Last Updated on December 2, 2025 by Bilal Hasdemir

Did you know that childhood cancer is one of the leading causes of death in children worldwide? The episode “The Pediatric Oncologist” from “The Studio” shines a light on the vital work of pediatric oncologists. It also shows the challenges they face. We will look into why identifying and understanding these medical professionals is so important.Learn about the role and location (studio identification) of a Pediatric oncologist studio identification in treating childhood cancers.
In the world of pediatric oncology, we focus on the expertise and credentials needed in this field. The episode “The Studio” shows the complexity of their work. It highlights the need for specialized healthcare professionals. We want to give a full view, stressing their critical role.
Key Takeaways
- Understanding the role of pediatric oncologists in healthcare.
- The challenges faced by medical professionals in pediatric oncology.
- The importance of specialized credentials in pediatric oncology.
- The portrayal of pediatric oncologists in media and its impact.
- The need for continued support for pediatric oncology professionals.
What is a Pediatric Oncologist?

A pediatric oncologist is a doctor who specializes in treating children with cancer. They are key in diagnosing, treating, and managing cancers in kids.
Definition and Role
Pediatric oncologists provide comprehensive care for children with cancer, overseeing their treatment from start to finish. They do more than just give treatments like chemotherapy. They also support families and kids emotionally.
They work with a team, including surgeons and nurses, to give kids the best care. Their leadership in research helps find new ways to fight childhood cancers.
Importance in Child Healthcare
Pediatric oncologists are very important in child healthcare. They tailor care to each child’s needs, considering their health and the cancer type. They also think about how treatments might affect them later.
“The care of children with cancer requires a multidisciplinary approach, with pediatric oncologists playing a central role in coordinating care and making treatment decisions.”
They also play a big part in clinical research. Their work helps find better treatments for kids with cancer. This is key to improving survival rates and quality of life for these children.
- Providing full care to children with cancer
- Leading clinical research in pediatric oncology
- Working as part of a multidisciplinary oncology team
Knowing about pediatric oncologists helps families understand childhood cancer care better.
How Pediatric Oncologists Are Trained

Pediatric oncologists provide comprehensive care for children with cancer, overseeing their treatment from start to finish.
Extensive Education and Training
Pediatric oncologists go through tough medical education and training. They learn the skills needed to diagnose and treat cancers in kids. “
Medical Education Requirements
The journey starts with medical school. Here, aspiring pediatric oncologists learn a solid foundation in medicine. They study subjects like anatomy, biochemistry, and pharmacology.
After medical school, they enter a residency program, usually in pediatrics or a related field. This hands-on experience is key for developing the clinical skills needed to care for children.
Residency and Fellowship Programs
After their residency, those interested in pediatric oncology often pursue specialized training through fellowship programs. These programs give advanced knowledge in diagnosing and treating childhood cancers.
Fellowship programs in pediatric oncology cover topics like chemotherapy, radiation therapy, and surgery. They also focus on supportive care and the role of family in treatment.
By combining extensive medical education with practical experience, pediatric oncologists are ready to provide top care for children with cancer.
Common Types of Pediatric Cancers
It’s important to know about the different types of pediatric cancers. They are different from adult cancers in how they work and how they are treated. We will look at leukemia, brain tumors, and sarcomas, the most common ones.
Leukemia
Leukemia is the most common cancer in kids, making up about 30% of all pediatric cancers. It affects the blood and bone marrow, causing abnormal white blood cells. Acute Lymphoblastic Leukemia (ALL) is the most common type, making up about 80% of cases.
Symptoms include feeling tired, pale skin, and getting sick often. Treatment usually involves chemotherapy. Thanks to better medical care, kids with leukemia have a much better chance of getting better.
Brain Tumors
Brain tumors are the second most common cancer in kids. They can be either benign or malignant and vary in how aggressive they are. Medulloblastoma and gliomas are examples of brain tumors in children.
Symptoms include headaches, nausea, and problems with the nervous system. Treatment depends on the type and location of the tumor. It may include surgery, radiation, and chemotherapy.
Sarcomas
Sarcomas are cancers that start in connective tissues like bones and muscles. Osteosarcoma and Ewing’s Sarcoma are common bone sarcomas in kids. Soft tissue sarcomas, like rhabdomyosarcoma, also occur.
Symptoms include swelling or pain in the affected area. Treatment usually involves surgery, chemotherapy, and sometimes radiation therapy.
| Type of Cancer | Common Subtypes | Typical Treatment Approaches |
| Leukemia | Acute Lymphoblastic Leukemia (ALL) | Chemotherapy |
| Brain Tumors | Medulloblastoma, Gliomas | Surgery, Radiation Therapy, Chemotherapy |
| Sarcomas | Osteosarcoma, Ewing’s Sarcoma, Rhabdomyosarcoma | Surgery, Chemotherapy, Radiation Therapy |
Pediatric oncologists work with a team to create treatment plans for each child. This ensures the best possible results for each child.
Symptoms That May Indicate Cancer in Children
Spotting cancer early in kids is key. We need to know the signs that show a serious health problem. This way, we can get help fast.
Warning Signs to Watch For
Some symptoms point to cancer in kids. These include:
- Persistent fatigue or weakness
- Unexplained weight loss or loss of appetite
- Pain or swelling in the abdomen, legs, arms, or other parts of the body
- Frequent or recurring infections
- Easy bruising or bleeding
- Pale skin or anemia
These signs can also mean other things. But if your kid keeps showing them, see a doctor.
Importance of Early Detection
Finding cancer early in kids helps a lot. Early treatment works better and raises survival chances. Our research teams help find these symptoms and find ways to treat them.
We team up with parents and doctors to give kids the best care. Knowing the signs and acting fast can help kids with cancer get better.
Diagnosis Process in Pediatric Oncology
Diagnosing cancer in kids is a detailed process. It uses imaging and lab tests. This approach is both precise and caring.
We use the latest tech to make sure diagnoses are right and quick. First, we take a detailed medical history and do a physical check. Then, we use advanced imaging.
Imaging Techniques Used
Imaging is key in finding cancers in kids. Here are some imaging methods we use:
- X-rays: Good for first checks and finding bone issues.
- Computed Tomography (CT) scans: Show detailed body images, helping spot tumors.
- Magnetic Resonance Imaging (MRI): Gives clear images of soft tissues, great for brain tumors.
- Positron Emission Tomography (PET) scans: Show how active tumors are, important for treatment plans.
Laboratory Tests
Lab tests confirm the diagnosis and learn about the cancer. These include:
- Blood tests: Check for odd blood cell counts or tumor markers.
- Bone marrow aspiration and biopsy: Look at bone marrow cells for leukemias and lymphomas.
- Lumbar puncture: Check cerebrospinal fluid for cancer cells, important for brain issues.
- Biopsy: Get a tissue sample for detailed cancer analysis.
These tests are vital for a full understanding of the child’s cancer. They help us plan the best treatment.
A top pediatric oncologist says, “Accurate diagnosis is key for treating kids’ cancer. New tech has made diagnosing and treating better.”
“The mix of imaging and lab tests has changed pediatric oncology. It lets us make more precise diagnoses and treatments.”
Treatment Options Offered by Pediatric Oncologists
Pediatric oncologists use many ways to treat childhood cancers. They pick the best treatment based on the cancer type, stage, and the child’s health.
Chemotherapy
Chemotherapy is key in treating many childhood cancers. It uses drugs to kill or slow cancer cells. We use it in different ways, like:
- Systemic chemotherapy: Drugs are given orally or intravenously to target cancer cells throughout the body.
- Regional chemotherapy: Drugs are delivered directly to the affected area, such as through intra-arterial infusion.
Chemotherapy protocols are designed to work well and have fewer side effects.
Radiation Therapy
Radiation therapy kills cancer cells with high-energy rays. We use advanced techniques like IMRT and proton therapy. These methods target tumors well while protecting healthy tissues.
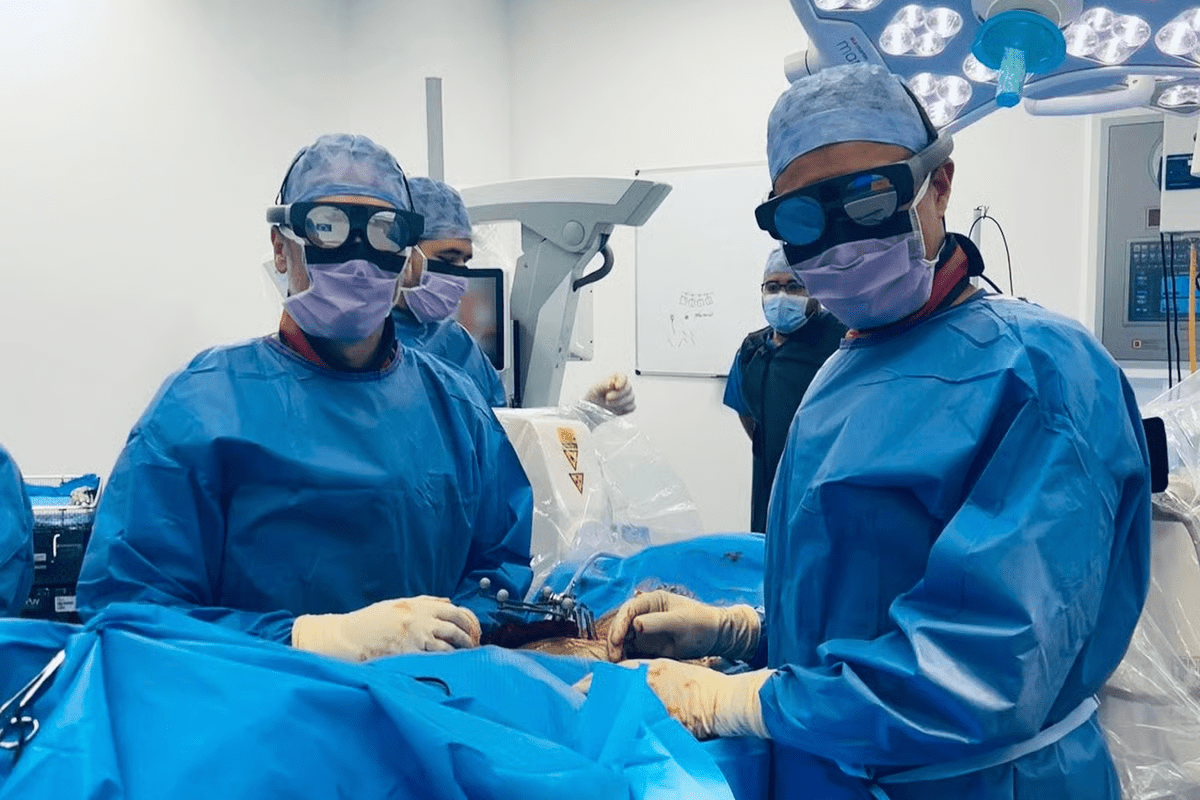
Surgical Interventions
Surgery is important in treating many childhood cancers. It can be used alone or with other treatments. Our surgical oncologists work with other specialists for complete care.
Clinical Trials
Clinical trials test new treatments or interventions. We join these trials to offer our patients new therapies. These trials help us learn more about pediatric cancers and improve treatments.
The table below shows the main treatment options and their benefits:
| Treatment Option | Description | Key Benefits |
| Chemotherapy | Use of drugs to kill cancer cells | Systemic treatment, can target cancer cells throughout the body |
| Radiation Therapy | High-energy rays to kill cancer cells | Precise targeting of tumors, spares healthy tissues |
| Surgical Interventions | Removal of tumors or affected tissues | Can be curative, when used early in treatment |
| Clinical Trials | Research studies for new treatments | Access to innovative therapies, contributes to medical advancements |
By mixing these treatments and tailoring them for each child, we aim for the best results in pediatric oncology.
The Importance of Family Support
Supporting a child with cancer needs a full approach that includes strong family support. When a child gets cancer, the whole family feels it. So, it’s key that families are part of the care.
Involving Family in Treatment Decisions
Getting family involved in treatment choices is key in pediatric oncology. It makes sure the family is on board with the plan and can support the child well. Family involvement can lead to better treatment adherence and improved outcomes. We work with families to understand their worries, likes, and values. This helps in making smart choices.
Shared decision-making is when healthcare teams work with families to choose the best for the child. This method empowers families and makes sure the treatment fits the child and family’s needs.
Resources for Families
Families of children with cancer need many resources to get through treatment. These can include counseling services, financial help, and support groups. Giving families access to these is key to caring for them fully.
| Resource | Description | Benefit |
| Counseling Services | Professional counseling for families to cope with the emotional impact of cancer diagnosis. | Emotional Support |
| Financial Assistance Programs | Programs designed to help families with the financial burden of cancer treatment. | Financial Relief |
| Support Groups | Groups for families to connect with others going through similar experiences. | Community Support |
We know every family is different, and we try to give personalized support to each. Our goal is to make a supportive space for the child and their family to thrive.
What to Expect During a Pediatric Oncology Visit
A pediatric oncology visit is key in a child’s fight against cancer. It’s a mix of care that’s both caring and effective. Knowing what to expect can help families during tough times.
Initial Consultation
The first step is the initial consultation. Here, we check the child’s health in detail. This includes looking at their medical history, doing a physical check, and talking about their symptoms.
Key aspects of the initial consultation include:
- Reviewing the child’s medical history and previous test results
- Conducting a physical examination to assess the child’s overall health
- Discussing the diagnosis, treatment options, and prognosis with the family
- Addressing any questions or concerns the family may have
Follow-Up Appointments
Follow-up visits are vital for checking how the treatment is working. We also manage side effects and adjust the treatment plan if needed. We work closely with families to ensure the best care for the child.
During follow-up appointments, we focus on:
- Assessing the child’s response to the treatment and adjusting the plan as needed
- Managing any side effects or complications that may arise
- Providing ongoing support and guidance to the family
- Coordinating care with other healthcare professionals involved in the child’s treatment
We use patient-centered care models to support the child and their family. We value clear communication, empathy, and understanding in our care.
FAQs About Pediatric Oncology
When a child is diagnosed with cancer, parents have many questions. We’ll answer some of the most common ones here. Pediatric oncology is complex and sensitive. Understanding diagnosis, treatment, and care can be overwhelming.
Common Questions by Parents
Parents often ask many questions when their child is diagnosed with cancer. Some common questions include: “What are the chances of survival?” “What are the treatment options?” and “How will this affect our family?”
- Survival Rates: Advances in medical research have significantly improved survival rates for children with cancer. According to recent studies, the overall survival rate for pediatric cancers is now over 85%.
- Treatment Options: Treatment plans are tailored to the specific type of cancer and the child’s overall health. Options may include chemotherapy, radiation therapy, surgery, or a combination of these.
- Family Support: We emphasize the importance of family support throughout the treatment process. This includes emotional support, counseling, and resources to help families cope.
“The journey through pediatric cancer treatment is challenging, but with the right support and care, families can navigate it together.”
Misconceptions About Pediatric Cancer
There are several misconceptions about pediatric cancer that need to be addressed. One common myth is that cancer in children is rare and untreatable. In reality, while pediatric cancer is less common than adult cancer, treatment outcomes have improved dramatically due to collaborative medical research.
| Myth | Reality |
| Cancer in children is always fatal. | With modern treatment, over 85% of children diagnosed with cancer can survive. |
| Pediatric cancer is caused by genetic factors only. | While genetics play a role, environmental and other factors can also contribute to the development of pediatric cancer. |
| All pediatric cancers are treated the same way. | Treatment plans are highly individualized based on the type of cancer, stage, and the child’s health. |
Collaborative medical research is key in advancing our understanding and treatment of pediatric cancers. By working together, researchers and clinicians can develop more effective treatments and improve outcomes for children with cancer.
We hope this section has provided valuable insights into some of the most common questions and misconceptions about pediatric oncology. For more information or to consult with a specialist, please reach out to our team.
Finding a Pediatric Oncologist
When a child is diagnosed with cancer, finding the right pediatric oncologist is key. It’s important to explore professional networks to find the best specialist for your child.
Guidelines for Selecting a Specialist
Choosing a specialist means looking at their experience, qualifications, and care approach. Research their background, read reviews, and ask for referrals from trusted healthcare providers.
Resources for Locating Qualified Professionals
There are many resources to help find qualified pediatric oncologists. Professional organizations like the Children’s Oncology Group have directories and treatment center info. Your primary care physician can also recommend specialists based on their network.
By following these steps and using these resources, you can find a pediatric oncologist who will give your child the best care.
FAQ
What is a pediatric oncologist, and what role do they play in child healthcare?
A pediatric oncologist is a doctor who specializes in treating children with cancer. They are key in child healthcare. They give care and work with others to help children get better.
What kind of training and education is required to become a pediatric oncologist?
To be a pediatric oncologist, one must go to medical school. Then, they do a residency in pediatrics and a fellowship in pediatric oncology. This training prepares them to care for children with cancer.
What are the common types of cancers that affect children, and how are they treated?
Children often get leukemia, brain tumors, and sarcomas. Treatment varies by cancer type and stage. It might include chemotherapy, radiation, surgery, or clinical trials. Pediatric oncologists create treatment plans for each child.
What are the symptoms and warning signs that may indicate cancer in children?
Signs of cancer in children include tiredness, weight loss, and pain. They might also have swelling or unusual bleeding. Finding these early is important for treatment.
How is cancer diagnosed in children, and what diagnostic tests are used?
Diagnosis uses imaging like X-rays and CT scans, and lab tests like blood tests and biopsies. These help find the cancer type and stage. This info guides treatment.
What treatment options are available for pediatric cancer, and how are they determined?
Treatment options include chemotherapy, radiation, surgery, and clinical trials. The choice depends on the cancer type, stage, and the child’s health. Pediatric oncologists tailor treatment plans for each child.
How can families support their child with cancer, and what resources are available to them?
Families can support their child by being involved in treatment and providing emotional support. There are resources like counseling and support groups. Healthcare teams help families with support and guidance.
What can families expect during a pediatric oncology visit, and how can they prepare?
Visits include a full assessment of the child’s condition. Families should bring medical records and ask questions. This helps them prepare and understand the care their child is receiving.
How can I find a qualified pediatric oncologist for my child?
To find a pediatric oncologist, ask your child’s doctor for a referral. You can also check with your insurance or search online. Professional organizations like the American Society of Pediatric Hematology/Oncology can provide lists of qualified doctors.
References
World Health Organization. Evidence-Based Medical Insight. Retrieved from https://www.who.int/news-room/fact-sheets/detail/cancer-in-children
Trusted Medical Source. Evidence-Based Medical Insight. Retrieved from https://www.unicef.org/health/children-and-cancer