Last Updated on December 2, 2025 by Bilal Hasdemir
Did you know that pituitary tumors are among the most common brain tumors? They affect thousands of people worldwide each year. Surgery is often needed to treat them. A craniotomy is a surgery that lets doctors remove these tumors.Learn what a pituitary tumor craniotomy is. Understand the specific surgical approaches used to access tumors in this area clearly.
Thinking about surgery can be scary. We want to help you understand what to expect from a pituitary tumor surgery. In this article, we’ll talk about the procedure, its importance, and what recovery is like.
Key Takeaways
- Craniotomy is a surgical procedure used to remove complex pituitary tumors.
- Pituitary adenoma surgery is often necessary to alleviate symptoms and prevent further complications.
- Understanding the procedure and its risks can help you prepare for a successful outcome.
- Our team is dedicated to providing comprehensive care and support throughout your treatment journey.
- A successful surgery can significantly improve your quality of life.
Understanding Pituitary Tumors
To understand pituitary tumors, you need to know about the pituitary gland. It’s a key part of the endocrine system. It’s called the “master gland” because it controls many important hormones in our bodies.
Function of the Pituitary Gland
The pituitary gland is a small gland at the brain’s base. It helps control many body functions by making hormones. For example, it makes growth hormone for growth and adrenocorticotropic hormone (ACTH) to help the adrenal glands make cortisol.
The gland has two parts: the anterior and posterior pituitary. The anterior part makes hormones that control other glands. The posterior part releases hormones made by the hypothalamus.
Types of Pituitary Tumors
Pituitary tumors are divided by their hormone activity and size. Functioning tumors make too much hormone, causing health problems. Non-functioning tumors don’t make hormones but can still cause issues because of their size and pressure.
- Functioning Tumors: These include prolactinomas, growth hormone-secreting tumors (leading to acromegaly), and ACTH-secreting tumors (leading to Cushing’s disease).
- Non-functioning Tumors: These tumors can grow large and cause symptoms by pressing on nearby structures, like the optic chiasm, leading to vision problems.
Prevalence and Risk Factors
Pituitary tumors are rare, making up about 10% of brain tumors. They affect about 80-100 people per 100,000. Genetic conditions like Multiple Endocrine Neoplasia Type 1 (MEN1) raise the risk.
Other risk factors include family history and genetics. Knowing these can help find and treat tumors early.
“Early diagnosis and proper treatment of pituitary tumors are key to avoiding long-term health issues and improving life quality for those affected.”
Signs and Symptoms of Pituitary Tumors

Pituitary tumors can show many symptoms. Knowing these signs is key to getting help early. We’ll look at the different symptoms these tumors can cause.
Hormone-Related Symptoms
Pituitary tumors can mess with hormone levels. This can lead to too much or too little of certain hormones. For example, it might cause hyperthyroidism or hypothyroidism.
Other symptoms include changes in menstrual cycles, fertility problems, and issues with sex drive.
Pressure-Related Symptoms
As a tumor grows, it can press on nearby areas. This can cause headaches, vision problems, and even nerve damage. In some cases, it can also cause hydrocephalus, where fluid builds up in the brain.
When to Seek Medical Attention
If you have symptoms that won’t go away, see a doctor. Early treatment can make a big difference. Look out for headaches, vision changes, or hormonal issues. If you notice these, get checked by a healthcare expert.
Diagnosis of Pituitary Tumors
Healthcare professionals use many tools to diagnose pituitary tumors. They look at clinical signs, use imaging studies, and do lab tests. These steps help find out if a tumor is there and what it’s like.
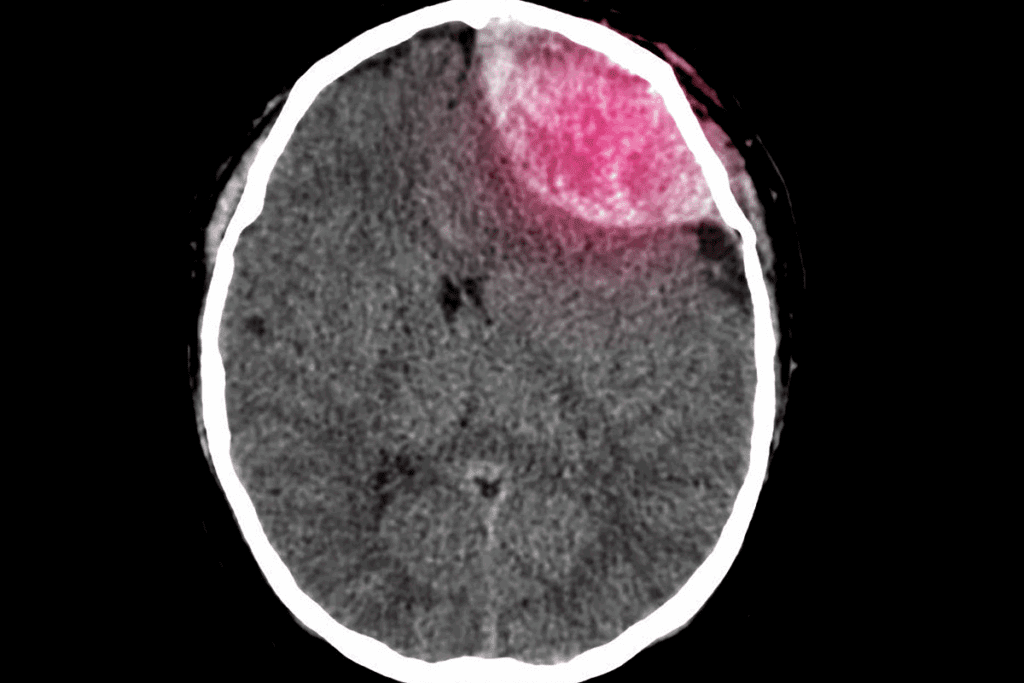
Imaging Studies
Imaging is key for finding pituitary tumors. MRI is the main tool. It shows the gland and nearby areas clearly. MRI helps see the tumor’s size, where it is, and how it affects nearby parts.
Hormone Testing
Hormone tests are also important. Pituitary tumors can change hormone levels. Blood tests check hormones like prolactin and growth hormone. This shows how the tumor affects the body’s hormones.
Visual Field Testing
Visual field tests check how the tumor affects sight. Tumors can press on the optic chiasm, causing vision problems. This test shows how much vision is affected and helps plan treatment.
| Diagnostic Test | Purpose |
| MRI | To visualize the pituitary tumor and its relationship with surrounding structures |
| Hormone Testing | To assess the impact of the tumor on hormone production |
| Visual Field Testing | To evaluate any visual disturbances caused by the tumor |
In conclusion, diagnosing pituitary tumors takes several steps. Imaging, hormone tests, and visual field tests are used together. This way, doctors can accurately find and understand tumors. They then make the best treatment plans.
Treatment Options for Pituitary Tumors
Managing pituitary tumors involves several methods. These include watching the tumor, using medication, radiation, and surgery. The right treatment depends on the tumor’s type, size, and location. It also depends on the patient’s health and what they prefer.
Observation (Watchful Waiting)
For small, non-active tumors that don’t cause symptoms, watchful waiting might be chosen. This means regular checks with imaging and hormone tests. It helps catch any changes or symptoms.
Medication Therapy
Medication is often the first step for active tumors, like prolactinomas. Dopamine agonists like bromocriptine and cabergoline help control hormone levels and shrink the tumor. Other medications are used for different types of tumors.
Radiation Therapy
Radiation therapy is used for tumors that can’t be fully removed by surgery. It’s also for tumors that come back or grow quickly. SRS and fractionated radiotherapy deliver precise radiation to the tumor, protecting nearby tissues.
Overview of Surgical Approaches
Surgery is a main treatment for many pituitary tumors, especially those causing symptoms or vision problems. The most common method is the transsphenoidal approach, through the sphenoid sinus. Other methods, like craniotomy, might be used based on the tumor’s details and location.
Choosing a treatment plan for a pituitary tumor is very personal. It needs a team of doctors, including neurosurgeons, endocrinologists, and radiation oncologists. They work together to find the best treatment.
Results from treatment can differ based on the tumor and the patient’s health. It’s important to keep up with regular check-ups. This helps see if the treatment is working and to handle any issues or changes in the tumor.
- Key Considerations:
- Tumor type and size
- Patient’s overall health
- Presence of symptoms
- Potential treatment side effects
What is a Pituitary Tumor Craniotomy?
Understanding craniotomy for pituitary tumors is key for patients. A craniotomy is a surgery where part of the skull is removed to access the brain. This method helps surgeons reach tumors that are big or complex.
Definition and Purpose
A pituitary tumor craniotomy is a surgery where the skull is partially removed to get to the pituitary gland. The main goal is to remove the tumor safely without harming nearby important areas. This is especially useful for big tumors or those putting pressure on the brain.
This surgery aims to remove the tumor safely, reducing the risk of damage. The choice to do a craniotomy depends on the tumor’s size, location, and the patient’s health.
When is a Craniotomy Recommended
A craniotomy is usually suggested for patients with:
- Large or giant tumors
- Complex or irregularly shaped tumors
- Tumors causing a lot of pressure on the brain
- Tumors not responding to other treatments
According to the American Cancer Society, craniotomy is often chosen for bigger or more complex tumors. These can’t be safely removed through other methods.
| Tumor Characteristics | Craniotomy Recommendation |
| Large or Giant | Highly Recommended |
| Complex or Irregular Shape | Recommended |
| Significant Pressure on Brain Structures | Highly Recommended |
Comparison with Transsphenoidal Approach
The transsphenoidal approach is another way to remove pituitary tumors. It goes through the sphenoid sinus to get to the gland, without removing skull parts. It’s less invasive and better for smaller tumors, but not for bigger ones.
“The choice between craniotomy and transsphenoidal surgery depends on the tumor’s characteristics and the patient’s condition. Craniotomy offers a more direct access for complex cases, while transsphenoidal surgery is less invasive and often results in quicker recovery.” – Expert Neurosurgeon
We compare these methods to find the best treatment for each patient. The table below shows the main differences:
| Characteristics | Craniotomy | Transsphenoidal Approach |
| Invasiveness | More invasive | Less invasive |
| Tumor Size Suitability | Large or complex tumors | Smaller tumors |
| Recovery Time | Generally longer | Generally shorter |
Types of Craniotomy Approaches for Pituitary Tumors
Neurosurgeons use different craniotomy methods for pituitary tumor surgery. They pick the best approach based on the tumor’s size and where it is. The patient’s health also plays a big role in the choice.
Pterional (Frontotemporal) Approach
The pterional or frontotemporal approach is a common method. It involves an incision in the frontotemporal area. This gives a clear view of the tumor site.
This approach is great for tumors that go beyond the sella turcica.
Subfrontal Approach
The subfrontal approach goes through the frontal lobe to reach the tumor. It’s good for tumors that spread up into the suprasellar area. This method offers a straight path to the tumor for removal.
Supraorbital Keyhole Approach
The supraorbital keyhole approach is a small incision above the eyebrow. It’s less invasive and leads to quicker recovery. It’s best for tumors that are easy to get to.
Each craniotomy method has its own use and benefits. The right technique depends on the patient’s specific situation. Knowing about these approaches helps patients understand the complexity of pituitary tumor surgery.
Preparing for Pituitary Tumor Surgery
Pituitary tumor surgery needs careful planning. This includes a detailed medical check-up and changes to your medicines. Knowing what to do can make you feel more at ease and ready for the surgery.
Medical Evaluation
Getting a full medical check-up is key before surgery. Your doctor will look at your health history and current status. They might also check for any past treatments or surgeries.
They will run tests like blood work and imaging scans. These help understand your health and the tumor better. This information helps your doctor plan the surgery just for you.
Tell your doctor about all the medicines you’re taking. This includes any supplements or over-the-counter drugs. These can affect your surgery and how you recover.
Medication Adjustments
You might need to change your medicines before surgery. Some drugs, like blood thinners, could increase bleeding risks. Your doctor will tell you which medicines to stop or change and when.
If you’re on hormone therapy or other tumor-related medicines, your doctor might adjust them. It’s important to follow these changes carefully. This ensures your safety during the surgery.
Preoperative Instructions
You’ll get detailed instructions from your healthcare team before surgery. These might cover fasting, hygiene, and what to bring to the hospital. You’ll also learn how to stay comfortable and safe before surgery.
| Preoperative Instruction | Description |
| Fasting | Avoid eating or drinking for a specified period before surgery |
| Hygiene | Shower or bathe as instructed to minimize infection risk |
| Medications | Follow specific guidance on which medications to take or avoid before surgery |
By following these instructions and adjusting your medicines, you’ll be ready for your surgery. This preparation helps ensure the best outcome for you.
The Craniotomy Procedure Step by Step
We carry out the craniotomy procedure with great care. Each step is done with precision. The process includes several key stages, from giving anesthesia to closing the incision.
Anesthesia and Positioning
The first step is giving anesthesia. Our anesthesiology team makes sure the patient is comfortable and pain-free. The patient is then placed on the operating table for the best access to the pituitary gland.
Anesthesia for craniotomy is usually general anesthesia. This keeps the patient unconscious and pain-free during the surgery.
Incision and Bone Flap Removal
After the patient is set up, the surgical team makes an incision in the scalp. The incision’s size and location depend on the chosen approach. A bone flap is then removed to get to the brain.
Tumor Resection Process
With the bone flap off, the neurosurgeon carefully moves through the brain tissue to find the tumor. The goal is to remove as much of the tumor as possible while keeping healthy tissue safe.
Closure and Immediate Recovery
After removing the tumor, the surgical team closes the incision. The bone flap is put back, and the scalp is closed with sutures or staples. The patient is then moved to the recovery room for post-operative care.
| Stage | Description |
| Anesthesia and Positioning | Administration of anesthesia and patient positioning. |
| Incision and Bone Flap Removal | Incision in the scalp and removal of a bone flap. |
| Tumor Resection | Removal of the pituitary tumor. |
| Closure | Replacement of the bone flap and closure of the scalp. |
Knowing the steps of a craniotomy for a pituitary tumor can ease concerns. It helps prepare patients for their surgical journey.
Technological Advances in Pituitary Tumor Surgery
Technology has greatly improved pituitary tumor surgeries. New tools help neurosurgeons diagnose and treat these tumors better.
Neuronavigation Systems
Neuronavigation systems are key in pituitary tumor surgery. They use advanced imaging to guide surgeons in real-time. This makes the surgery more precise, reducing harm to nearby areas.
The main features of neuronavigation systems are:
- Real-time tracking of surgical instruments
- Advanced imaging integration for precise localization
- Enhanced visualization of complex anatomy
Intraoperative MRI
Intraoperative MRI is a big step forward in surgery. It lets surgeons see real-time MRI images during the surgery. This helps them check how much tumor they’ve removed and make changes if needed.
The benefits of intraoperative MRI are:
- Immediate assessment of surgical progress
- Enhanced ability to achieve complete tumor removal
- Reduced risk of complications
Endoscopic Assistance
Endoscopic assistance has changed pituitary tumor surgery for the better. It uses small incisions to see the tumor and surrounding areas. This approach is less invasive, leading to quicker recovery times.
The benefits of endoscopic assistance are:
- Minimally invasive approach reducing recovery time
- Improved visualization of the surgical site
- Enhanced precision in tumor resection
These technologies help neurosurgeons perform safer and more precise surgeries. This means safer and more effective treatments for patients.
Risks and Complications of Pituitary Craniotomy
Pituitary craniotomy is a key surgery for pituitary tumors. But, it also has risks and complications. It’s important to know about these risks.
Neurological Complications
Neurological issues can happen because of the surgery’s location. This area is close to important brain parts. These problems include:
- Stroke or Cerebral Vasospasm: Surgery can cause stroke or vasospasm.
- Seizures: Seizures can happen, though they are rare.
- Cerebrospinal Fluid (CSF) Leakage: CSF leakage is a complication that needs careful handling.
Endocrine Complications
The surgery can affect hormone balance. This can lead to endocrine problems, such as:
- Hypopituitarism: This is when the pituitary hormones are not made enough.
- Diabetes Insipidus: It’s a condition with too much thirst and urination because of ADH.
General Surgical Risks
Like any big surgery, pituitary craniotomy has general risks. These include:
- Infection: Infections can happen at the surgery site or system-wide.
- Bleeding: Bleeding can happen during or after surgery.
- Anesthesia-Related Complications: There are risks with the anesthesia used.
Long-term Considerations
Patients may face long-term challenges. These include:
- Recovery Time: Recovery times vary among people.
- Hormone Replacement Therapy: Some may need hormone therapy for life.
- Follow-Up Care: Regular check-ups with doctors are key for managing long-term issues.
It’s crucial for patients and families to understand these risks. Talking about these with a doctor is very important.
Recovery After Pituitary Tumor Craniotomy
The recovery after a pituitary tumor craniotomy has several stages. It starts with the hospital stay and ends when you return to normal life. Knowing what to expect can make the journey easier for patients and their families.
Hospital Stay Duration
The hospital stay after surgery can last from a few days to a week. This time varies based on your health, the surgery’s complexity, and any complications. “The length of hospital stay is key in recovery,” a neurosurgeon notes.
In the hospital, doctors watch your brain health, manage pain, and look for complications.
Pain Management
Managing pain is very important after surgery. Patients get medicine to help with pain, especially in the first days. We adjust pain plans as needed to keep you comfortable.
Good pain management helps you feel better and recover faster. It lets you move more and take part in your care.
Activity Restrictions
After surgery, you’ll need to avoid certain activities. These include heavy lifting, bending, and hard exercises. “Staying away from activities that raise brain pressure is key in the early recovery,” a healthcare expert says.
You’ll start doing normal activities again slowly, based on your surgeon’s advice. This usually happens a few weeks after surgery.
Return to Normal Life
How long it takes to get back to normal varies. Most people need several weeks to a few months to fully recover. Regular check-ups with your healthcare team are important to track your progress and address any issues.
With the right care and following instructions, most people can recover well and return to their usual activities.
Post-Operative Care and Follow-Up
After a craniotomy for pituitary tumors, post-operative care and follow-up are key. They greatly affect the patient’s recovery and quality of life.
Wound Care
Keeping the surgical site clean and dry is crucial. It helps prevent infection and promotes healing. Always follow the wound care instructions from your healthcare team.
Hormone Replacement Therapy
Many patients need hormone replacement therapy (HRT) after surgery. This is especially true if the tumor affected hormone production. HRT helps restore normal hormone levels, easing symptoms like fatigue and hormonal imbalances.
Hormone Replacement Therapy Considerations:
| Hormone | Function | Replacement Therapy |
| Thyroid Hormone | Regulates metabolism | Synthroid (levothyroxine) |
| Cortisol | Stress response, metabolism | Hydrocortisone |
| Growth Hormone | Growth and development | Somatropin |
Follow-Up Imaging
Regular imaging is vital to watch for tumor recurrence or changes in the pituitary gland. MRI scans are often used. The scan frequency varies based on the case and the surgeon’s advice.
Long-term Monitoring
Long-term monitoring is about regular check-ups with your healthcare team. They check hormone levels, visual function, and any long-term surgery effects. It’s crucial to stick to your follow-up schedule for timely issue management.
It’s essential for patients to adhere to their follow-up schedule to ensure timely detection and management of any potential issues.
Cost and Insurance Considerations in the United States
It’s important for patients to know about the money side of pituitary surgery. The costs can be high, and figuring out insurance and financial help is key. This helps in planning the treatment.
Typical Costs of Pituitary Surgery
The price of pituitary surgery changes based on many things. These include how complex the surgery is, the surgeon’s fees, hospital costs, and insurance. On average, it can cost from $30,000 to over $100,000. Here are the main parts that add up to the total cost:
- Surgeon’s Fees: These depend on the surgeon’s experience and the surgery’s complexity.
- Hospital Charges: This includes the cost of the hospital stay, operating room, and other expenses.
- Anesthesia Fees: The price for anesthesia during the surgery.
- Diagnostic Tests: Costs for imaging studies, hormone tests, and other diagnostic procedures.
Insurance Coverage
Most insurance in the U.S. covers pituitary surgery, but how much can vary. It’s important for patients to check their insurance to know what’s covered and what they’ll have to pay. Key things to look at include:
- Deductibles and Coinsurance: The amount to pay before insurance starts and the percentage of costs after.
- Pre-authorization Requirements: Some plans need approval before certain treatments or procedures.
- Network Providers: Using providers in your network can lower what you have to pay out of pocket.
Financial Assistance Options
For those facing money problems, there are ways to get help. These include:
- Patient Advocacy Groups: Groups that help and guide through the healthcare system.
- Financial Aid Programs: Some hospitals and non-profits offer financial help to those who qualify.
- Government Programs: Medicaid and other government programs might cover costs for some.
Knowing about costs, insurance, and financial help can help patients deal with the financial side of pituitary surgery.
Patient Experiences and Quality of Life
Understanding the personal impact of pituitary tumors is key for patients and their families. Living with a pituitary tumor is more than just medical treatment. It needs a holistic approach to health. We know that patient experiences with pituitary tumors vary a lot. It’s important to focus on the quality of life after surgery.
Patients who have surgery often share their recovery experiences. Recovery testimonials give us insights into what patients can expect. They show how people cope with the challenges they face.
Recovery Testimonials
Many patients have shared their recovery stories. They talk about the physical and emotional challenges they faced. For example, one patient said, “The first few weeks after surgery were tough. But with my family’s and the medical team’s support, I got stronger.”
“The care I received was exceptional. The neurosurgeon’s team was very supportive, and the nurses were always available to answer my questions.”
These stories show how important comprehensive care and support are during recovery.
Long-term Outcomes
The long-term outcomes for patients after surgery are mostly positive. Many see big improvements in their symptoms and quality of life. But, some may need ongoing medical care, like hormone replacement therapy.
| Outcome | Percentage of Patients |
| Improved Symptoms | 80% |
| Hormone Replacement Therapy | 40% |
| Return to Normal Activities | 90% |
This table shows the typical long-term outcomes for patients after surgery. It highlights the different experiences patients can have.
Support Groups and Resources
Support groups are crucial in recovery. They offer a community and resources to manage the condition. Organizations like the American Brain Tumor Association provide valuable support and information.
Support groups connect patients with others who have similar experiences. They help with the emotional and practical sides of living with a pituitary tumor.
Choosing the Right Neurosurgeon and Medical Center
Finding the right neurosurgeon and medical center is key for treating pituitary tumors. This choice greatly affects your surgery’s success and your care experience.
Qualifications to Look For
When looking for a neurosurgeon, check their qualifications and experience with pituitary tumors. A board-certified surgeon with a strong track record in neurosurgery is a good start. Specialization in endoscopic or microscopic surgery is also beneficial.
Also, consider the neurosurgeon’s connection to a reputable medical center. A surgeon working in a well-equipped hospital with a team can offer better care.
Questions to Ask Your Surgeon
Before deciding, make a list of questions for your neurosurgeon. Ask about their experience with pituitary tumor surgeries and their approach to your case. Also, inquire about their complication rates and emergency handling.
- What is your experience with pituitary tumor surgeries?
- What surgical approach do you recommend for my case?
- How do you manage potential complications?
The Importance of Specialized Centers
Choosing a specialized center for your treatment has many benefits. These centers have teams of experts, including neurosurgeons and endocrinologists, for comprehensive care.Specialized centers also offer access to the latest treatments and technologies through research and clinical trials. This is crucial for complex or rare cases.
Conclusion
We’ve looked into the details of pituitary tumors and the surgery options, like craniotomy. It’s key for patients to understand the diagnosis, treatment choices, and surgical methods.
Pituitary tumor craniotomy is a big surgery that needs careful thought and skill. We’ve highlighted the main points to show how important a full treatment plan is. This includes everything from diagnosis to after-care.
In wrapping up, dealing with pituitary tumors is more than just surgery. It involves planning, using the latest technology, and ongoing care. We urge patients to team up with their doctors to make these tough choices.
FAQ
What is a pituitary tumor craniotomy?
A pituitary tumor craniotomy is a surgery. A neurosurgeon removes part of the skull. This lets them remove a tumor on the pituitary gland.
When is a craniotomy recommended for pituitary tumor treatment?
A craniotomy is often needed for big or complex tumors. It’s also used when the tumor can’t be safely removed through another method. Or when direct access is needed.
What are the risks associated with pituitary craniotomy?
Risks include problems with the brain and hormones. There’s also a chance of infection, fluid leakage, and general surgery risks like bleeding.
How long does it take to recover from a pituitary tumor craniotomy?
Recove
ry time varies. Most patients stay in the hospital for a few days to a week. They may need weeks to months to fully recover.
What is the role of post-operative care after pituitary tumor surgery?
Post-operative care is key. It involves managing pain, watching for complications, and adjusting hormone therapy. Follow-up imaging is also done to check for tumor return.
How much does pituitary surgery typically cost in the United States?
Costs vary widely. They depend on the procedure’s complexity, hospital charges, and surgeon’s fees. Costs can range from tens of thousands to over a hundred thousand dollars.
Does insurance typically cover pituitary tumor surgery?
Most insurance plans cover pituitary tumor surgery. But, coverage can vary. It’s important to check with your insurance provider.
What are the long-term outcomes after pituitary tumor surgery?
Outcomes depend on the tumor type and size. They also depend on surgery success and the need for ongoing treatments.
How do I choose the right neurosurgeon for my pituitary tumor treatment?
Look for a neurosurgeon with experience in pituitary tumor surgery. Check their qualifications and ask about their approach and success rates. Understand what to expect during and after surgery.
What technological advances have improved pituitary tumor surgery?
Advances like neuronavigation systems and intraoperative MRI have improved surgery. Endoscopic assistance has also made it safer and more precise.
Are there support groups for patients after pituitary surgery?
Yes, there are support groups and resources for patients. They provide a community for sharing experiences and getting support.
What are the signs and symptoms of pituitary tumors that I should be aware of?
Symptoms include hormonal imbalances and pressure-related issues. These can be headaches, vision problems, or neurological deficits. They depend on the tumor’s size and location.
References
JAMA Network. Evidence-Based Medical Insight. Retrieved from https://jamanetwork.com/journals/jama/fullarticle/2596980





