular care when things are stable.
Pediatric Neurology at Liv Hospital
Liv Hospital deals with diagnosis and treatment of many neurological diseases such as neurological follow up of premature babies and babies at risk, eclampsia, developmental disorders, fainting, walking and behavioral disorders, brain traumas, headache, epilepsy, autism, muscle and nerve injuries, stroke.
In patients in infancy and all childhood periods, EEG records can be performed according to modern standards and is evaluated by a pediatric neurology specialist. In addition, brain tomography and MRI can be performed on children of any age.
A child as an organism is a whole, diseases belonging to other systems and organs can also affect the development and functions of a child’s nervous system. Urgent neurological problems are also not uncommon in children; coma, paralysis, seizures with or without fever are the most common neurological emergencies in children. These urgent neurological problems can cause permanent damage, even lead to death.
For more information about our academic and training initiatives, visit Liv Hospital Academy
Frequently Asked Questions for Pediatric Neurology
What is pediatric neurology?
Pediatric neurology is a medical specialty focused on diagnosing and treating nervous system conditions in infants, children, and adolescents. Pediatric neurologists evaluate concerns such as seizures, headaches and migraine, developmental delays, tics, weakness, movement problems, and episodes like staring spells or fainting. Care plans are tailored to age, growth, and family needs.
What are pediatric neurological disorders?
Pediatric neurological disorders affect the brain, spinal cord, nerves, or muscles. Common examples are epilepsy (recurrent seizures), migraine and other headaches, tic disorders (including Tourette syndrome), developmental delay or regression, neuromuscular issues (like low muscle tone or weakness), functional neurological disorder (FND), and sleep related neurological problems.
What is a pediatric neurological exam?
A pediatric neurological exam is an age appropriate evaluation of your child’s brain and nerve function. It checks alertness and attention, eye movements and vision, facial strength and sensation, muscle tone and strength, reflexes, coordination, and sensation. For younger children, it often looks like play to reduce anxiety. The exam determines whether tests such as EEG or MRI are needed.
What can I expect at my child’s first pediatric neurology appointment?
Expect a detailed conversation about symptoms, timelines, triggers, sleep, development, and family history, followed by a gentle neurological exam. Bring videos of events, a symptom diary, prior test results, and a medication list. Depending on the findings, your clinician may order tests such as an EEG, MRI, blood tests, or a sleep study. You’ll leave with a personalized care plan.
What symptoms mean my child should see a pediatric neurologist?
Consider a pediatric neurology visit if your child has: a first unprovoked seizure or repeated spells; frequent or severe headaches (especially morning headaches with vomiting); developmental delay or loss of previously gained skills; persistent weakness, imbalance, or changes in walking; tics causing distress; or nighttime events with snoring and breathing pauses.
What is pediatric epilepsy, and how is it diagnosed?
Pediatric epilepsy is a tendency to have recurrent unprovoked seizures. Diagnosis uses history, event videos when possible, a neurological exam, and an EEG to look at brain wave patterns. Depending on findings, an MRI may be ordered. Treatment may include medication, sleep optimization, trigger management, and a seizure action plan.
What should I do if my child has a seizure?
Stay calm, time the event, turn your child on their side, and clear the area to prevent injury. Do not place anything in the mouth. Call emergency services if a seizure lasts longer than 5 minutes, if breathing is impaired, or if seizures repeat without recovery. Share details and videos with your clinician afterward.
What is a pediatric EEG and why might my child need one?
An EEG records electrical activity in the brain using small scalp sensors. It helps identify seizure tendencies and classify seizure types, guiding treatment. EEGs are painless; sometimes, sleep deprived EEGs are used to increase the test’s yield.



