Last Updated on November 13, 2025 by
Knowing about the platelet count is key, for those with health issues like immune thrombocytopenia or before surgery.
A platelet count, or PLT blood test, checks how many platelets are in your blood. These cells are vital for clotting and stopping too much bleeding.

It’s important to have enough platelets to avoid serious bleeding. If your count is too low, the risk of bleeding goes up a lot.
Key Takeaways
- Understanding platelet count is key for knowing bleeding risk.
- A PLT blood test counts the platelets in your blood.
- Platelets are key to clotting and stopping too much bleeding.
- Having enough platelets is vital to avoid serious bleeding problems.
- A low platelet count means a higher risk of bleeding.
Understanding Platelets and Their Function in Hemostasis
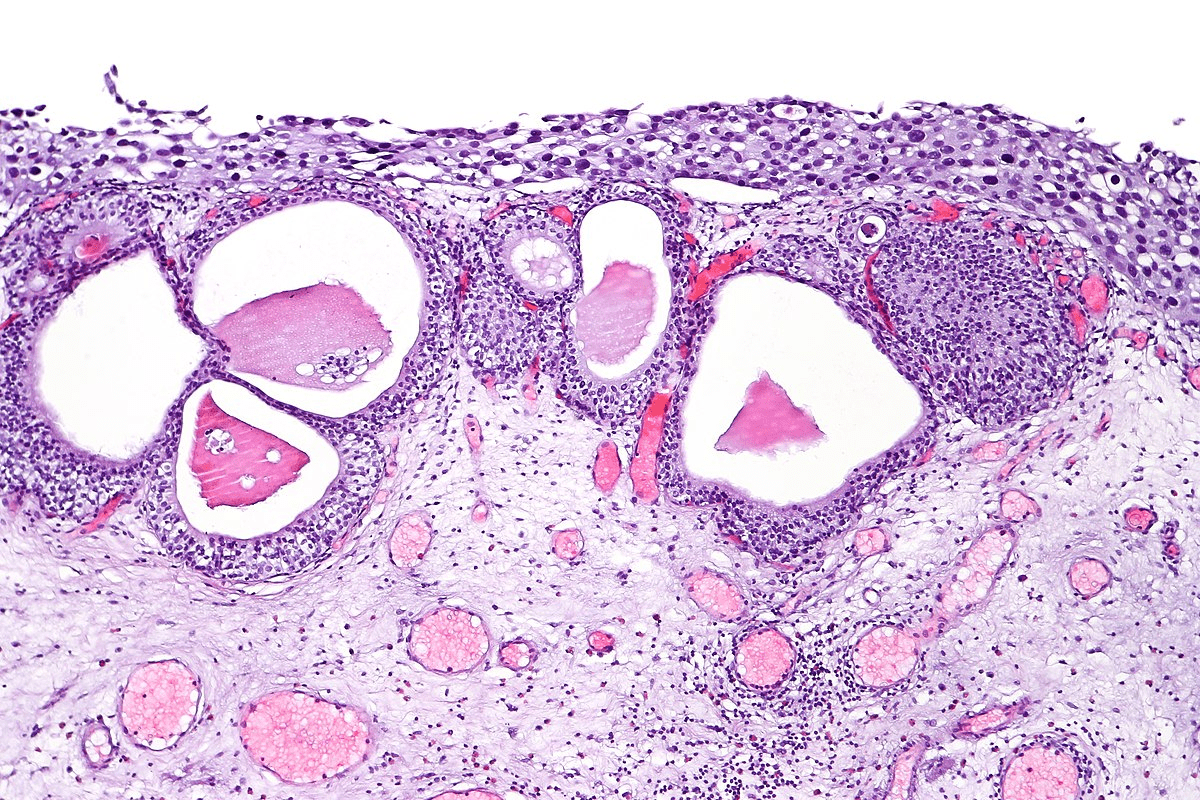
Platelets are tiny blood cells that play a key role in stopping bleeding. They are vital for forming blood clots. This helps keep our blood vessels strong.

What Are Platelets and Their Normal Ranges
Platelets, or thrombocytes, are small, colorless fragments in our blood. They help form clots to stop bleeding. A normal count is between 150,000 to 450,000 platelets per microliter of blood.
This range is important for proper blood clotting. It helps prevent thrombocytopenia, or low platelet count. Different labs might have slightly different ranges, but this is the general guideline.
How Platelets Prevent Bleeding and Maintain Vascular Integrity
When a blood vessel gets hurt, platelets stick to the injury. They clump together to form a plug. This seals the damaged area temporarily.
Chemicals and proteins like von Willebrand factor and fibrinogen help hold the plug in place. This process is key to stopping bleeding and keeping our blood vessels strong.
- Platelet activation and aggregation are critical for clot formation.
- The coagulation cascade starts, creating a fibrin clot that strengthens the platelet plug.
- This ensures bleeding stops and our blood vessels stay intact.
It’s important to understand how platelets work. This knowledge helps us see the risks of low platelet counts. Keeping a healthy platelet count can lower the risk of bleeding problems.
Critical PLT Thresholds That Increase Bleeding Risk
Understanding platelet count thresholds is key to assessing bleeding risk. Platelet count, plays a big role in this. Knowing these thresholds helps doctors manage patients better.
Mild Risk: Platelet Counts Between 50-100 × 10^9/L
A platelet count of 50-100 × 10^9/L means a mild risk of bleeding. Patients might not bleed on their own, but they could during surgery or trauma. Monitoring and adjusting treatment plans is important to avoid problems.
Moderate Risk: Platelet Counts Between 20-50 × 10^9/L
Counts between 20-50 × 10^9/L mean a moderate risk of bleeding. Patients might see more bruising and petechiae. The risk of serious bleeding goes up, mainly with trauma or invasive procedures.
High Risk: Platelet Counts Below 20 × 10^9/L
Counts below 20 × 10^9/L mean a high risk of bleeding. Spontaneous bleeding can happen, and patients face a big risk of hemorrhage. Immediate medical attention is needed to manage severe bleeding.
Severe Risk: Platelet Counts Under 10 × 10^9/L
A count under 10 × 10^9/L is very risky for bleeding. Patients face a high risk of life-threatening hemorrhage. They need urgent medical intervention. Treatment often includes platelet transfusions and other support.
Here’s a quick summary of the PLT thresholds and their bleeding risks:
- Mild Risk: 50-100 × 10^9/L
- Moderate Risk: 20-50 × 10^9/L
- High Risk: Below 20 × 10^9/L
- Severe Risk: Under 10 × 10^9/L

Healthcare providers must understand these thresholds to manage low platelet counts well. Recognizing the risks helps them take the right steps to prevent bleeding.
Clinical Manifestations of Bleeding at Different Platelet Levels
Bleeding signs change with platelet counts. Knowing these signs is key to spotting thrombocytopenia early. As platelets drop, bleeding risks grow, showing different symptoms at each level.
Early Warning Signs of Thrombocytopenia
Look out for mild mucosal bleeding like nosebleeds or gum spots. Also, watch for petechiae, small spots on the skin from tiny bleeds. These signs show up when platelets start to fall.
Mucosal Bleeding and Petechiae
As thrombocytopenia gets worse, mucosal bleeding gets more serious. Petechiae spread too. This bleeding can be in the gut or kidneys. Petechiae show platelet problems, appearing where veins are tight.
Spontaneous Bleeding and Hemorrhage
At very low platelet counts, below 20 × 10^9/L, bleeding risks jump up. Spontaneous bleeding can happen anywhere and is very dangerous. It needs quick medical help.
Duration of Low PLT Count and Cumulative Bleeding Risk
How long platelets stay low affects bleeding risks. Longer times mean higher risks. This shows why quick and good treatment is so important.
Platelet Count Requirements for Medical Procedures and Conditions
Different medical procedures need specific platelet count levels for safety. This is very important in surgeries and interventions where bleeding is a big risk.
Surgical Procedures: From Minor to Major Interventions
The platelet count needed changes with the surgery type. For small surgeries, a count of 50 × 10^9/L is usually enough. But for big surgeries, a count over 80 × 10^9/L is better to lower bleeding risks.
Special Considerations for Neurosurgery (80-100 × 10^9/L)
Neurosurgery is very sensitive. Even a little bleeding can be very dangerous. For neurosurgery, a platelet count of 80-100 × 10^9/L is recommended. This is to prevent serious bleeding in the brain.
Platelet Thresholds in Immune Thrombocytopenia and Hematologic Malignancies
In cases like immune thrombocytopenia and hematologic malignancies, managing platelet count is key. For surgeries, patients with immune thrombocytopenia should have at least 50 × 10^9/L platelets. The needs for hematologic malignancies depend on the condition and treatment.
Knowing these platelet count needs helps doctors make better decisions. It helps lower the risk of bleeding during medical procedures.
Conclusion: Management Strategies for Patients with Low Platelet Counts
It’s key to know the dangers of low platelet counts for good care. People with thrombocytopenia or similar issues need close watch and custom treatment plans. This helps avoid bleeding problems.
Keeping platelet counts right is very important, like before surgery. A normal count is needed for blood to clot properly. Counts too low can raise the chance of bleeding a lot.
Doctors might use platelet transfusions, drugs to boost platelet making, or fix the cause of low counts. Even when counts are high, watching closely is needed to stop blood clots.
Healthcare teams can lessen risks and better patient results by knowing about platelet counts and using the right care plans. Good care for those with low platelet counts means looking at the whole person, not just the count.
FAQ
What is a normal platelet count?
What are the risks associated with a high platelet count?
What is thrombocytopenia, and what are its symptoms?
How do platelets function in hemostasis?
What platelet count is considered safe for surgery?
Can a low platelet count be treated?
What does a PLT blood test measure?
How does a low platelet count affect the body?
References
- Biolato, M., et al. (2023). Minimum platelet count threshold before invasive procedures: A systematic review and expert opinion. Journal of Clinical Medicine, 12(5), 1567. https://pmc.ncbi.nlm.nih.gov/articles/PMC9988645/