Last Updated on December 1, 2025 by Bilal Hasdemir
Cancer remains one of the leading causes of death worldwide. In the United States, it causes nearly one in four deaths, says the American Cancer Society. The deadliest cancers are lung, pancreatic, and colon. They are often found late, making treatment hard which also rely on the PET scan lifetime limit.
Metastatic cancer makes treatment even harder. It happens when cancer cells spread to other parts of the body. This leads to higher cancer mortality rates. Knowing how these aggressive cancers work is key to finding better treatments.
Key Takeaways
- Cancer is the second-leading cause of death in the United States.
- Lung, pancreatic, and colon cancers are among the deadliest forms.
- Metastatic cancer complicates treatment and increases mortality.
- Understanding cancer behavior is key to effective treatment.
- Advanced cancers often require frequent diagnostic procedures.
Understanding Metastatic Cancer
Metastasis is when cancer cells spread from the first tumor to other parts of the body. This complex process is a key feature of advanced cancer. It is responsible for most cancer-related deaths.
Definition and Process of Metastasis
Metastasis happens when cancer cells leave the primary tumor. They invade nearby tissues and enter the bloodstream or lymphatic system. Then, they travel to distant sites, forming new tumors.
The metastasis process includes several steps. These are invasion, circulation, and colonization of cancer cells at new sites. The ability of cancer cells to metastasize depends on many factors. These include the type of cancer, its genetic makeup, and the tumor’s environment.
Understanding the metastasis process is key for developing effective treatments. It helps improve patient outcomes.
Common Sites of Metastasis
Cancer can spread to different parts of the body, but some sites are more common. The lungs, liver, and bones are among the most frequent sites. The lungs are a common site because of their rich blood supply.
The liver is also a common site, as it receives a lot of blood from the digestive tract. Bones, like those in the spine, pelvis, and ribs, are often affected too.
Detecting metastatic disease is critical for determining the cancer stage and planning treatment. Imaging techniques, like PET scans, are vital for identifying metastases. They help monitor how well treatment is working.
It’s also important to understand the risks of PET scan radiation exposure. This helps balance the benefits of diagnosis with the risks.
The Most Lethal Metastatic Cancers
The deadliest metastatic cancers are tough to treat and care for. They spread quickly to other parts of the body. This makes them very aggressive and hard to manage.
Pancreatic Cancer Metastasis
Pancreatic cancer is hard to catch early and has a poor outlook. Metastatic pancreatic cancer often goes to the liver, lungs, and peritoneum. This makes treatment harder. The five-year survival rate for this cancer is very low, showing we need better treatments.
Lung Cancer Metastasis
Lung cancer is also very deadly and spreads fast. Non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC) are the main types. SCLC is more aggressive and spreads early. It often goes to the brain, bones, and liver. While new treatments help some, the outlook for advanced disease is bleak.
Liver Cancer Metastasis
Liver cancer, whether it starts there or spreads, is hard to treat. The liver is a common place for cancer to spread from, like colorectal and pancreatic cancer. Metastatic liver cancer usually means the disease is advanced. Treatment options are mostly palliative care or clinical trials.
Brain Metastases from Various Primary Sites
Brain metastases can come from many cancers, like lung, breast, and melanoma. These are serious because they affect quality of life and are hard to treat. Whole-brain radiation therapy and stereotactic radiosurgery are common treatments. But, the outcome depends on the cancer type and how many metastases there are.
In summary, the deadliest metastatic cancers need a complex treatment plan. This includes early detection, aggressive treatments, and palliative care to help patients.
Factors That Determine Metastatic Cancer Mortality
Metastatic cancer mortality is influenced by many factors. Knowing these factors helps doctors predict outcomes and choose treatments.
Stage at Diagnosis
The cancer’s stage at diagnosis greatly affects survival. Early detection leads to better survival rates. Early detection is key to improving outcomes in cancer patients.
Location and Number of Metastatic Sites
The location and number of metastatic sites are also important. Metastasis to vital organs like the brain or liver often means a worse prognosis. The spread of cancer to multiple sites complicates treatment and generally results in higher mortality.
Genetic and Molecular Factors
Genetic and molecular characteristics of the tumor affect its spread and treatment response. Certain genetic mutations can make tumors more aggressive or resistant to treatment.
Response to Treatment Options
The success of treatment is another key factor. Patients who respond well to initial treatments generally have better outcomes. Treatment response is a significant prognostic indicator in metastatic cancer.
Understanding these factors helps healthcare providers assess patient prognosis and tailor treatment plans.
Diagnostic Imaging Technologies for Metastatic Disease
In the fight against cancer, diagnostic imaging technologies are key. They help doctors find where cancer has spread. This is vital for knowing the cancer’s stage and how to treat it.
Comparison of Imaging Modalities
Many imaging methods are used to find metastatic disease. Each has its own strengths and weaknesses. Common ones include CT scans, MRI, PET scans, and bone scans.
| Imaging Modality | Sensitivity | Specificity | Common Use |
| CT Scan | High | Moderate | Detecting metastases in lungs, liver, and lymph nodes |
| MRI | High | High | Evaluating metastases in the brain and spinal cord |
| PET Scan | High | High | Detecting metabolic activity of tumors, assessing spread |
| Bone Scan | Moderate | Low | Detecting bone metastases |
Each imaging method has its own strengths, making some better for certain types of metastases.
The Unique Role of PET Scans in Metastasis Detection
PET scans are vital for finding metastatic disease. They are very sensitive and specific. They are often used with CT and MRI to get a full picture of the disease.
“PET scans have revolutionized the field of oncology by enabling the early detection of metastatic disease, facilitating timely intervention.”
PET scans are great for finding metastasis because they show tumor activity. This is key for seeing how cancer has spread and planning treatment.
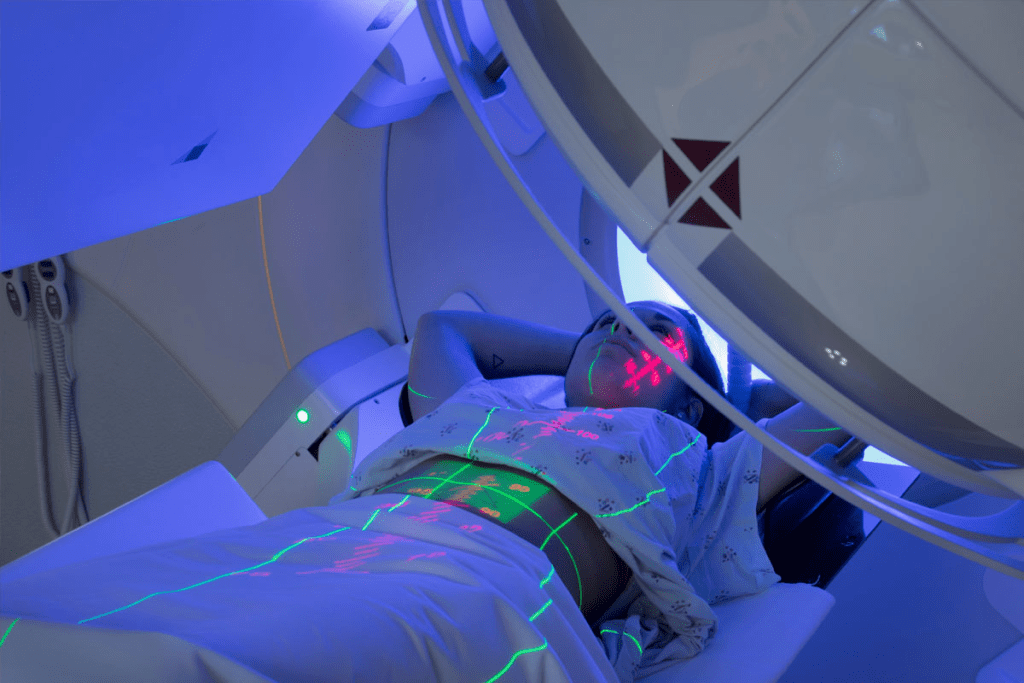
PET Scan Lifetime Limit: Understanding Radiation Exposure
PET scans are very useful for diagnosing diseases but they involve radiation. This radiation can add up if you have many scans. They are key in finding and tracking cancers, but the radiation is a big worry, mainly for those who have many scans.
How PET Scans Work
PET scans use a tiny bit of radioactive tracer, usually attached to glucose. This tracer is injected into your body. Cancer cells take in more glucose and tracer, so they show up on the scan.
The scanner picks up the radiation from the tracer. This creates detailed images of your body’s activity. It helps doctors see cancer cells and how far they’ve spread.
Radiation Dosage in Single PET Scan Procedures
The amount of radiation from one PET scan can vary. It usually is about 7 millisieverts (mSv). But it can be between 4 to 14 mSv or more, depending on the tracer and your size.
For comparison, you get about 3 mSv of background radiation each year from nature.
Cumulative Radiation Exposure Concerns
Getting more radiation over time is a worry because it raises the chance of cancer. While one scan is low risk, many scans can add up. For example, five scans could mean up to 35 mSv of radiation.
Doctors follow PET scan safety guidelines to lower risks. They use the least amount of tracer needed and make sure scans are done right. It’s important for patients to talk to their doctors about the risks and need for more scans.
The idea of a PET scan lifetime limit is about using them wisely. Knowing about the radiation and following safety rules helps doctors use scans safely and effectively.
Monitoring Protocols for Metastatic Cancer
Monitoring protocols are key in treating metastatic cancer. They help doctors track how the disease is growing and how well treatments are working. This way, they can change treatment plans as needed.
Frequency Guidelines for Different Cancer Types
The timing of monitoring varies with the cancer type and how fast it grows. For example, fast-growing cancers like pancreatic or lung cancer need more checks. Slower-growing cancers might not need as many.
| Cancer Type | Typical Monitoring Frequency |
| Pancreatic Cancer | Every 6-8 weeks |
| Lung Cancer | Every 8-12 weeks |
| Breast Cancer | Every 12-16 weeks |
PET Scan Surveillance Schedules
PET scans are vital for tracking metastatic cancer. They show how active tumors are. The timing of these scans depends on the cancer type and how it’s responding to treatment.
PET scan frequency changes based on the cancer and treatment results. For aggressive cancers, scans might be done more often.
Tailoring Monitoring to Individual Risk Profiles
Monitoring plans should match each patient’s risk level. This includes genetic factors, overall health, and past treatments. Personalized monitoring can lead to better care and outcomes for patients.
Balancing Diagnostic Benefits and Radiation Risks
PET scans are key in cancer diagnosis and monitoring. They offer insights into cancer growth and how well treatments work. But, they also come with radiation risks.
Medical Necessity Assessment
Assessing medical necessity is vital for using PET scans. This looks at the patient’s health history and current state. It also considers how the scan might affect treatment choices.
By doing this, doctors can reduce the amount of radiation patients get.
Risk-Benefit Analysis for Frequent Imaging
Doctors do a risk-benefit analysis for PET scans. They compare the scan’s benefits to its radiation risks. They think about the patient’s condition, how the scan might change treatment, and other monitoring options.
Table: Risk-Benefit Considerations for PET Scans
| Factors | Benefits | Risks |
| Diagnostic Accuracy | High sensitivity and specificity | Radiation exposure |
| Treatment Planning | Informs treatment decisions | Cumulative radiation dose |
| Monitoring Response | Assesses treatment efficacy | Potential for false positives |
Alternative Monitoring Methods
When deciding on PET scans, doctors also look at other options like MRI and CT scans. These can give important information with less radiation.
Healthcare providers aim to find the right balance. They assess medical need, do thorough risk-benefit checks, and explore other monitoring methods. This way, they can use PET scans while keeping radiation risks in check.
PET Scan Safety Protocols and Patient Precautions
PET scan safety is key to reduce radiation for patients. It involves careful preparation, precise execution, and considering each patient’s needs.
Preparing for a PET Scan Procedure
Patients must prepare before a PET scan. They need to fast, avoid hard activities, and remove metal items or jewelry. Proper preparation is vital for accurate results and less need for repeat scans, which lowers radiation exposure.
Strategies for Minimizing Radiation Exposure
Healthcare providers use the least amount of radiotracer needed for scans. Advances in PET scan technology have made doses lower without losing image quality. Sometimes, other imaging methods are used to cut down exposure even more.
Special Considerations for Patients Requiring Frequent Scans
Patients needing many PET scans, like those with metastatic cancer, get extra care. Doctors balance scan benefits against risks and look for other ways to monitor. Customized monitoring plans help keep radiation low while getting needed info.
Following PET scan safety rules and patient precautions helps. Healthcare providers make sure patients get the scan’s benefits with less radiation.
Treatment Approaches for Deadly Metastatic Cancers
It’s important to know the different ways to treat metastatic cancers to help patients. Treating metastatic disease needs a plan that uses many treatments.
Standard Treatment Protocols by Cancer Type
How we treat metastatic cancers depends on where the cancer started. For example, breast cancer might get hormone therapy, chemotherapy, or targeted therapy. Lung cancer might need chemotherapy, targeted therapy, and immunotherapy. It’s key to tailor treatment to the cancer type and the patient’s needs.
The right treatment also depends on the patient’s health, genetic mutations, and past treatments. For instance, colorectal cancer might get targeted therapies based on genetic changes.
Emerging Targeted Therapies for Metastatic Disease
Targeted therapies have changed how we treat metastatic cancers. They focus on specific cancer growth drivers. These therapies are often more effective and have fewer side effects than traditional chemotherapy. For example, HER2-targeted therapies help with breast cancer, and EGFR inhibitors work for lung cancer.
Immunotherapy Approaches
Immunotherapy uses the body’s immune system to fight cancer. It’s a promising treatment for many metastatic cancers. Checkpoint inhibitors, like pembrolizumab, are effective against melanoma, lung cancer, and more.
Role of Imaging in Treatment Planning and Response Assessment
Imaging is key in managing metastatic cancers. It helps in diagnosis, treatment planning, and checking how well treatments work. PET scans are great for seeing how active tumors are and if treatments are working.
By combining imaging with clinical data, doctors can make better treatment choices. This helps improve patient care.
Conclusion
Metastatic cancer is a big challenge in fighting cancer. Some types are very deadly. It’s important to know how cancer spreads and what makes it deadly.
PET scans help find and track cancer that has spread. But, we must think about the limits of PET scans and the risks of radiation. Following guidelines for PET scans helps balance the benefits and risks.
Healthcare providers can improve care by focusing on each patient’s needs. New treatments like targeted therapies and immunotherapy give hope to those with deadly cancers.
Monitoring cancer well means knowing about PET scans and following the right steps. As technology gets better, we need to keep improving PET scan rules. This will help patients get better care.
FAQ
What is metastatic cancer and how does it affect mortality rates?
Metastatic cancer is when cancer spreads to other parts of the body from where it started. It makes treatment harder and raises mortality rates.
How does metastasis occur, and what are the common sites where it occurs?
Cancer cells break away and travel through the body to form new tumors. Common places for these new tumors are the lungs, liver, bones, and brain.
What is the role of PET scans in detecting metastatic disease?
PET scans help find metastatic disease by showing where cancer cells are. They do this by highlighting areas of high activity in the body.
What are the deadliest metastatic cancers, and what are their metastatic patterns?
Pancreatic, lung, and liver cancers, along with brain metastases, are among the deadliest. Each type spreads differently, like pancreatic cancer often going to the liver and lungs.
How do PET scans work, and what is the radiation dosage involved?
PET scans use a radioactive tracer that goes to cancer cells. The dose of radiation varies based on the scan and the patient’s health.
What are the concerns related to cumulative radiation exposure from PET scans?
Too much radiation from PET scans can harm, including causing cancer. But, the benefits of these scans in tracking cancer are usually greater than the risks.
Is there a PET scan lifetime limit, and how is it determined?
There’s no strict limit on PET scans, but guidelines suggest using them wisely. This means choosing them only when needed and considering each patient’s risk.
How often should PET scans be performed for monitoring metastatic cancer?
How often PET scans are needed depends on the cancer type, its stage, and how well the patient responds to treatment. Doctors adjust the frequency based on each patient’s situation.
What are the safety protocols and patient precautions for PET scans?
PET scans follow strict safety rules. This includes preparing patients right, keeping radiation low, and special care for those needing many scans, like kids and pregnant women.
How do treatment approaches for deadly metastatic cancers involve imaging, particular PET scans?
Treatment for metastatic cancers often uses imaging, like PET scans, to check how well treatments work. New treatments also rely on imaging to see if they’re effective.
What are the alternative monitoring methods to PET scans, and when are they used?
Instead of PET scans, doctors might use CT scans, MRI scans, or ultrasound. These are chosen when PET scans aren’t needed or to lower radiation exposure.
How is the risk-benefit analysis performed for frequent PET scans?
For frequent PET scans, doctors weigh the benefits of diagnosis against the risks of radiation. This decision is made for each patient, considering their health and risk factors.
References (APA Style) You Can Use
- Quinn, B., Keevil, S., Harper, P., et al. (2016). Radiation dosimetry of ^18F-FDG PET/CT. BMC Medical Imaging, 16, Article 14.https://bmcmedimaging.biomedcentral.com/articles/10.1186/s12880-016-0143-y
- Nievelstein, R. A. J., et al. (2012). Radiation exposure and mortality risk from CT and PET. Radiation Protection Dosimetry / PMC. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC3411290/
- Hosono, M., et al. (2021). Cumulative radiation doses from recurrent PET“CT imaging. PMC. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC9328066/ PMC
- Stiles, B. M., et al. (2011). Cumulative Radiation Dose From Medical Imaging in PET-CT Surveillance Protocols. Annals of Thoracic Surgery. Retrieved from https://www.annalsthoracicsurgery.org/article/S0003-4975(11)00782-X/fulltext