Last Updated on November 27, 2025 by Bilal Hasdemir

Every year, thousands of children worldwide die from sickle cell disease (SCD). This genetic disorder affects how red blood cells are made. It makes them misshapen. This condition causes severe pain and increases the risk of infections and stroke in children. Identifying the major medical events and conditions that contribute to Pediatric sickle cell mortality in childhood and adolescence.
It’s important to understand the risks and use effective management strategies. This can help lower mortality rates in children with SCD.
Comprehensive care is critical for improving outcomes in children with SCD. By tackling the advanced medical challenges of SCD, we can improve their lives and survival chances. Managing the disease comprehensively is essential for this goal.
Sickle Cell Disease (SCD) is a genetic disorder that affects hemoglobin production. Hemoglobin is a protein in red blood cells that carries oxygen. It impacts children all over the world.
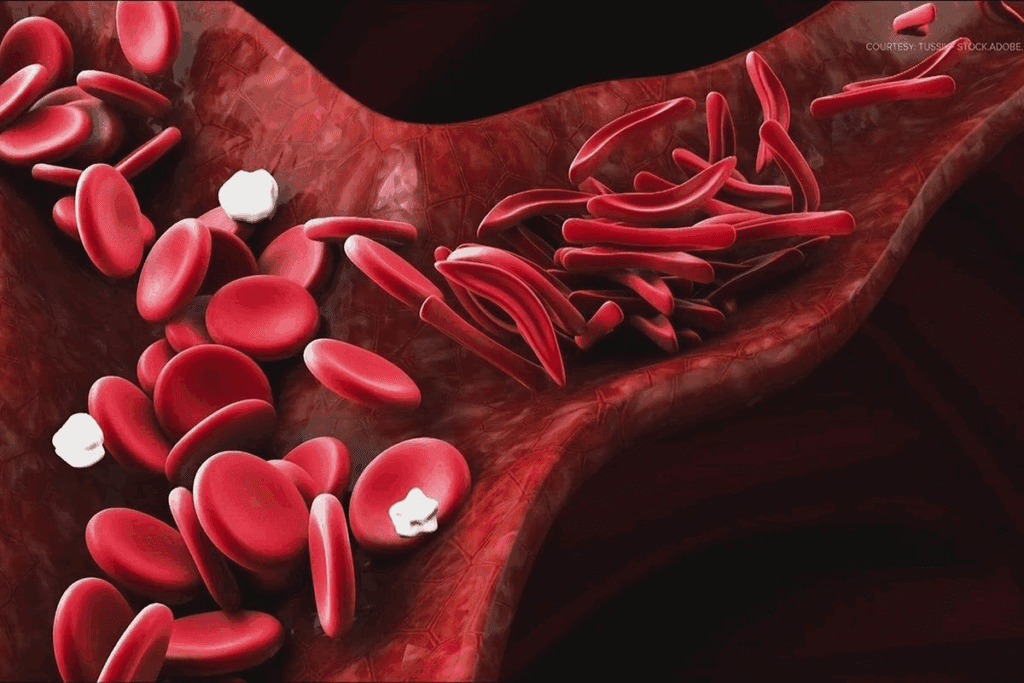
Sickle Cell Disease is caused by abnormal hemoglobin, called hemoglobin S. This hemoglobin makes red blood cells rigid and sickle-shaped. These sickled cells can block blood vessels, causing pain and organ damage. The HBB gene variation leads to this defective hemoglobin.
Children with SCD may have pain episodes, fatigue, and jaundice. The disease can greatly affect their quality of life. They need close health monitoring and specialized care.
Managing SCD means treating symptoms and preventing complications. Vaccinations and regular check-ups are key. Parents and caregivers play a big role in watching their child’s health and getting medical help when needed.
It’s important to know the different types of sickle cell disease for good management. Sickle cell disease (SCD) affects hemoglobin, a protein in red blood cells. It carries oxygen to the body’s parts.
SCD is divided into several types based on genetic mutations. The main types are:
Each type affects health differently, from mild to severe symptoms.
Sickle cell anemia, or HbSS, is the most severe SCD type. It happens when someone gets two abnormal hemoglobin genes, one from each parent. This leads to hemoglobin S production, causing red blood cells to break down.
Characteristics of Sickle Cell Anemia:
Sickle cell trait, or HbAS, is when someone has one normal and one abnormal hemoglobin S gene. People with this trait usually don’t show SCD symptoms but can pass the gene to their kids.
Key aspects of Sickle Cell Trait:
Other types include HbSC disease and HbS beta thalassemia. HbSC disease happens when someone has one HbS and one HbC gene. HbS beta thalassemia is when someone has one HbS and one beta thalassemia gene.
| Type of SCD | Genetic Makeup | Health Implications |
| Sickle Cell Anemia (HbSS) | Two abnormal hemoglobin S genes | Severe anemia, pain crises, infections |
| Sickle Cell Trait (HbAS) | One normal and one abnormal hemoglobin S gene | Generally asymptomatic, can pass to offspring |
| HbSC Disease | One HbS and one HbC gene | Mild to moderate anemia, some pain episodes |
| HbS Beta Thalassemia | One HbS and one beta thalassemia gene | Variable severity, anemia, and other complications |
Knowing the exact type of SCD is key for the right treatment. Advanced medical screening helps find the disorder’s exact nature. This lets doctors give the best disease management.
Sickle Cell Disease (SCD) is a big health issue in the United States, hitting many children hard. It’s more common in people of African, Caribbean, and Mediterranean backgrounds. Knowing how widespread SCD is helps us plan better healthcare and services.
SCD hits some groups harder than others. Kids of African descent are most affected, thanks to their genetic makeup. Early diagnosis and care are key to better lives for these kids.
It also affects kids from Caribbean and Mediterranean backgrounds. Genetic counseling and screening are vital for families with SCD history.
SCD’s spread varies across the United States. Some areas have more cases because of their populations. Urban spots with diverse people tend to see more cases.
Places with big African American populations, like the Southeast, have more SCD. Knowing where SCD is common helps us focus our efforts better.
By pinpointing high-risk areas, we can better use our resources. This ensures kids get the care they need quickly. It’s all about reducing SCD’s bad effects and improving health.
Understanding Sickle Cell Disease (SCD) is key to managing it well. SCD is a genetic disorder that affects how red blood cells make hemoglobin. This makes these cells sickle-shaped under certain conditions.
SCD is passed down in an autosomal recessive pattern. This means a child needs two abnormal hemoglobin genes, one from each parent, to have the disease. Genetic counseling is very important for families with SCD history.
It helps them understand the risk of passing the disease to their kids. Genetic counseling gives families important info about their children’s chances of getting SCD.
If both parents carry the sickle cell trait, there’s a 25% chance with each pregnancy that the child will have SCD. Knowing this risk is important for planning families and preparing for their children’s needs.
Genetics are important in SCD, but environmental factors also play a big role. Things like infections, dehydration, and extreme temperatures can cause sickle cell crises. Managing these factors is important to reduce complications.
For example, staying hydrated and avoiding extreme temperatures can help prevent some crises. Also, getting all recommended vaccinations can lower the risk of infections that might trigger a crisis. Understanding and managing these environmental risks is a big part of SCD management.
Sickle Cell Disease in kids shows up in many ways that need quick action. We’ll look at the usual signs and serious problems linked to SCD. It’s key to spot these early and act fast.
Kids with SCD might have pain, anemia, jaundice, and get sick easier. Pain episodes, or crises, are really tough and need good pain care. Watching for these signs is very important.
Every child with SCD is different. They might show:
These signs can really hurt a child’s life. So, it’s important to watch closely and treat quickly.
SCD can cause serious problems like stroke, acute chest syndrome, and splenic sequestration. Stroke is a big deal that can affect a child’s health and growth. We’ll talk more about these issues, why prevention and quick medical help are so important.
Handling serious problems often means using blood transfusions to lower stroke risk. Regular doctor visits and sticking to treatment plans are key to lessening SCD’s effects on a child’s life.
Spotting symptoms early and acting fast is key to managing SCD well. Knowing the usual signs and serious issues helps us care for kids with this condition better.
Sickle Cell Disease diagnosis starts with screening newborns. This is to catch the condition early. Early detection helps manage the disease better and improves life quality for kids with SCD.
Newborn screening programs are the first step in diagnosing Sickle Cell Disease. They are key for early detection and prompt medical care. The screening involves a blood test to check for abnormal hemoglobin levels.
Key screening methods include:
After initial screening, confirmatory tests are done to confirm the diagnosis. These tests are more detailed. They help in creating a proper treatment plan.
Confirmatory tests may include:
We stress the importance of these diagnostic steps. They are vital for providing complete care for children with Sickle Cell Disease. Advanced diagnostic techniques and specialized health evaluations are key in managing the condition.
Managing sickle cell disease requires a detailed treatment plan. Each patient’s needs are different. So, treatments must be customized to meet those needs.
Pain management is key in treating sickle cell disease. We use various methods to control pain. These include medicines and alternative therapies. Our goal is to reduce pain and enhance life quality.
Medications: We prescribe different medicines for pain. These range from common pain relievers to stronger drugs for severe pain.
Blood transfusions are vital for sickle cell disease treatment. They increase normal red blood cells in the body. This reduces the risk of serious complications.
| Condition | Treatment Approach | Benefits |
| Severe Pain Crisis | Immediate blood transfusion, pain management medication | Reduces pain, improves oxygen delivery to tissues |
| Stroke Prevention | Regular blood transfusions | Decreases risk of stroke, improves overall health |
Bone marrow transplantation can cure sickle cell disease. We consider it for those with severe disease and a compatible donor.
Benefits and Risks: This treatment can cure the disease but has risks like graft-versus-host disease. We carefully consider these when deciding on this option.
We aim to offer personalized treatment protocols and advanced clinical management. This ensures the best care for our patients. Tailoring treatments to individual needs improves life quality for those with sickle cell disease.
Preventative care is key for kids with Sickle Cell Disease. It helps lower the chance of serious problems. We focus on a full plan that includes shots, regular doctor visits, and keeping healthy with good food and water.
Vaccines are very important for kids with SCD. Big dangers like pneumococcus and meningococcus infections can be stopped with shots. Also, eating right and drinking enough water helps keep them healthy.
Medical Expert, “Vaccines and staying healthy are essential to fight off infections and manage SCD well.”
“Stopping infections is key in SCD care. Shots against pneumococcus and meningococcus are very important.”
Regular doctor visits are important to watch how the disease is doing. These visits help doctors catch problems early. This means they can help kids with SCD get better faster.
By focusing on care before problems start, we can make life better for kids with SCD. It’s also important to have family support. This makes sure kids get the care they need in a loving place.
Healthcare has made big strides in cutting down sickle cell disease (SCD) deaths in kids worldwide. We’ve seen a big leap in managing SCD, leading to more kids living longer. This part will look at how death rates have changed over time and what we’re doing now to keep improving.
SCD used to be a big killer in kids, mainly because of infections and sudden problems. But, thanks to newborn screenings, shots, and full care plans, death rates have dropped a lot. Early action and care have been key in cutting down SCD-related deaths.
Research shows that screening all newborns for SCD has greatly lowered death rates in kids with the disease. This early check-up lets doctors start treatment right away. This includes giving penicillin to prevent infections and shots to fight off pneumococcus, a big threat to SCD patients.
Today, we’re seeing fewer SCD deaths in kids, thanks to better medical care and new ways to manage the disease. Better pain control, more blood transfusions, and better ways to stop infections have all helped kids do better.
We’re moving towards care that’s more about each child, with plans made just for them. This, along with regular check-ups and care, has really helped lower death rates. Plus, new research into treatments and therapies is promising for even better survival chances.
As we keep learning and improving how we handle SCD, it’s vital to keep focusing on full care. This includes mental support and teaching families. By doing this, we can keep cutting down SCD deaths in kids and make their lives better.
Families with Sickle Cell Disease face many challenges. They need a lot of support to manage the condition. This support includes medical care and a strong support system with various resources and care approaches.
A multidisciplinary care approach is key. It involves a team of healthcare experts. They include pediatricians, hematologists, nurses, and social workers. Together, they help with the medical, emotional, and social needs of children with SCD and their families.
Support groups are very important for families with SCD. They offer emotional support and practical advice. These groups let families share experiences, get guidance, and connect with others who understand their challenges.
Online resources are also very helpful for parents. They include:
We believe that using these support systems and resources helps families manage SCD better. It improves the quality of life for their children.
Research on Sickle Cell Disease (SCD) is moving fast, bringing hope to kids with this condition. We’re seeing big steps forward in new treatments and ways to help patients live better lives.
New treatments like gene therapy are being looked into to fix the problems caused by SCD. These therapies aim to make sickle cell crises less common and less severe. This could greatly improve life for those affected.
Clinical trials and studies are key to checking if new treatments work well and are safe. A new approach to care is being used, mixing medical treatment with support. This aims to give patients a more complete care plan. We’re all in this together, working to improve how SCD is managed.
Sickle cell disease is a genetic disorder that affects hemoglobin production. This causes red blood cells to become misshapen and break down. It can lead to serious health issues, like severe pain, infections, and stroke risk.
There are several types, including sickle cell anemia (HbSS) and sickle cell trait. Other variants like HbSC disease and HbS beta thalassemia have different severities and health impacts.
Diagnosis starts with a newborn screening. Then, confirmatory tests determine the specific type of SCD. These tests help understand the condition’s severity and characteristics.
Symptoms include severe pain, infections, and other complications. Recognizing these symptoms early is key for effective management.
Pain management is tailored to each child. It may include medication, hydration, and other supportive measures. Effective pain management improves their quality of life.
Blood transfusions increase normal red blood cells, reducing complications. They are used for severe anemia, stroke prevention, and other complications.
Sickle cell disease is genetic and cannot be prevented. But, understanding risk factors and genetic counseling can help families. Preventative care, like vaccinations, can also reduce complications.
Families can find support groups, online resources, and a multidisciplinary care approach. These offer emotional support, practical advice, and overall care for managing SCD.
Advances in care have led to improved survival rates. Better pain management, infection prevention, and monitoring are key. Understanding these trends helps in improving care further.
New treatments, like gene therapy and medications, are being explored. Ongoing clinical trials aim to improve SCD outcomes.
Families need a multidisciplinary approach for care. This includes regular check-ups, pain management, and preventive measures. Working closely with healthcare providers is essential for a personalized care plan.
The Lancet. Pediatric Sickle Cell Disease Mortality Worldwide. Retrieved from https://www.thelancet.com/journals/lanhae/article/PIIS2352-3026(23)00107-2/fulltext[1
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!