Last Updated on December 3, 2025 by Bilal Hasdemir
More than 100,000 people worldwide are waiting for a heart transplant. But, there aren’t enough donor hearts to meet the demand. This has led to big steps in making robotic hearts or artificial hearts. These are made to help or replace the natural heart.Curious about a plastic heart? Discover the lifespan and technology of modern robotic hearts. Get positive, insightful answers here today!
We’re seeing a big change in treating heart failure with mechanical heart replacements. These include the plasticheart. They are made to last a long time and help those who need a heart transplant.
The life span of a robotic heart is key to its success. In this article, we’ll look at the latest in artificial hearts. We’ll also talk about what patients and doctors can expect for how long these devices will last.
Key Takeaways
- The demand for heart transplants far exceeds the availability of donor hearts.
- Robotic hearts are being developed to support or replace natural hearts.
- The longevity of a robotic heart is critical for its success.
- Advancements in technology are improving the durability of artificial hearts.
- Mechanical heart replacements offer a promising solution for heart failure patients.
The PlasticHeart: Revolutionary Materials in Cardiac Technology
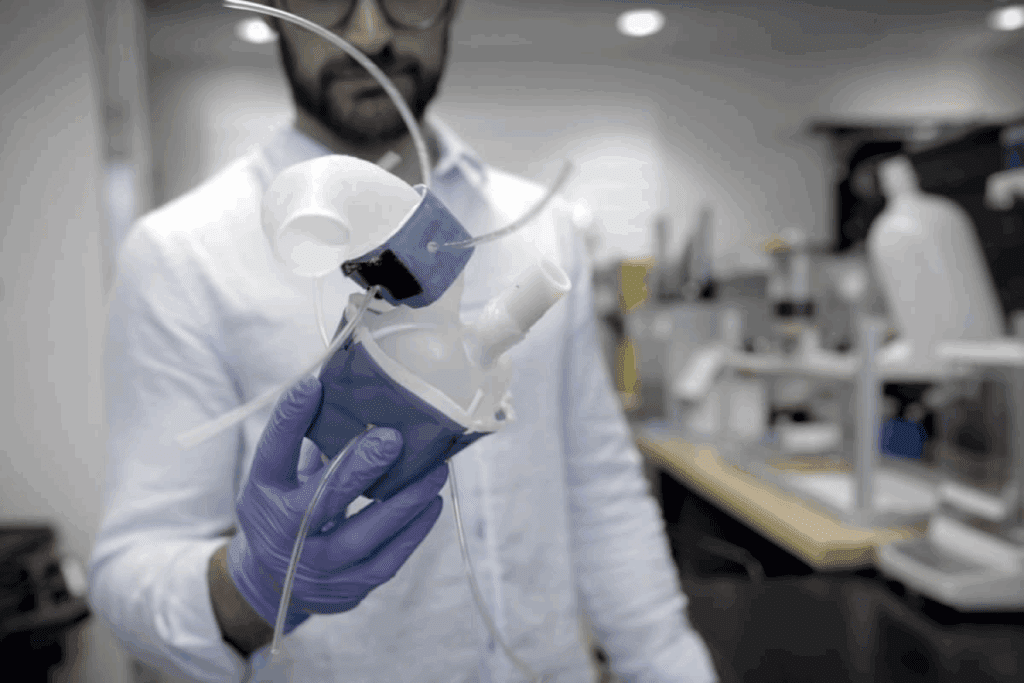
Advances in biocompatible polymers have led to stronger and more efficient artificial hearts. This is a big step forward in heart technology. The PlasticHeart is a major change in how heart devices are made and work.
Modern artificial hearts use biocompatible polymers. These materials are made to work well with the body. This reduces the chance of bad reactions and makes the device work better.
Biocompatible Polymers in Modern Designs
Biocompatible polymers are key in making artificial hearts. They bring many benefits, such as:
- They last longer and are less likely to wear out
- They are safe for the body, lowering the risk of problems
- They allow for more complex designs that work better
Thanks to these materials, we can make artificial hearts that work more like real hearts.
Advantages of Plastic Components in Artificial Hearts
Plastic parts in artificial hearts have big advantages. They can be made very precisely, leading to better designs.
Some main benefits are:
- They are lighter, making them more comfortable for patients
- They are cheaper to make, which could make artificial hearts more available
- They resist corrosion and wear better over time
A top cardiologist, says, “Using biocompatible polymers in artificial hearts is a big deal. It opens up new options for patients who need these devices.”
By using these new materials and tech, we can keep making artificial hearts better. This means better outcomes and a better life for patients.
Average Lifespan of Current Robotic Heart Models
The lifespan of robotic heart models is key in cardiac tech. As these devices grow in use, knowing how long they last is vital. This info helps both patients and healthcare teams.
Expected Operational Timeframes by Device Type
Robotic heart models vary by type, affecting their lifespan. Continuous-flow devices are built to last, working well for years. On the other hand, pulsatile-flow devices might not last as long due to their design.
The design and how these devices work greatly affect their lifespan. Companies are improving their devices with better materials and engineering.
Comparing Longevity Between Manufacturers
When looking at how long robotic heart models last, many things matter. This includes the materials, design, and how well they’re made. For example, some makers use stronger materials or design their devices to last longer.
Top companies like Syncardia and Berlin Heart have made big strides. They offer devices that last a long time. By looking at these devices’ specs and performance, healthcare teams can choose the best for their patients.
Factors That Influence Artificial Heart Durability
It’s important to know what affects how long artificial hearts last. These devices face many challenges that can impact their lifespan.
Material Properties and Degradation Patterns
The materials used in artificial hearts are key to their durability. Biocompatible polymers and metals are chosen for their strength and safety in the body. But, they can wear down over time due to corrosion, wear, and body fluids.
How fast materials break down depends on the material and the body’s conditions. Some materials might break down faster when exposed to certain enzymes or stress. Knowing this helps make artificial hearts last longer.
Mechanical Stress and Component Fatigue
Artificial hearts work hard, pumping blood all the time. This constant effort can cause parts to wear out, leading to mechanical failure. This is a big worry because it can make the device stop working and need to be replaced.
The design and materials of artificial hearts help fight off mechanical stress and wear. New designs and materials are making these devices more reliable.
Power Systems and Battery Limitations
The power systems of artificial hearts, like batteries and external power, are vital. The battery life and how well the power system works are big factors in how long the device lasts.
| Power System Component | Typical Lifespan | Factors Affecting Durability |
| Batteries | 8-12 hours | Charge cycles, depth of discharge |
| External Power Sources | Varies | Usage patterns, maintenance |
| Internal Drives | Several years | Mechanical stress, material quality |
Knowing the limits of power systems is key to managing patient hopes and improving device design. Better batteries and power management are essential for making artificial hearts more durable and useful.
Maintenance Requirements for Extending Device Lifespan
To keep artificial heart devices working well, regular maintenance is key. Proper care extends the device’s life and keeps it running smoothly. This improves the patient’s life quality.
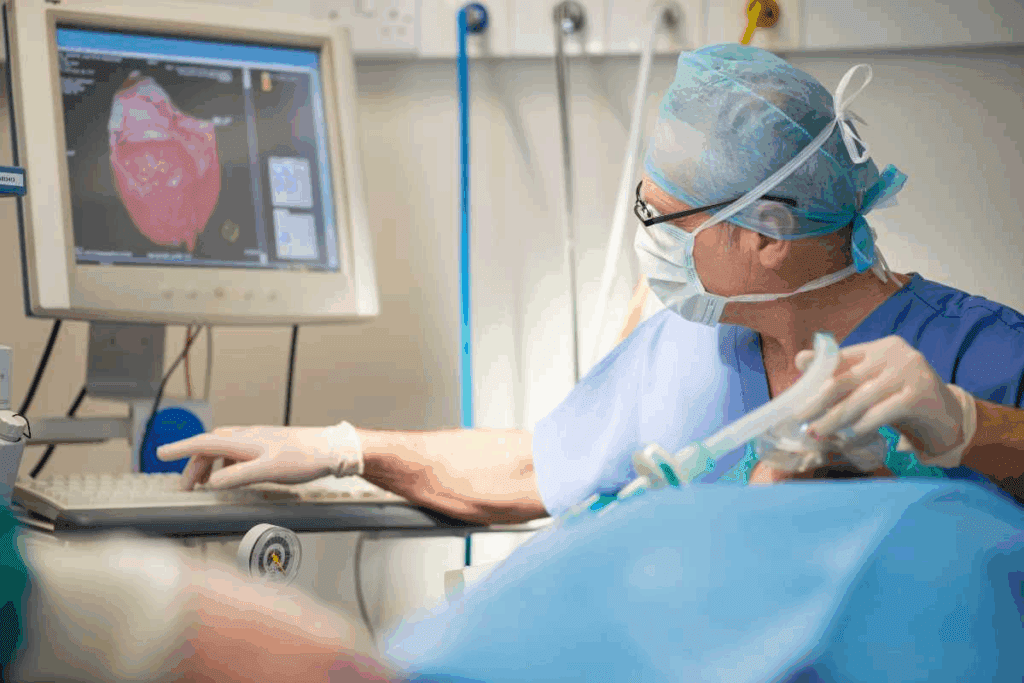
Regular Monitoring Protocols
Checking the device regularly is vital. This includes daily checks on power, mechanical function, and any alarms. Patients or caregivers should watch the device closely and tell their doctor about any issues.
The monitoring protocols include:
- Daily checks on device power levels and battery status
- Regular assessment of the device’s mechanical components
- Monitoring for any alarm signals or warning messages
Component Replacement Schedules
Replacing parts is a big part of keeping artificial hearts working. Some parts, like batteries or wearable parts, need to be swapped out. Patients should follow the maker’s schedule to avoid problems.
| Component | Replacement Interval | Responsibility |
| Batteries | Every 6-12 months | Patient/Caregiver |
| Wearable Parts | Every 3-6 months | Patient/Caregiver |
| Internal Components | As recommended by manufacturer | Healthcare Provider |
External Equipment Maintenance
External gear, like controllers and power units, also need care. Keep them clean, store them right, and update software as needed.
Best practices for external equipment maintenance include:
- Regularly cleaning the equipment to prevent dust buildup
- Storing the equipment in a dry, cool place
- Updating software and firmware as recommended by the manufacturer
By sticking to these maintenance steps, patients with artificial hearts can keep them running well. This improves their life quality.
Real Patient Experiences with Artificial Hearts
Patients with artificial hearts have stories that are both diverse and inspiring. These stories give us a glimpse into the challenges and triumphs of life with these devices. They help us understand the realities of living with an artificial heart.
Longest-Living Recipients and Their Stories
Some patients have had artificial hearts for over five years. Their stories show how far cardiac technology has come. They are living proof of the advancements in heart care.
These long-term survivors often stick to their treatment plans and have strong support systems. Their experiences stress the need for thorough care to extend the life of artificial hearts.
Quality of Life Reports from Long-Term Users
Users of artificial hearts often see a big boost in their quality of life. They can do things they love, but with some adjustments. This shows how artificial hearts can improve life, not just extend it.
For example, some patients can travel, exercise lightly, and even work again. Their stories highlight the artificial heart’s ability to enhance life’s quality.
We know each patient’s journey is different. It depends on their health, the type of device, and their personal strength. By sharing these stories, we aim to give a detailed look at life with an artificial heart.
Complications That Can Shorten Device Lifespan
It’s important to know about the problems that can happen with artificial heart devices. These devices help or replace the heart’s work. But, many things can affect how long they last and how well they work.
Infection Risks and Prevention
Infections are a big worry for people with artificial heart devices. We can lower the risk of infection by using careful surgery, good care after surgery, and special coatings on the device. It’s key to watch closely and see the doctor often to catch any infections early.
Prevention strategies include giving antibiotics before and after surgery. Also, teaching patients about infection signs that need quick doctor visits. These steps help keep the device working longer.
Thrombosis and Embolism Concerns
Thrombosis and embolism are serious problems with artificial heart devices. Blood clots can cause the device to fail or lead to dangerous blockages. We use blood thinners and check the blood often to lower this risk.
The design of the device also helps. Advances in material science have made surfaces that are less likely to cause clots.
Mechanical Failures and Their Causes
Mechanical failures are another issue. They can happen because of wear and tear, mistakes in making the device, or not taking good care of it. We make sure to check and maintain the device regularly to avoid these problems.
Causes of mechanical failure include wear and tear, misuse, or power issues. Knowing these causes helps doctors take steps to keep the device working well for a long time.
Living Daily Life with a Mechanical Heart
A mechanical heart can save lives, but it needs careful care. Understanding how it affects our health and its lifespan is key. This knowledge helps us live better with these devices.
Physical Activity Guidelines and Limitations
Staying active is good for health, but with a mechanical heart, there are rules. Patients should do moderate exercise, like walking fast or swimming. But, they should avoid hard activities or sports that could harm the device.
It’s vital to listen to your body during exercise. Watch for signs of tiredness or pain. Talking to doctors can help create a workout plan that’s right for you.
Powering Considerations and Backup Systems
Keeping a mechanical heart powered is a big part of daily life. Most need an outside power source. So, patients must keep an eye on battery life and have a backup plan.
Carrying extra batteries and knowing how to swap them out helps avoid long breaks. Also, knowing how to fix common power issues can help patients deal with small problems. Regular checks by doctors are also important to keep everything working right.
Psychological Adaptation to Device Dependency
The mental side of having a mechanical heart is important. Patients may feel many emotions, from relief to worry about needing the device. Support groups and counseling can help a lot. They offer a place to share and learn how to cope.
Also, teaching family and friends about the device helps. It makes patients feel supported and less alone in their journey.
Comparing Artificial Hearts to Biological Transplants
When looking at heart replacement options, patients and doctors must consider the pros and cons of artificial hearts versus biological transplants. This is key to finding the best treatment for those with severe heart failure.
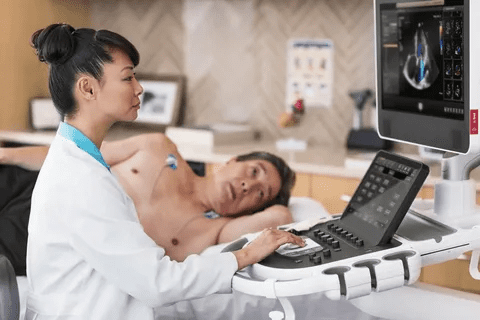
Survival Statistics and Outcomes
Survival rates for artificial heart patients have jumped up in the last ten years. Studies show a one-year survival rate of about 80% for artificial heart patients. Some devices even have higher success rates.
Heart transplant patients have a one-year survival rate of about 90%. But, both artificial hearts and transplants have their long-term benefits. Some artificial heart patients live more than five years.
“The advancements in artificial heart technology have been remarkable, giving patients a good alternative when a transplant is not possible,” says a leading cardiologist. “But, the choice between an artificial heart and a transplant depends on many factors specific to the patient.”
Advantages and Disadvantages of Each Approach
Artificial hearts have big advantages. They are immediately available and can support patients until a transplant is found. They also offer a mechanically durable solution, lowering the risk of transplant complications like rejection.
Biological transplants, on the other hand, offer a more natural heart function. They might also avoid the need for long-term blood thinners needed with artificial hearts. But, they are limited by the availability of donor hearts and carry risks of rejection and other complications.
In conclusion, both artificial hearts and biological transplants have their roles in treating heart failure. The choice depends on the patient’s needs, medical history, and personal preferences. As technology advances, we can expect better outcomes for patients.
Technological Innovations Extending Robotic Heart Longevity
We’re seeing big steps forward in robotic heart tech. New materials, power solutions, and monitoring systems are making artificial hearts last longer and work better.
Next-Generation Materials and Coatings
Biocompatible polymers and advanced coatings are key to longer-lasting robotic hearts. They help avoid problems like blood clots and infections. They also make the device more durable.
For example, nanotechnology coatings can cut down on friction and wear. This means the artificial heart can work longer without breaking down.
Advanced Power Solutions and Wireless Charging
Powering robotic hearts is a big challenge. Old battery systems don’t last long or work well. But, advanced power solutions like wireless charging are changing that.
Wireless charging keeps the device running without cables. This cuts down on infection risks and makes patients more comfortable. It’s a big win for robotic heart longevity.
Self-Monitoring and Adaptive Systems
Self-monitoring and adaptive systems are also big deals in robotic heart tech. They watch how the device is doing and adjust as needed.
With smart sensors and AI, these systems can spot problems before they happen. They can then change how the device works to keep it running smoothly. This makes the robotic heart more reliable and longer-lasting.
The Economics of Artificial Heart Technology
Artificial heart technology is a big investment for patients. There are many costs and ways to get financial help. It’s important to know how this technology affects both patients and healthcare providers financially.
Device and Procedure Costs
The cost of artificial heart devices is high, ranging from $100,000 to over $200,000. For example, the SynCardia total artificial heart is used for patients waiting for a heart transplant. The surgery to put in these devices is also expensive, needing skilled surgeons and long hospital stays.
Some of the main costs are:
- Device Cost: The price of the artificial heart device itself.
- Surgical Procedure: Costs for the surgery, including surgeon fees, anesthesia, and hospital stay.
- Follow-up Care: Ongoing costs for monitoring, maintenance, and possible device replacement.
A study in a Journal found the first year’s costs can be over $250,000. This shows the need for good financial planning and support for patients.
Insurance Coverage and Financial Support Options
Getting insurance for artificial heart technology can be tough. Many insurance plans cover a lot of the costs, but how much varies. Medicare and Medicaid in the U.S. often cover approved devices, but the coverage can be different.
For those struggling financially, there are help options:
- Manufacturer Assistance Programs: Some makers offer financial help or grants to eligible patients.
- Non-profit Organizations: Groups like the American Heart Association provide resources and sometimes financial aid to patients in need.
- Government Programs: Other government programs may also offer financial support to eligible people.
It’s key for patients and their families to look into these options. This way, they can manage the cost of artificial heart technology better. Knowing about financial support and insurance can help patients deal with the complex financial side of these devices.
As artificial heart technology gets better, we must also focus on making it more affordable. This is important so these life-saving devices are available to those who need them most.
Future Directions in Synthetic Heart Development
Synthetic heart technology is on the verge of a new era. This is thanks to advances in bioengineered tissues and fully implantable systems. We’re moving towards more advanced and personalized treatments for heart conditions.
Bioengineered Tissues and Hybrid Solutions
Research in bioengineered tissues is very promising. It combines synthetic materials with living cells. This creates hybrid solutions that are both strong and biological.
These hybrid solutions could make synthetic hearts work better with the body. They might also lower the chance of problems and improve results.
The use of hybrid solutions also means we can tailor treatments to each patient. This could lead to more effective and lasting treatments.
Fully Implantable Systems Without External Components
Another focus is on fully implantable systems without external parts. This means better power systems and wireless charging. It lets devices charge without cables or batteries.
These systems have many benefits. They reduce infection risk and improve how patients can move around. They make life better for those with synthetic hearts, allowing them to be more active.
As we look ahead, combining these technologies is key. With more research and innovation, we’re hopeful about better patient outcomes. We’re excited to see how these advancements will change cardiac therapy.
Conclusion: Balancing Technology, Longevity, and Quality of Life
The lifespan of a robotic heart depends on many things. These include new technology, how well materials last, and how well patients are cared for. New artificial hearts are showing great promise in making patients’ lives better.
New materials, power systems, and ways to monitor health are making these devices last longer. This means patients get better care. At our institution, we aim to give top-notch healthcare to patients from around the world.
We want to keep improving the lives of those with artificial hearts. Our goal is to offer the latest medical solutions. We focus on making sure our patients get the best care and support, improving their overall well-being.
FAQ
What is the average lifespan of a robotic heart?
The lifespan of a robotic heart depends on its model and maker. Most are made to last several years. Some can even last up to 5 years or more with good care.
What materials are used in constructing artificial hearts?
Artificial hearts are made from materials like polyurethane and titanium. These are chosen for their strength and to avoid harmful reactions.
How long can a person live with an artificial heart?
How long someone can live with an artificial heart varies. It depends on the heart’s quality, how well it’s maintained, and the person’s health. But, some people have lived for years with these devices.
What are the risks associated with artificial hearts?
Artificial hearts can face issues like infections, blood clots, and mechanical problems. But, these risks can be lowered with proper care and checks.
How do I maintain my artificial heart?
Keeping an artificial heart in good shape means regular checks, replacing parts when needed, and looking after the external equipment. This helps it last longer.
Can I lead a normal life with a mechanical heart?
Living with a mechanical heart does require some changes. But, many people can lead active lives with the right care and management.
How does an artificial heart compare to a biological transplant?
Artificial hearts and biological transplants have their own pros and cons. The choice between them depends on what each patient needs and their situation.
What are the latest advancements in artificial heart technology?
New advancements include better materials, power sources, and systems that can check themselves. These improvements are making artificial hearts more durable and effective.
How much does an artificial heart cost?
The price of an artificial heart changes based on the type and maker. There are also options for insurance and financial help to make these devices more accessible.
What is the future of synthetic heart development?
The future of synthetic hearts looks promising. New technologies like bioengineered tissues and fully implantable systems are on the horizon. They aim to change heart replacement therapy for the better.
Reference
- Timms, D. (2011). A review of clinical ventricular assist devices. Medical Engineering & Physics, 33(9), 1041–1047. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3156927/





