Last Updated on December 2, 2025 by Bilal Hasdemir
Did you know thousands of kids worldwide get life-saving platelet transfusions every year? The World Health Organization (WHO) sets important guidelines. These ensure transfusions are safe and work well. A guide to calculating and adjusting the infusion rate of platelets, according to standard Platelet transfusion rate guidelines.
Pediatric blood transfusion guidelines are key in treating many illnesses. This includes cancer, trauma, and bleeding disorders. Getting the transfusion rate right is key. It helps avoid bad reactions and makes sure treatment works.
Healthcare workers need to know the latest guidelines to care for patients well. In this article, we’ll look at the WHO’s pediatric transfusion guidelines. We’ll see why they’re important in caring for kids.
Key Takeaways
- The WHO provides guidelines for safe and effective platelet transfusions in children.
- Understanding pediatric blood transfusion guidelines is vital for healthcare professionals.
- The correct transfusion rate is vital to prevent adverse reactions and ensure treatment efficacy.
- Pediatric transfusion guidelines play a critical role in treating various medical conditions.
- Staying updated with the latest guidelines is essential for providing quality patient care.
Overview of Platelet Transfusion in Pediatrics

In pediatric medicine, platelet transfusions are key for managing low platelet counts or dysfunction. It’s vital to grasp the details of platelet transfusions for the best care of our young patients.
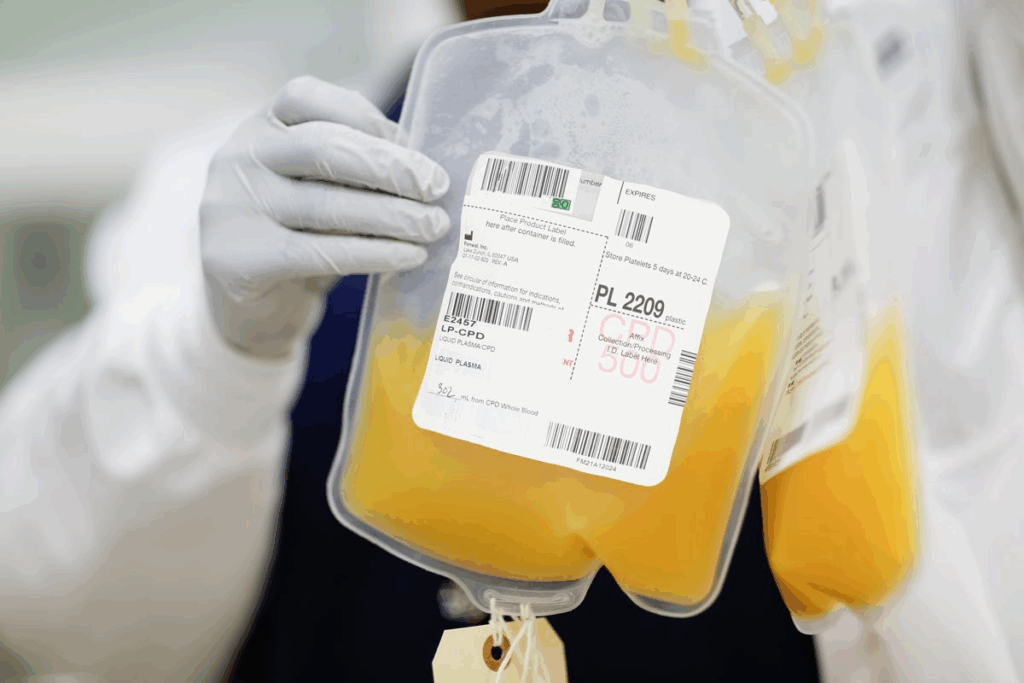
What Is Platelet Transfusion?
A platelet transfusion adds platelets to a patient’s blood to stop or treat bleeding. It’s essential for kids with low platelet counts or bleeding risks from medical conditions or treatments.
“Platelet transfusions are vital for managing bleeding disorders in pediatric patients or those undergoing treatments that affect platelet counts.”
Why Are Platelet Transfusions Necessary?
Platelet transfusions are needed for several reasons. Kids with immune thrombocytopenic purpura (ITP) or undergoing chemotherapy face bleeding risks. Transfusions boost platelet counts, preventing or controlling bleeding.
They’re also critical for kids having surgeries or invasive procedures that could cause bleeding. Ensuring enough platelets reduces the risk of bleeding during these times.
Common Conditions Requiring Platelet Transfusion
Several conditions may require platelet transfusions in kids. These include:
- Immune Thrombocytopenic Purpura (ITP): An autoimmune condition causing low platelet counts.
- Cancer and Chemotherapy: Cancer treatments can lower platelet counts by affecting bone marrow.
- Aplastic Anemia: A condition where the bone marrow doesn’t make enough blood cells, including platelets.
- Major Surgery or Trauma: Significant blood loss or dilutional thrombocytopenia may require transfusions.
Knowing these conditions and the role of platelet transfusions is key for caring for pediatric patients. Following pediatric transfusion guidelines helps ensure the best outcomes for young patients.
The Role of WHO Guidelines in Blood Transfusion
The WHO guidelines are key for healthcare providers around the world. They help ensure safe blood transfusions. This is very important in pediatric care, where mistakes can be deadly.
Understanding the WHO Guidelines
The WHO guidelines cover all important aspects of blood transfusions. They talk about choosing donors, screening blood, and how to transfuse it. They stress the need for proper blood typing and cross-matching to avoid bad reactions. This is very important for kids, where matching blood types is critical.
These guidelines are not just suggestions. They are the rules that make blood transfusions safe and effective everywhere. By following them, doctors can lower the risks of problems during transfusions.
Importance of Global Standards in Pediatric Care
Global standards are essential for kids’ health care. The WHO guidelines help make sure kids get the best care no matter where they are. They set a universal standard for blood transfusions.
- Standardization of Care: Makes sure all kids get the same high-quality care, based on the latest research and best practices.
- Safety: Highlights the need for safe transfusions, lowering the chance of bad reactions.
- Training and Education: Offers a foundation for training doctors, making sure they can give blood transfusions safely and well.
By sticking to the WHO guidelines, we can make sure kids get transfusions that save their lives. This shows our dedication to top-notch healthcare for all.
Recommended Platelet Transfusion Rates
In pediatric care, the right amount of platelet transfusions changes based on the patient’s health and the hospital’s rules. Finding the best amount to transfuse is complex. It depends on many clinical factors.
How Are Rates Determined?
Doctors figure out how many platelets to give by looking at several things. They check why the patient has low platelets, how sick they are, and if they’re bleeding. This helps them find a balance between helping the patient and avoiding risks.
They look at how bad the low platelets are and the patient’s overall health. For example, a child with very low platelets and bleeding might need more transfusions than one with only a little low and no bleeding.
Variability in Transfusion Practices
Even with guidelines, how often platelets are given can vary a lot. This difference comes from how doctors interpret data, hospital rules, and what resources are available.
This variation can affect how well patients do. So, there’s a push to make transfusions more consistent and based on solid evidence. By understanding why this variation happens, we can work towards better, more consistent care.
Factors Influencing Transfusion Rates
Many things affect how often platelets are given. These include how bad the low platelets are, if the patient is bleeding, and their overall health. Also, why the patient has low platelets matters a lot.
By thinking about these factors, we can make transfusions fit each patient’s needs. This way, we can make sure platelet transfusions help a lot while keeping risks low.
Indications for Platelet Transfusions in Children
We look at when platelet transfusions are needed in kids. These transfusions are key for managing many pediatric conditions. They are most important when kids have severe low platelet counts or are bleeding a lot.
Clinical Scenarios Requiring Transfusion
Platelet transfusions are needed in several situations. For example, kids who are bleeding a lot or are about to have surgery. They help prevent bleeding.
Children on chemotherapy or getting a bone marrow transplant also need them. This is because they risk having very low platelet counts.
Other kids might have severe thrombocytopenia or platelet problems. Transfusions help stop or manage bleeding in these cases.
Acute vs. Chronic Conditions
It’s important to know if a condition is acute or chronic. Acute conditions, like trauma or leukemia, might need immediate transfusions. This is to stop severe bleeding or prevent more problems.
Chronic conditions, like aplastic anemia or myelodysplastic syndromes, might need transfusions more often. Knowing the condition helps doctors tailor care to each child’s needs.
| Condition | Transfusion Indication | Frequency of Transfusion |
| Acute Leukemia | Severe thrombocytopenia or bleeding | As needed based on platelet count and clinical condition |
| Aplastic Anemia | Severe thrombocytopenia | Regularly, based on platelet count |
| Trauma | Significant bleeding | Immediately, as needed |
Understanding when to give platelet transfusions helps us care for kids better. This matches pediatric blood transfusion guidelines. It ensures our patients get the best treatment.
Risks and Complications of Platelet Transfusions
It’s important to know the risks and complications of platelet transfusions. These transfusions save lives but can have side effects. We must watch for these to help our pediatric patients.
Common Side Effects
Side effects of platelet transfusions can be mild or moderate. These include:
- Fever, which can be a sign of an immune response to the transfused platelets.
- Chills, often accompanying fever, these can be uncomfortable for the patient.
- Allergic reactions, which can manifest as rash, itching, or more severe reactions like anaphylaxis.
While these reactions can be concerning, they are usually manageable. Prompt recognition and treatment of these side effects are critical to preventing more severe outcomes.
Serious Adverse Reactions
There are also serious adverse reactions that can happen. These include:
- Anaphylaxis, a severe, life-threatening allergic reaction that requires immediate intervention.
- Transfusion-related acute lung injury (TRALI), a potentially life-threatening complication characterized by non-cardiogenic pulmonary edema.
- Graft-versus-host disease (GVHD), a rare but serious complication where the transfused immune cells attack the recipient’s tissues.
These serious reactions highlight the need for careful monitoring and a well-equipped transfusion service.
Monitoring Post-Transfusion
Monitoring patients after a platelet transfusion is key. This involves:
- Regularly checking vital signs to quickly identify any deviations from normal.
- Assessing for signs of adverse reactions, such as fever, chills, or rash.
- Evaluating the effectiveness of the transfusion through platelet count monitoring.
As emphasized by a leading medical source,
“The key to managing complications lies in early detection and appropriate response.”
By being proactive and vigilant, we can minimize risks and ensure our patients get the best care.
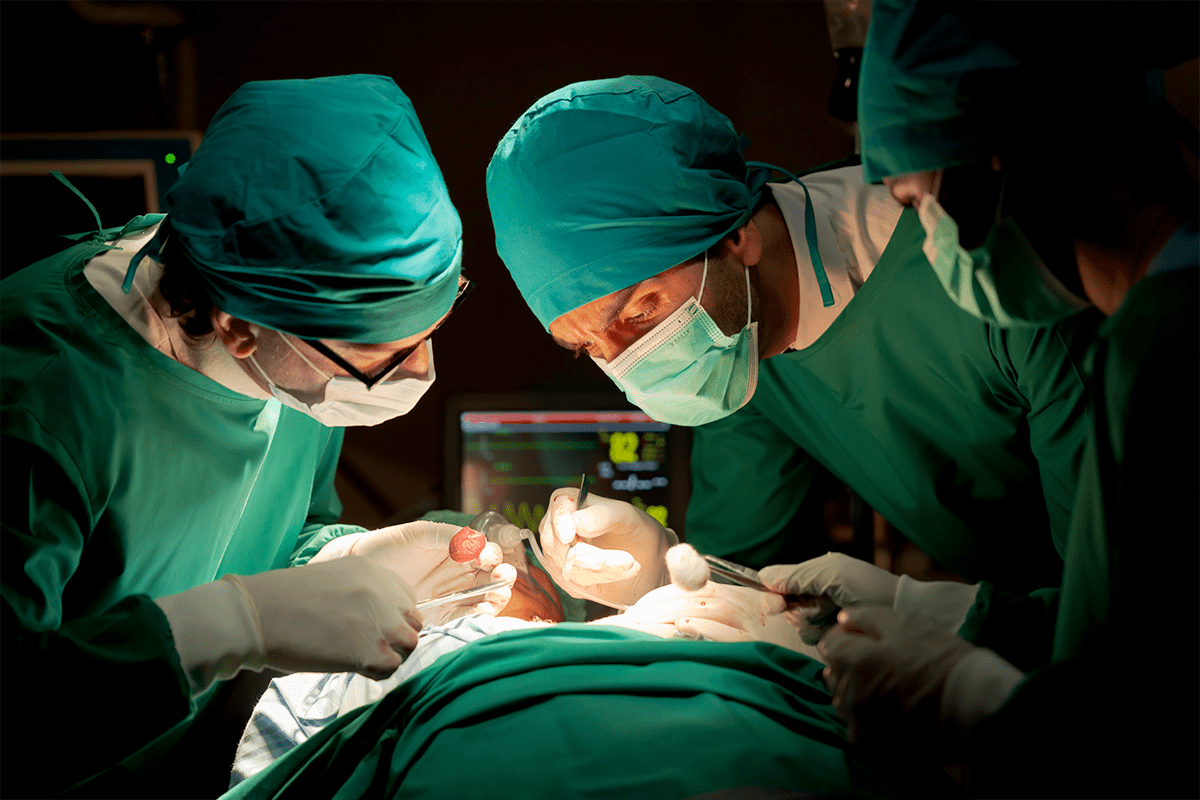
Best Practices for Administering Platelet Transfusions
Administering platelet transfusions to children needs a detailed plan. This includes careful preparation and safe ways to give the transfusions. We know it can seem tough, but with the right help, it can be done well.
Preparation of the Child for Transfusion
Getting the child ready for a platelet transfusion is key. This means explaining the process to the child and their family. We also check the child’s medical history and current health to spot any risks.
Key steps in preparing the child include:
- Providing clear explanations and reassurance to the child and their family
- Verifying the child’s identity and ensuring that the correct blood component is used
- Assessing the child’s medical history and current condition
- Obtaining informed consent from the parents or guardians
Techniques for Safe Administration
Safe ways to give the transfusion are very important. We follow strict rules to check the blood, use filters, and watch the patient closely during and after.
Safe administration techniques include:
| Technique | Description | Benefits |
| Verifying the Blood Component | Checking the blood component for compatibility and integrity | Prevents adverse reactions due to incompatibility |
| Using Appropriate Filters | Utilizing filters to remove any contaminants or debris | Ensures the purity of the transfused blood component |
| Monitoring the Patient | Closely observing the patient during and after the transfusion | Allows for prompt intervention in case of any adverse reactions |
By sticking to these best practices, we can lower the risks of platelet transfusions. This helps us get the best results for our young patients.
Assessing Patient Response to Platelet Transfusions
After a platelet transfusion, we watch the patient closely. We check how well the treatment works. This includes both clinical checks and lab tests to spot any issues early.
Monitoring Platelet Counts
Checking platelet counts before and after transfusion is key. If the count goes up after transfusion, it means it worked. We check the count once an hour after and again 24 hours later to see how long it lasts.
The table below shows what we expect to see in platelet counts after a transfusion:
| Time | Expected Platelet Count Change |
| Pre-transfusion | Low |
| 1 hour post-transfusion | Significant increase |
| 24 hours post-transfusion | Variable, depending on underlying condition |
Signs of Improvement or Complications
We also look for signs of better health or problems. If the patient stops bleeding and wounds heal, it’s a good sign. But, if they have adverse reactions like fever or rash, or if the platelet count doesn’t go up enough, it’s a problem.
Here are some key signs we look for:
- Signs of improvement: Less bleeding, wounds healing, stable health.
- Signs of complications: Fever, chills, rash, platelet count not rising enough.
By watching how the patient reacts to the transfusion, we can give them the best care. We follow pediatric blood transfusion guidelines to make sure they get the best results.
Ethical Considerations in Blood Transfusion
In pediatric blood transfusion, ethics are key to patient safety and well-being. We must carefully balance medical needs with ethical standards.
Informed Consent for Pediatric Patients
Getting informed consent is vital, as kids can’t give it themselves. We count on parents or guardians to make decisions for them.
To help with informed consent, we should:
- Clearly explain why the transfusion is needed and its risks and benefits.
- Tell them about other treatment options, if any.
- Make sure the family understands the procedure and can ask questions.
This approach respects family autonomy and builds trust with the healthcare team.
Cultural Sensitivity in Transfusion Practices
Cultural beliefs and practices shape how families view blood transfusions. We must be culturally sensitive to our diverse patients.
Important considerations include:
- Understanding and respecting cultural views on blood.
- Knowing about any cultural or religious blood transfusion objections and discussing alternatives.
- Talking with families in a way that respects their culture and addresses their concerns.
By being culturally sensitive, we offer care that respects the patient’s and family’s cultural background.
Ethical issues in blood transfusion are complex. We are dedicated to upholding the highest ethical standards. This ensures our patients get the best care possible.
Future Directions in Platelet Transfusion Research
Future Directions in Platelet Transfusion Research
Platelet transfusion is on the verge of a revolution thanks to ongoing research. The field of transfusion medicine is always changing. It’s driven by the need to make blood transfusions safer and more effective for kids.
We’re seeing big steps forward in many areas. This includes better ways to store platelets, improved matching techniques, and new products. These changes are key for better patient results and lowering the risks of platelet transfusions.
Era Page Innovations in Transfusion Medicine
The era of innovation in transfusion medicine is filled with important developments. One big step is in how we store platelets. Old methods can lead to bacterial contamination and have a short shelf life. New solutions and technologies are being looked into to fix these problems.
Another area seeing big changes is in matching platelets. New genotyping techniques are being developed. They aim to make sure donors and recipients are a better match, reducing the chance of bad reactions.
Ongoing Studies and Trials
Many studies and clinical trials are looking into new ways to do platelet transfusions. They’re exploring the use of pathogen-reduced platelet components. This is to lower the risk of infections from transfusions.
They’re also studying different ways to give platelets and how they affect patients in different situations. This research could lead to better outcomes for patients.
Page table>
| Area of Research | Description | Potential Impact |
| Improved Storage Methods | New technologies to enhance platelet storage, reducing bacterial contamination risk and prolonging shelf life. | Reduced risk of transfusion-transmitted infections and improved platelet availability. |
| Advanced Typing and Matching | Genotyping techniques to improve donor and recipient compatibility. | Minimized risk of adverse reactions and improved transfusion outcomes. |
| Pathogen-Reduced Platelet Components | Technologies to reduce pathogens in platelet components. | Enhanced safety of platelet transfusions by reducing infection risks. |
Conclusion: Importance of Adhering to Guidelines
Following Page guidelines for platelet transfusions is key for safety and success in kids. It helps us give the best care and improve patient results.
It’s important to keep the right platelet transfusion rate and stick to pediatric blood transfusion guidelines. These rules help doctors make smart choices for pediatric transfusion guidelines.
Optimizing Patient Care
We aim to give top-notch healthcare, starting with transfusion medicine. By sticking to pediatric transfusion guidelines, we make sure our patients get the best care.
Future of Transfusion Medicine
We’re dedicated to outstanding patient care and pushing transfusion medicine forward. This means staying updated with the latest pediatric blood Page transfusion guidelines.
FAQ.
What are the recommended pediatric blood transfusion guidelines for platelet transfusions?
The World Health Organization (WHO) has guidelines for safe platelet transfusions in kids. These cover donor selection, blood screening, and how to transfuse.
How are platelet transfusion rates determined in pediatric patients?
We look at several things to decide on platelet transfusions. This includes the patient’s health, why they need the transfusion, and how low their platelets are. We aim to keep risks low and make sure the transfusions work well.
What are the common indications for platelet transfusions in children?
Kids might need platelet transfusions for bleeding, low platelets, or before surgery. We choose the right approach based on the situation.
What are the risks and complications associated with platelet transfusions?
Platelet transfusions are lifesaving but can have side effects. These range from mild issues like fever to serious reactions like anaphylaxis. We watch patients closely after transfusions to catch and treat any problems quickly.
How are platelet transfusions administered safely in pediatric patients?
Giving platelet transfusions safely involves careful steps. We explain the process to the child, check the blood, and get consent. We also monitor the patient during and after the transfusion.
What is the significance of informed consent in pediatric blood transfusions?
Getting consent from parents is key. We also respect cultural views on blood transfusions. This helps us provide the best care while considering ethical issues.
What are the future directions in platelet transfusion research?
Transfusion medicine is always improving. Research focuses on better storage, matching, and new products. We keep up with these advances to give the best care.
How do WHO guidelines impact pediatric transfusion practices globally?
WHO guidelines set a global standard for blood transfusions. They’re critical in pediatric care, where safety is a top priority. Following these guidelines helps us avoid risks.
What factors influence transfusion rates in pediatric patients?
Several things affect how often kids need transfusions. These include how low their platelets are, if they’re bleeding, and their overall health. We use these factors to decide on the right transfusion rate
References
JAMA Network. Evidence-Based Medical Insight. Retrieved from https://jamanetwork.com/journals/jama/fullarticle/2834703
World Health Organization. Evidence-Based Medical Insight. Retrieved from https://www.who.int/publications/i/item/9789240030289
ScienceDirect. Evidence-Based Medical Insight. Retrieved from https://www.sciencedirect.com/science/article/pii/S0268960X19300391