Last Updated on November 26, 2025 by Bilal Hasdemir

Learn physical exam test for gallbladder like Murphy’s sign and how it helps detect inflammation. Accurate diagnosis of gallbladder conditions is key to effective treatment. At Liv Hospital, we stress the need for a detailed physical examination to spot gallbladder problems. One essential tool we use is Murphy’s sign, a simple yet critical test for gallbladder inflammation.
Murphy’s sign is very important for diagnosing acute cholecystitis, a condition that needs quick medical care. Knowing how to do Murphy’s sign and what it means helps doctors make better decisions for their patients. In this article, we’ll explore Murphy’s sign, its importance, and how it’s done.
Key Takeaways
- Murphy’s sign is a key tool for diagnosing gallbladder inflammation.
- It’s very useful for spotting acute cholecystitis.
- Understanding Murphy’s sign helps in quick and effective patient care.
- The test requires a specific technique that doctors should know.
- Using Murphy’s sign correctly can greatly improve treatment results.
The Significance of Gallbladder Assessment in Clinical Practice
Gallbladder assessment is key in clinical practice. It helps in diagnosing and managing gallbladder disease. Evaluating gallbladder health is vital for patient care and outcomes.
Prevalence of Gallbladder Disease in the United States
Gallbladder disease is common in the United States. Millions of Americans have gallstones and other issues. This leads to high healthcare costs and suffering.
The risk of gallbladder disease grows with age. It’s more common in women and those with certain genes. Knowing this helps doctors find and help at-risk patients.
Role of Physical Examination in Diagnosis
Physical examination is vital in diagnosing gallbladder disease. Techniques like Murphy’s sign are used. We use history, physical findings, and tests to diagnose and manage gallbladder issues.
Physical exams play a big role in diagnosis. They help find patients who need more tests and rule out other pain causes. A detailed physical exam is key for quality care.
Anatomical Foundations: Understanding Murphy’s Point
To do Murphy’s sign right, you need to know where Murphy’s point is. This is key for checking gallbladder health.
Location of the Gallbladder and Murphy’s Point
Murphy’s point is in the right upper part of the belly. It matches where the gallbladder is. The gallbladder is shaped like a pear and sits under the liver.
To find Murphy’s point, draw a line from the belly button to the right ninth rib. Where this line hits the rib is Murphy’s point.
The spot of Murphy’s point is important. It’s where the gallbladder touches the belly wall. This makes Murphy’s sign a good way to find gallbladder problems.
Relationship to Surrounding Structures
The gallbladder is close to other parts of the body. It’s under the liver, with a duct linking it to the common bile duct. Knowing this helps us see why Murphy’s point is important.
The liver is above the gallbladder, and the transverse colon is below it. These close relationships can make diagnosing gallbladder issues tricky.
Understanding the anatomical foundations of Murphy’s point helps doctors diagnose gallbladder diseases better. This knowledge is key for doing Murphy’s sign and understanding its results.
Pathophysiology of Acute Cholecystitis
Understanding the inflammation process in acute cholecystitis is key to diagnosing and treating it. This condition involves inflammation of the gallbladder, usually caused by gallstones blocking the cystic duct. This blockage triggers a series of inflammatory responses.
The inflammation process starts when the cystic duct is blocked. This blockage stops bile from leaving the gallbladder. The gallbladder then gets distended, causing pressure to rise. This pressure makes the gallbladder wall inflamed, starting the inflammation.
Inflammation Process in the Gallbladder
Inflammation in acute cholecystitis means inflammatory cells move into the gallbladder wall. These cells release chemicals that make the inflammation worse. The gallbladder wall swells, and parts may die due to high pressure and poor blood flow.
Why Pain Occurs During Murphy’s Sign
Pain during Murphy’s sign happens because of the gallbladder’s inflammation and its close location to the front of the belly. When a doctor does Murphy’s sign, they press on the gallbladder area. In someone with acute cholecystitis, this pressing causes pain, mainly when they take a deep breath. This is because the inflamed gallbladder touches the doctor’s fingers.
The pain comes from the increased sensitivity of the inflamed gallbladder to touch and the irritation of the surrounding tissue. A positive Murphy’s sign shows the gallbladder is inflamed. It’s a helpful sign for doctors to diagnose acute cholecystitis.
The Complete Physical Exam Test for Gallbladder
Checking the gallbladder’s health needs a careful plan. A full physical exam is key to spotting gallbladder problems. We use inspection, percussion, and palpation to do this.
Initial Inspection and Percussion Techniques
We start by checking the belly area closely. We look for jaundice, swelling, or old surgery scars. Then, we use percussion to find pain in the right upper belly.
Percussion is tapping the belly gently to find sore spots. It helps us see if there’s gallbladder trouble. We start far from the problem and move closer.
Murphy’s Sign as the Cornerstone Assessment
Murphy’s sign is a key test for gallbladder issues, like acute cholecystitis. It checks for pain in the right upper belly when you breathe deeply. If the patient can’t breathe deeply because of pain, it’s a positive sign.
To do Murphy’s sign right, we place our hands just so and tell the patient what to expect. The patient’s reaction tells us a lot about gallbladder inflammation.
Additional Gallbladder Examination Maneuvers
There are more tests to check the gallbladder’s health. These include sonographic Murphy’s sign and other touch tests.
We also check for pain that spreads to the right shoulder or if the belly is tight in the right area. These tests help us understand the gallbladder’s health better.
By using all these methods, we get a full picture of the gallbladder’s health. This helps us decide on the next steps, like more tests or treatment.
Step-by-Step Guide to Performing Murphy’s Sign
Murphy’s sign is a key tool in diagnosing gallbladder issues. It needs careful technique and the patient’s full cooperation. Healthcare pros must know how to position their hands, give clear instructions, and coordinate breathing.
Proper Hand Positioning Techniques
To start, find Murphy’s point at the right costal margin and mid-clavicular line. Place your fingers under the rib cage at this spot, but don’t press too hard at first.
The right hand placement is:
- Put your fingertips under the right costal margin
- Avoid pressing too hard on the abdomen
- Keep a firm but gentle touch on the abdominal wall
Patient Instructions and Communication
Talking clearly with the patient is essential. Tell them to:
- Take a deep breath in
- Hold their breath at the highest point
- Slowly exhale
Watch how the patient reacts to the touch, looking for any pain or tenderness when they inhale.
Respiratory Coordination During the Test
Getting the patient to breathe right is important for a good Murphy’s sign. When they inhale deeply, the gallbladder moves towards your fingers. If it’s inflamed, this will hurt, and they’ll stop breathing.
Here’s a quick guide to Murphy’s sign:
| Step | Description | Patient Response |
| 1 | Find Murphy’s point and position fingers | Patient relaxes abdominal muscles |
| 2 | Tell the patient to take a deep breath | Gallbladder descends towards fingers |
| 3 | Look for pain or tenderness | Patient may stop breathing if in pain |
By following these steps and watching the patient’s reactions, doctors can do Murphy’s sign right and get important info.
Interpreting Results: What a Positive Murphy Sign Means
Understanding a positive Murphy’s sign is key for correct diagnosis. A positive sign during a physical exam means the gallbladder is inflamed, known as acute cholecystitis.
Classic Positive Response Characteristics
A classic positive Murphy’s sign shows pain in the right upper abdomen when deep breathing. This pain is sharp and can stop the patient from breathing in fully.
The signs of a positive response are:
- Pain in the right upper quadrant
- Pain gets worse with deep breathing
- Patient might pause breathing
Grading the Intensity of Response
How much pain a patient feels from Murphy’s sign matters. The pain can range from a little discomfort to very severe.
| Grade | Description |
| 1+ | Mild tenderness |
| 2+ | Moderate pain |
| 3+ | Severe pain with inspiratory arrest |
Differentiating True Positives from False Positives
Telling true positives from false positives is critical for correct diagnosis. A true positive Murphy’s sign means the gallbladder is actually sick, like with acute cholecystitis.
False positives happen when other issues, like hepatitis or pneumonia, cause pain in the right upper quadrant. We must look at the whole clinical picture, including lab tests and scans, to tell them apart.
By carefully looking at Murphy’s sign and the patient’s overall health, we can make better diagnoses. This helps us create the right treatment plans.
Murphy’s Percussion Test and Other Variations
The field of diagnosing gallbladder disease has grown with new methods. These include percussion tests and sonographic assessments. These tools help doctors better diagnose and treat gallbladder issues.
Technique for Murphy’s Percussion Test
Murphy’s percussion test is a useful twist on Murphy’s sign. It uses percussion to check for gallbladder tenderness. First, we find Murphy’s point and then apply a percussive motion to see if it hurts.
- Identify Murphy’s point on the patient.
- Apply gentle percussion at this site.
- Assess the patient’s response for tenderness.
This method is great for cases where the traditional Murphy’s sign is hard to use.
Sonographic Murphy’s Sign in Ultrasound Assessment
Ultrasound technology has introduced the sonographic Murphy’s sign. It uses ultrasound to see the gallbladder while applying pressure with the probe.
- Visualize the gallbladder using ultrasound.
- Apply pressure with the probe over the gallbladder.
- Assess for tenderness and visualize any changes.
This method has been found to improve the accuracy of diagnosing acute cholecystitis.
Comparative Effectiveness of Different Techniques
Research has looked into how well Murphy’s sign, Murphy’s percussion test, and sonographic Murphy’s sign work. Sonographic Murphy’s sign is often seen as more precise because it lets doctors see the gallbladder directly.
| Technique | Sensitivity | Specificity |
| Murphy’s Sign | 80% | 85% |
| Murphy’s Percussion Test | 82% | 88% |
| Sonographic Murphy’s Sign | 90% | 92% |
Knowing how each method compares helps doctors pick the best one for each situation. This depends on the patient’s needs and what resources are available.
Diagnostic Accuracy and Clinical Utility
Understanding Murphy’s sign’s clinical utility means looking at its sensitivity, specificity, and predictive values. It’s a key tool in diagnosing acute cholecystitis. Yet, its accuracy can change based on several factors.
Sensitivity and Specificity Data Analysis
Research shows Murphy’s sign’s sensitivity ranges from 44 to 97 percent. Specificity ranges from 48 to 96 percent for acute cholecystitis. This wide range comes from different patient groups, examiner skills, and complicating factors.
This variability shows the importance of considering Murphy’s sign with the patient’s overall symptoms. A positive sign suggests gallbladder disease but should be checked with other signs.
Positive and Negative Predictive Values
The positive predictive value (PPV) of Murphy’s sign varies with disease prevalence. The negative predictive value (NPV) also changes with disease prevalence. This is important for making decisions on further testing and treatment.
In practice, knowing the PPV and NPV of Murphy’s sign helps in making informed decisions. This is key for further testing and treatment plans.
Integration with Laboratory Findings
Murphy’s sign is often used with lab results to improve accuracy. High white blood cell counts, liver enzymes, and bilirubin levels support acute cholecystitis diagnosis. This is when Murphy’s sign is positive.
Using Murphy’s sign with lab results and imaging gives a full picture of the patient’s condition. This helps doctors choose the best treatment options.
Special Patient Populations and Adaptations
When doing Murphy’s sign, we must think about different patient needs. Each group might need special adjustments in how we do the test or what we look for.
Technique Modifications for Elderly Patients
Elderly patients face special challenges, like less muscle and different pain feelings. When doing Murphy’s sign on them, we need to be careful but firm. A study in the Journal of the American Geriatrics Society shows that older adults with cholecystitis might not show typical symptoms. So, we must adjust our technique.
Approach to Pregnant Women
Pregnant women need special care because of changes in their body. The growing uterus can move organs around, changing where Murphy’s point is. We should adjust our touch and watch for pain that isn’t where it seems.
Challenges and Solutions for Obese Patients
Obese patients can be tough because their belly is thicker. This might mean we need to press deeper. But we also don’t want to hurt them. A study compared different ways to do Murphy’s sign on obese patients:
| Technique | Success Rate in Obese Patients | Patient Comfort Level |
| Standard Murphy’s Sign | 70% | 6/10 |
| Modified Deep Palpation | 85% | 7/10 |
| Sonographic Murphy’s Sign | 90% | 8/10 |
Pediatric Considerations
When doing Murphy’s sign on kids, we must think about their age, size, and how well they can help. Young kids might need a gentler, simpler way because they’re smaller and might not point to pain well. Being kind and easy to understand is key.
In short, making Murphy’s sign work for all patients is key to good care. By knowing what each group needs, we can do better for everyone.
Common Errors and Troubleshooting
To ensure reliability, it’s key to know the common errors with Murphy’s sign. This tool is valuable but only works well with the right technique and understanding.
Improper Hand Placement Issues
One big mistake is improper hand placement. We must place our fingers correctly at Murphy’s point. This spot is where the right costal margin meets the lateral border of the rectus sheath. Wrong placement can lead to wrong results, affecting the test’s accuracy.
To fix hand placement issues, first find Murphy’s point. Look for the right ninth costal cartilage and place your fingers there. Make sure your pressure is firm but not too hard, to avoid hurting the patient.
Patient Cooperation Challenges
Getting patient cooperation can be tough. Patients might find it hard to hold their breath or might be in too much pain. This makes it hard to get a clear reading.
To solve this, explain the test clearly to the patient. Show them how it’s done or use a gentle approach to make them feel at ease.
Interpretation Pitfalls
Even with the right technique, there are pitfalls in interpretation. For example, a patient with another condition might show a positive sign, leading to a wrong diagnosis.
To steer clear of these issues, look at the patient’s whole situation. Use Murphy’s sign along with other tests like imaging studies and laboratory tests to confirm the diagnosis.
Knowing these common errors and how to fix them can make Murphy’s sign more reliable in medical practice.
Clinical Decision Making After Murphy’s Sign Assessment
Murphy’s sign is a key moment in deciding what tests and treatments to use. If a patient gets a positive result, it means they likely have acute cholecystitis. This leads to important decisions about what to do next.
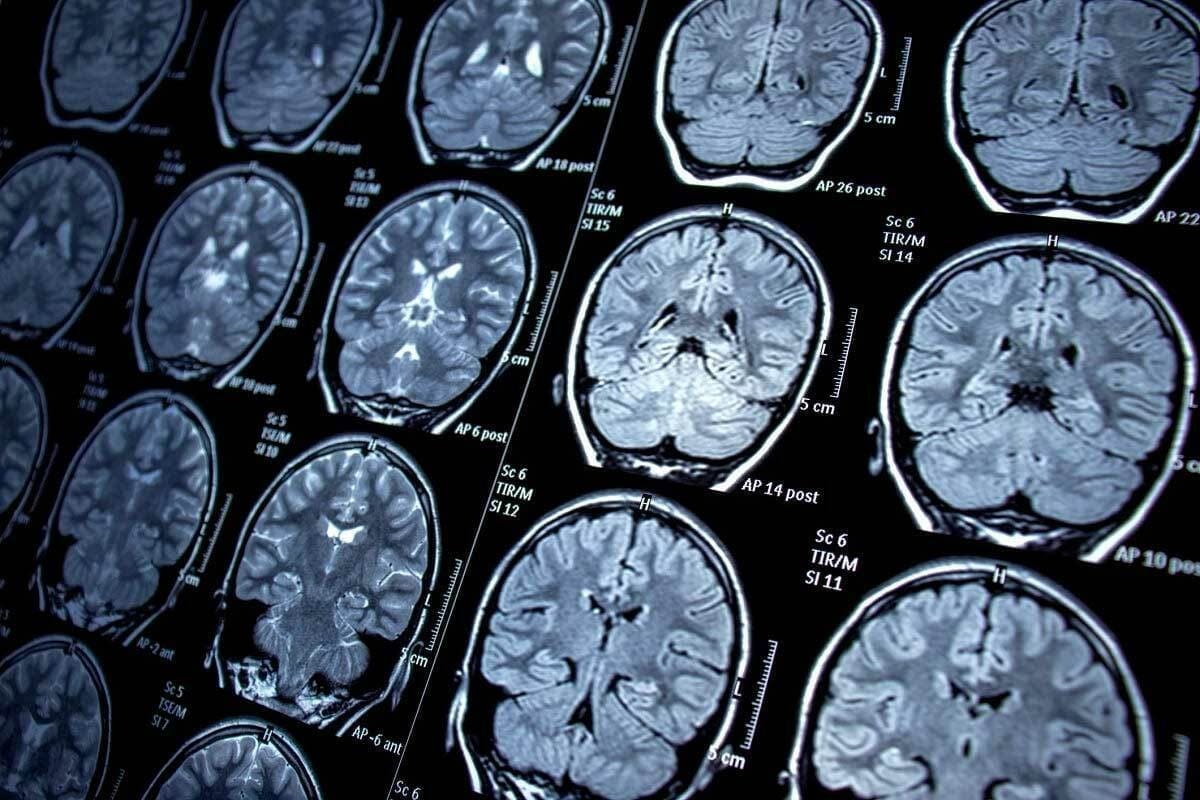
Appropriate Follow-up Diagnostic Tests
After a positive Murphy’s sign, we suggest certain tests to confirm the diagnosis and check how severe it is:
- Ultrasound examination to see gallstones, inflammation, and other issues.
- Laboratory tests, like complete blood count (CBC), liver function tests, and pancreatic enzymes, to check for inflammation and rule out other problems.
- CT scan or MRI in some cases to look at the gallbladder and nearby areas more closely.
These tests help us make sure we have the right diagnosis and plan the best treatment.
Treatment Pathways Based on Findings
The treatment plan for a patient with a positive Murphy’s sign depends on how severe the condition is and if there are any complications. Common treatments include:
- Initial stabilization with fluids and pain relief.
- Antibiotic therapy to treat or prevent infection.
- Surgical consultation for possible cholecystectomy, which can be immediate or delayed based on the patient’s condition and how they respond to initial treatment.
In some cases, treatments like percutaneous cholecystostomy might be considered for patients who are at high risk for surgery.
When to Consult Surgical Specialists
We advise talking to surgical specialists in certain situations:
- Severe acute cholecystitis with signs of gangrene or perforation.
- When conservative management doesn’t work.
- When there are complications like cholangitis or pancreatitis.
Getting surgical advice early is key for the best outcomes in complicated gallbladder disease.
Conclusion: Integrating Murphy’s Sign into Modern Clinical Practice
We’ve looked into how Murphy’s sign helps check for gallbladder inflammation, like in acute cholecystitis. This method is a key tool in diagnosing, thanks to its use with today’s medical tests.
Using Murphy’s sign in today’s medicine makes diagnosing better. It works well with scans and blood tests. This combo gives a full picture of a patient’s health, leading to quicker and more effective treatments.
It’s important for doctors to keep up with Murphy’s sign. Even as medical tech gets better, skills like this are just as vital.
By mixing old-school physical checks with new tech, we improve patient care. Using Murphy’s sign shows how medicine keeps getting better. It combines the old with the new for the best care.
FAQ
References
Pietrangelo, A. (2024). Managing weight loss after gallbladder removal. Medical News Today. Retrieved from
https://www.medicalnewstoday.com/articles/317659
Dahmiwal, T., et al. (2024). Dietary considerations in cholecystectomy. Journal of Gastrointestinal Surgery, 28(5), 345-350. Retrieved from