Last Updated on December 2, 2025 by Bilal Hasdemir
Cancer is a major cause of death in kids around the world. But, thanks to new medical treatments, more kids are surviving. Radiation therapy is key in treating many cancers and tumors. It kills cancer cells and stops them from growing.Get a comprehensive Pediatric radiation therapy overview, including treatment goals, delivery methods, and safety protocols for children.
Getting a cancer diagnosis is very tough for families. We aim to provide detailed information on cancer treatment for children. This includes how radiation therapy helps fight childhood cancers. Knowing about treatment options and childhood oncology protocols helps families make better choices for their kids.
Key Takeaways
- Cancer is a significant health issue in children globally.
- Radiation therapy is a vital treatment for various cancers and tumors.
- Understanding treatment options is key for families.
- Childhood oncology protocols guide the treatment process.
- Advancements in medical treatments have improved survival rates.
Introduction to Pediatric Radiation Therapy
Radiation therapy in pediatric oncology has changed how we treat cancers in kids. It offers advanced medical interventions that meet the special needs of young patients. We create each child’s treatment plan to reduce tumors and side effects.
Definition and Importance
Pediatric radiation therapy uses high-energy particles or waves to kill cancer cells. It’s key in treating childhood cancers, giving a targeted approach that boosts patient outcomes. This treatment is a minimally invasive option, used alone or with surgery and chemotherapy.
Our team works with families to make a treatment plan for each child. We use the latest in radiation therapy for precise and effective treatments. This helps increase the chances of a successful outcome.
Historical Context
The history of pediatric radiation therapy has seen big tech and technique improvements. We’ve moved from old radiation therapy to targeted radiation techniques like IMRT and proton therapy. These new methods help us target cancer more accurately, protecting healthy tissues and reducing side effects.
We keep improving our pediatric radiation therapy methods. We aim to give the best care to our young patients. By using advanced technology and a caring approach, we work towards the best results for kids undergoing radiation therapy.
Indications for Use in Pediatrics

Radiation therapy is key in treating many pediatric cancers and conditions. The choice to use it in kids depends on several factors. These include the cancer type and stage, the child’s health, and the treatment’s benefits and risks.
We use radiation therapy for kids with certain cancers that it works well on. Some common cancers treated with it are:
Common Pediatric Cancers Treated
- Brain and Central Nervous System Tumors: Radiation helps treat tumors in the brain and spinal cord.
- Neuroblastoma: It’s used for advanced or spread-out cases of this cancer.
- Wilms Tumor: It’s part of the treatment plan for this kidney cancer, along with surgery and chemotherapy.
- Hodgkin and Non-Hodgkin Lymphoma: It targets cancer in the lymphatic system.
- Rhabdomyosarcoma: This soft tissue sarcoma is treated with radiation as part of a full treatment plan.
Other than these cancers, radiation therapy is also used for other conditions that need precise and effective treatment.
Conditions Requiring Radiation Therapy
Some conditions that might need radiation therapy in kids include:
- Tumors of the Eye and Orbit: It treats tumors in the eye and surrounding areas.
- Certain Leukemias: It’s used for leukemia that has spread to the central nervous system or other areas.
- Pediatric Sarcomas: It’s often part of the treatment for various sarcomas in children.
We adjust the type and amount of radiation therapy for each child. This ensures the treatment is effective and minimizes side effects.
Techniques Used in Pediatric Radiation Therapy
Pediatric radiation therapy uses advanced methods to fight cancer while protecting healthy tissue. We use these therapeutic radiation protocols to help our young patients get the best care.
The right technique depends on the cancer type, the child’s health, and treatment goals. Let’s look at the main methods used in pediatric radiation therapy.
External Beam Radiation Therapy (EBRT)
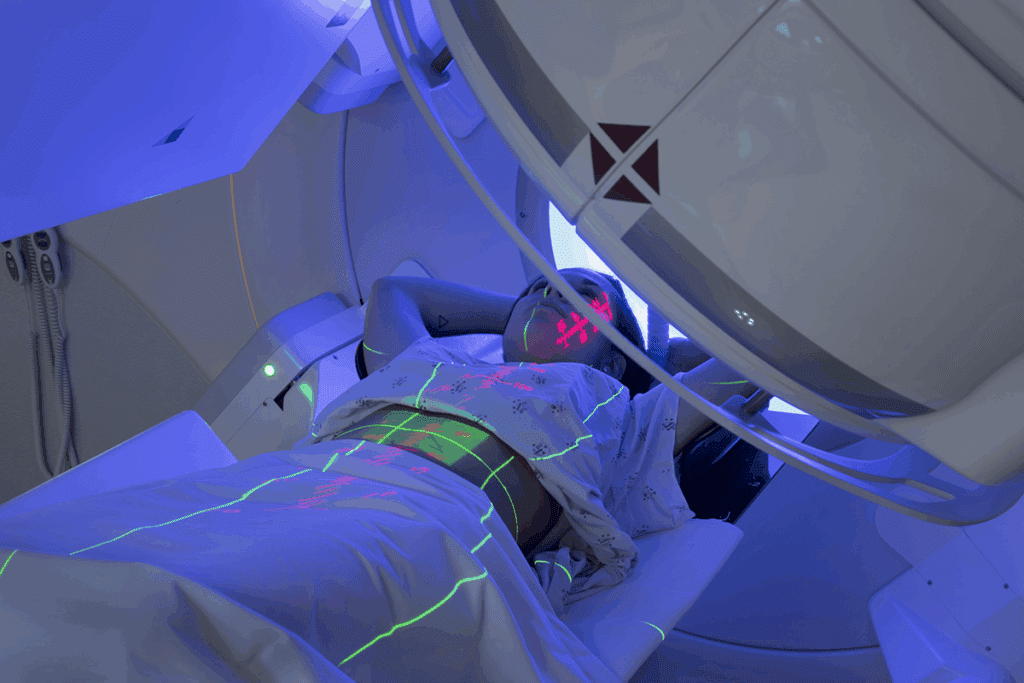
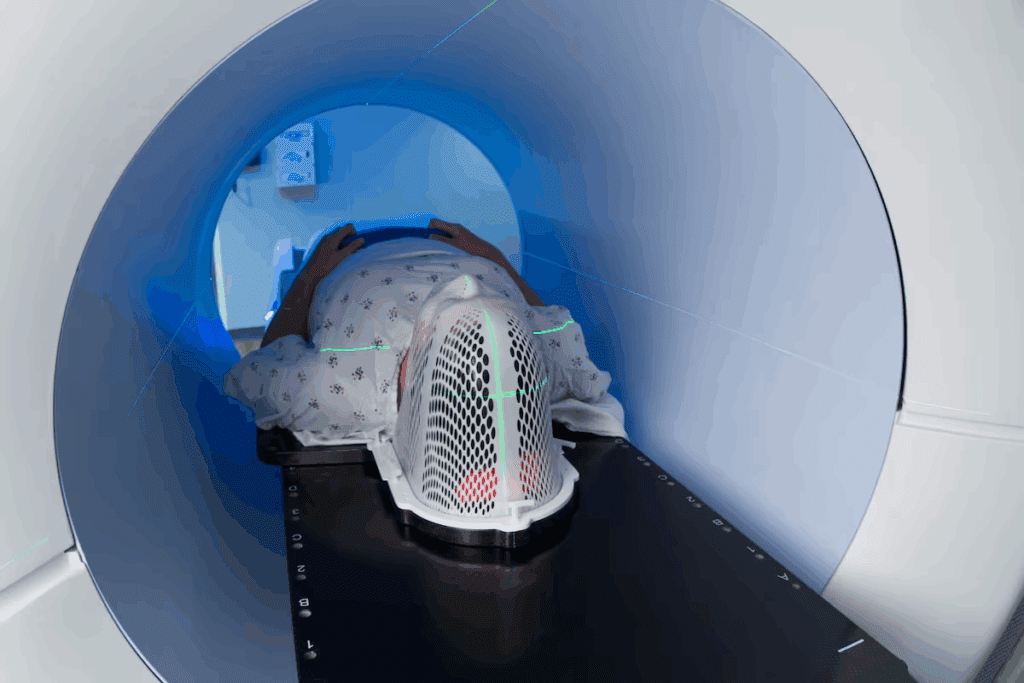
External Beam Radiation Therapy (EBRT) is a common method for treating pediatric cancers. It sends radiation from outside the body to the tumor. This method helps target cancer cells well, reducing harm to healthy tissues.
Medical experts say, “External radiation therapy uses a large machine and special equipment to aim the right amount of radiation at cancerous tumors.” This way, we can treat effectively while protecting other tissues.
“The precision of EBRT has been significantly enhanced by advancements in technology, allowing for more accurate targeting of tumors and better sparing of normal tissues.”
Brachytherapy
Brachytherapy is another technique used in pediatric radiation therapy. It involves placing a small amount of radioactive material inside or near the tumor. This method delivers high doses of radiation directly to the cancer, reducing harm to healthy tissues.
Brachytherapy is great for treating localized tumors. It’s an effective option for some pediatric cancers.
Proton Therapy
Proton therapy is a specialized form of radiation therapy. It uses protons instead of X-rays to target tumors. This method delivers a focused dose of radiation to the tumor, with less damage to healthy tissues.
Proton therapy is best for tumors near important structures like the brain, spine, or heart. It’s a key treatment option for some pediatric cancers, aiming to reduce long-term side effects.
By using these advanced cancer cell targeting techniques and a specialized medical approach, we can offer effective treatments for children with cancer. This improves their survival chances and quality of life.
Treatment Planning and Preparation
Planning treatment for kids with radiation therapy is a team effort. We know every child is different. So, we create a plan that works well and is safe.
Comprehensive Evaluation
Starting with a detailed check-up is key. We look at the child’s medical history, do physical exams, and run tests. This helps us understand the disease and the child’s health.
Before treatment starts, a radiation therapist marks the skin with ink. This “tattoo” makes sure the treatment goes to the right spot. It’s important for comprehensive treatment planning and keeping healthy tissues safe.
Imaging Techniques Utilized
Using the latest imaging is important for radiation exposure management. We use MRI, CT scans, and PET scans to see the tumor and tissues clearly. These images help us plan the treatment just right for the child.
With advanced medical technology, we can give radiation therapy with great precision. This makes the treatment more effective and reduces side effects. It’s all about giving the best care to kids.
We aim to provide detailed information on cancer treatment for children.
Pediatric Dosimetry Considerations
When treating children with radiation therapy, dosimetry is key. It helps find the right dose to kill tumors without harming healthy tissues. Getting the dose just right is essential for the treatment’s success and the child’s health.
Calculating Radiation Doses for Children
Figuring out the right radiation dose for kids involves looking at several things. This includes the tumor’s size, where it is, and the child’s health and age. Precision radiation dosage is vital to treat the tumor well and protect healthy tissues.
We use top-notch imaging and treatment planning systems to customize the dose for each child. This approach boosts treatment success and lowers the chance of side effects.
Minimizing Exposure Risks
Keeping exposure risks low is our main goal in treating kids with radiation. We use advanced techniques like intensity-modulated radiation therapy (IMRT) and proton therapy to do this.
| Technique | Description | Benefits |
| IMRT | Delivers radiation beams of varying intensities from multiple angles | Precise targeting of tumors, reduced exposure to healthy tissues |
| Proton Therapy | Uses protons instead of X-rays to destroy cancer cells | Reduced risk of secondary cancers, less damage to surrounding tissues |
By planning and delivering radiation therapy carefully, we can lower exposure risks. This helps ensure the best treatment results for kids. Our aim is to manage radiation exposure in a way that keeps our young patients healthy.
Pediatric health optimization is our main focus. We make sure every child gets the best care possible.
Consultation and Multidisciplinary Approach
Effective pediatric radiation therapy needs a specialized medical approach. A team of experts works together to care for young patients.
Healthcare professionals like pediatric oncologists, radiation oncologists, nurses, and support staff collaborate. They create a treatment plan that meets each child’s unique needs.
Role of Pediatric Oncologists
Pediatric oncologists are key in treating childhood cancers. They check the patient’s condition and suggest treatment options. They work with radiation oncologists to make sure the treatment is right.
Their role is vital in:
- Checking the patient’s health and medical history
- Finding the best treatment strategy
- Coordinating with other healthcare professionals
Involvement of Radiation Oncologists
Radiation oncologists focus on using radiation to treat cancer. They work with pediatric oncologists to plan treatments. They make sure the radiation doses are right to be effective and safe.
They are in charge of:
- Creating and carrying out the radiation treatment plan
- Using advanced tech to give precise radiation doses
- Watching how the patient responds and adjusting the plan if needed
Pediatric oncologists and radiation oncologists work together. They create healing radiation strategies that fit each child’s needs. This improves treatment results and quality of life for young patients.
The pediatric oncology interventions our team uses are all-encompassing and caring. They address the physical, emotional, and psychological needs of our young patients.
Side Effects and Management
Pediatric radiation therapy is a key treatment for many cancers in kids. It can cause short-term and long-term side effects. We aim to reduce these effects and help kids recover well.
Short-term Side Effects
Radiation therapy can harm healthy cells around the tumor. This can lead to immediate side effects. Some common ones include:
- Skin Problems: Skin can get irritated, red, and sensitive.
- Fatigue: Kids might feel very tired and unwell.
- Hematological Effects: It can affect bone marrow, causing anemia and low blood counts.
We help manage these side effects. This includes advice on skin care, nutrition, and blood count checks.
Long-term Effects and Monitoring
Long-term side effects can show up months or years later. These might include:
- Growth and Development Issues: Radiation can affect how kids grow and develop.
- Secondary Cancers: There’s a small chance of getting new cancers later due to radiation.
- Organ Dysfunction: There’s a risk of long-term problems with organs depending on the area treated.
We stress the need for long-term care to watch for these effects. This means regular check-ups, scans, and organ function tests.
Knowing about the side effects of pediatric radiation therapy helps us manage them better. This way, we can improve treatment results and the quality of life for our young patients.
Advances in Pediatric Radiation Therapy
Technology and research are changing pediatric radiation therapy. We now have better ways to treat kids. These new methods focus on being precise and reducing side effects.
Innovations in Technology
New tech has made pediatric radiation therapy better. For example, proton therapy is a big step forward. It targets tumors well while protecting healthy tissues.
A study found that new tech lets us treat cancer better. It also helps avoid harm to healthy tissues in kids.
“New technologies enable us to target the cancer while sparing nearby healthy tissue better now than ever before.”
— Source: Second web source
Some key tech advancements include:
- Advanced imaging for clearer tumor views
- Intensity-modulated radiation therapy (IMRT) for precise doses
- Image-guided radiation therapy (IGRT) for live monitoring
- Proton therapy for fewer side effects
| Technology | Benefit | Clinical Impact |
| Proton Therapy | Precise tumor targeting | Reduced long-term side effects |
| IMRT | Precise dose delivery | Enhanced tumor control |
| IGRT | Real-time monitoring | Improved treatment accuracy |
Research and Clinical Trials
Research and trials are key to improving pediatric radiation therapy. We’re always looking for new ways to help patients.
Some areas we’re exploring include:
- Personalized therapy based on genetics
- New radiation sensitizers to boost treatment
- Advanced ways to deliver radiation
We’re always trying to do better for our young patients. We’re using new medical approaches, advanced diagnostics, and adaptive tech to improve care.
Parental Involvement and Support
When a child gets radiation therapy, parents play a key role in their emotional health. We know it’s tough for the whole family. So, we focus on supporting the child and their family fully.
Psychosocial Support for Families
Families facing pediatric radiation therapy need more than just medical help. They need emotional support too. We offer personalized treatment approaches for each child and family. This includes counseling, support groups, and stress management resources.
We encourage families to get involved in their child’s care. For example, we suggest they take a tour of the radiation department. This helps them get used to the place and the equipment. It can really help reduce anxiety and make treatment easier.
Educational Resources Available
It’s important for families to understand the treatment process. We have many educational resources to help. These include brochures, online materials, and consultations with our specialists.
- Detailed explanations of the treatment process
- Information on possible side effects and how to handle them
- Advice on nutrition and lifestyle during treatment
- Access to support groups and counseling services
We aim to support families fully through pediatric radiation therapy. Our goal is to give every child the best care, with their family’s support every step of the way.
Guidelines and Safety Protocols
We have strict rules to keep our young patients safe during radiation therapy. Making sure this treatment is safe and works well is our top priority. We follow strict standards to meet this goal.
Radiation Safety Standards
Keeping radiation safe is key in pediatric therapy. We protect our patients and staff with strict rules. We use specialized oncology techniques and special equipment to lower exposure.
- Regular checks on radiation therapy equipment.
- Staff training on the latest safety guidelines.
- Using regenerative medical approaches to lessen long-term effects.
Protocols to Ensure Patient Safety
We have many ways to keep patients safe. For example, patients are often in private rooms. This keeps others safe from radiation.
Our team enters these rooms briefly and works fast. They follow radiation safety rules closely.
Some important steps include:
- Planning treatments carefully to give the right dose of radiation.
- Watching the patient’s health closely during treatment.
- Following radiation safety protocols to reduce risks.
We use the latest technology and care with strict safety rules. Our goal is to give the best treatment to our young patients.
Conclusion and Future Directions
We aim to treat cancer in kids well while keeping side effects low. We make a plan for each child to fight the tumor and keep side effects down.
Emerging Trends
New medical tech is changing how we treat cancer. It lets us adjust plans as we go and hit tumors more accurately. We’re also looking into ways to fix damaged tissues after radiation.
Enhancing Outcomes
We’re using all kinds of healing methods to help kids feel better. This includes the latest in radiation tech, support for their minds, and help for their families.
We’re dedicated to making care better for kids with cancer. We’re always looking for new ways to help them have a bright future.
FAQ
What is pediatric radiation therapy?
Pediatric radiation therapy is a treatment that uses high-energy radiation. It targets and destroys cancer cells in children. This helps manage and potentially cure various types of childhood cancers.
How does radiation therapy work in treating childhood cancers?
Radiation therapy delivers precise doses of radiation to cancerous tumors. It damages the DNA of cancer cells. This prevents them from growing and dividing, leading to cell death.
What are the different techniques used in pediatric radiation therapy?
Pediatric radiation therapy uses several techniques. These include External Beam Radiation Therapy (EBRT), brachytherapy, and proton therapy. Each has its own benefits and uses in treating childhood cancers.
What is the role of a multidisciplinary team in pediatric radiation therapy?
A multidisciplinary team is key in pediatric radiation therapy. It includes pediatric oncologists and radiation oncologists. They provide complete care to children undergoing therapy, ensuring effective treatment and minimizing side effects.
What are the possible side effects of pediatric radiation therapy?
Side effects of pediatric radiation therapy can be short-term or long-term. Short-term effects include fatigue, skin reactions, and hair loss. Long-term effects can affect growth and development and increase the risk of secondary cancers.
How are radiation doses calculated for children?
Radiation doses for children are calculated based on several factors. These include the type and stage of cancer, the child’s age and size, and the radiation therapy technique. The goal is to deliver effective treatment while minimizing exposure risks.
What measures are taken to ensure patient safety during radiation therapy?
Patient safety during radiation therapy is ensured through several measures. These include following radiation safety standards, precise treatment planning, and ongoing monitoring for side effects. Protocols are also in place to minimize exposure to healthy tissues.
How can families support their child during radiation therapy?
Families can support their child during radiation therapy in many ways. They can provide emotional support, help manage side effects, and access educational resources and psychosocial support services.
What advancements are being made in pediatric radiation therapy?
Advances in pediatric radiation therapy include new technology and research. Improved imaging techniques and more precise radiation delivery systems are being developed. Ongoing research and clinical trials aim to enhance treatment outcomes for children.
What is the future of pediatric radiation therapy?
The future of pediatric radiation therapy looks promising. It focuses on improving treatment outcomes for children. Emerging trends include personalized medicine approaches and advanced radiation therapy techniques.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC3636568/
JAMA Network. Evidence-Based Medical Insight. Retrieved from https://jamanetwork.com/journals/jamaoncology/fullarticle/2400657
Nature. Evidence-Based Medical Insight. Retrieved from https://www.nature.com/articles/nrclinonc201721





