Last Updated on December 3, 2025 by Bilal Hasdemir
Post-hysterectomy constipation is a common issue many women face after surgery. They often struggle with bowel movements and find it difficult to pass stool without straining. This raises an important question — is it safe to push to poop after a hysterectomy?
Managing bowel movements after surgery is essential for a smooth and safe recovery. Straining too much can put pressure on the surgical area and slow healing. Understanding post-hysterectomy constipation and learning safe ways to manage it can make recovery more comfortable and effective.
Key Takeaways
- Understand the risks associated with straining during bowel movements after a hysterectomy.
- Learn how to manage constipation effectively post-surgery.
- Discover the importance of gentle bowel movements for recovery.
- Find out how to minimize the risk of complications at the surgical site.
- Get tips on maintaining a healthy bowel routine after surgery.
Understanding Your Body After Hysterectomy
It’s important to know how your body changes after a hysterectomy. This surgery can greatly improve your life but also makes your body adjust in many ways.
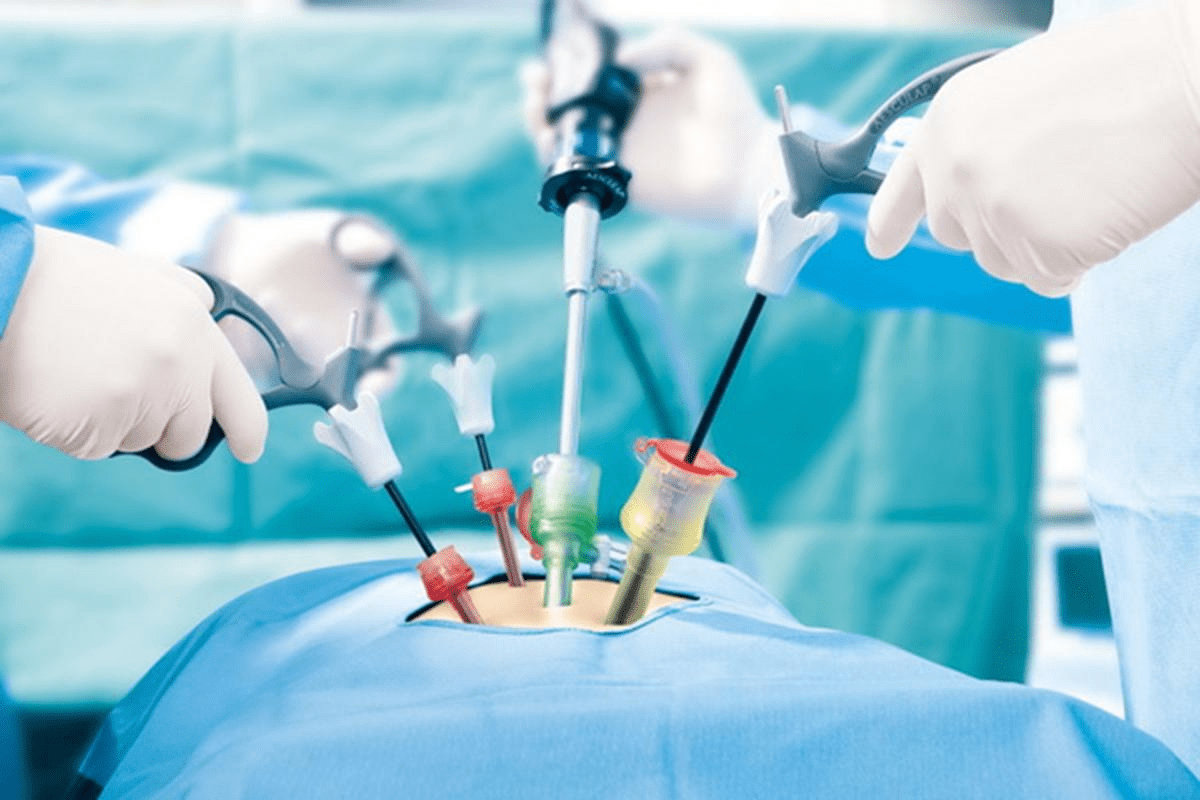
Anatomical Changes Following Surgery
When the uterus is removed, your body changes right away. Other organs move into the empty space. This can affect how you go to the bathroom or use your bladder.
How Surgery Affects Your Digestive System
The surgery can also impact your digestive system. Anesthesia and pain medications can make bowel movements slower, causing constipation. Not moving much after surgery can make this problem worse.
Many women notice changes in their bowel movements after a hysterectomy. A study in the Journal of Minimally Invasive Gynecology found that nearly 40% of women had bowel issues after the surgery.
Initial Recovery Expectations
Right after surgery, you might feel uncomfortable and have trouble moving. It’s key to follow the post-operative instructions from your doctor. This helps your body heal right.
As you get better, pay attention to how your body is changing. Talk to your doctor about any worries or strange feelings. Knowing what to expect and how to manage your recovery can make it easier.
Post-Hysterectomy Constipation: Causes and Mechanisms

Constipation is a common issue after a hysterectomy. Knowing why it happens is key to managing it. Several factors play a role in post-surgery constipation.
Effects of Anesthesia on Bowel Function
Anesthesia during hysterectomy can affect bowel function. General anesthesia can slow down bowel movements. This is because it impacts the muscles in the digestive tract.
This slowing down can cause constipation. The body takes longer to process and eliminate waste.
Impact of Pain Medications on Digestion
Pain medications, like opioids, can cause constipation. They bind to opioid receptors in the gut. This reduces the intestines’ motility.
It also increases water and electrolyte absorption. This makes stools harder and more difficult to pass.
Reduced Physical Activity and Mobility
After surgery, less physical activity can lead to constipation. Physical inactivity slows down food movement in the digestive system. This allows more water absorption, making stools harder.
Surgical Trauma and Intestinal Manipulation
The surgery itself, including intestinal manipulation, can cause trauma. This trauma can stop bowel movements temporarily. This is known as postoperative ileus.
| Cause | Effect on Bowel Movement |
| Anesthesia | Slows down bowel movements |
| Pain Medications (Opioids) | Reduces intestinal motility, hardens stools |
| Reduced Physical Activity | Slows down digestive system |
| Surgical Trauma | Causes temporary halt in bowel movements |
The Dangers of Straining After Hysterectomy
Straining after a hysterectomy can lead to several risks. It can stress the body, affecting recovery. Bowel movements can put extra pressure on the surgical area and tissues around it.
Risks to Surgical Site Healing
Straining can harm the healing at the surgical site. It increases abdominal pressure, which can stress the sutures or staples. This stress may slow healing or even reopen the wound.
It’s important to manage bowel movements carefully to avoid stressing the surgical site. Using stool softeners or other constipation relief as advised by your doctor can help reduce straining.
Potential for Pelvic Floor Damage
Straining can also harm the pelvic floor. These muscles are already stressed from surgery. Excessive straining can weaken or damage them further.
Pelvic floor physical therapy may be suggested to strengthen these muscles and aid in recovery.
Increased Risk of Bleeding and Complications
Straining can raise the risk of bleeding and complications after a hysterectomy. The increased pressure can dislodge clots or disrupt healing tissues. This can lead to hemorrhage or serious issues.
“Patients should be aware of the signs of excessive bleeding, such as heavy vaginal bleeding or severe abdominal pain, and seek immediate medical attention if these symptoms occur.”
Impact on Internal Sutures and Healing Tissues
The internal sutures used in a hysterectomy are key to healing. Straining can stress these sutures, possibly causing complications like suture breakage or adhesions.
Keeping a healthy bowel routine through diet, hydration, and exercise can help avoid straining. It supports the healing of internal tissues.
Is Pushing During Bowel Movements Safe?
It’s important to know the risks of pushing during bowel movements after a hysterectomy. This knowledge helps in a smooth recovery. Patients should be aware of complications from straining during bowel movements.
Medical Recommendations About Straining
Doctors usually advise against straining after a hysterectomy. Straining can put extra pressure on the surgical site. This might cause bleeding or damage to internal sutures. Following a gentle approach to bowel movements is key to avoid these risks.
“Patients should be counseled on the importance of avoiding straining during bowel movements to prevent complications such as hemorrhage or dehiscence at the surgical site.”
Differences Between Gentle Pressure and Harmful Straining
There’s a thin line between gentle pressure and harmful straining. Gentle pressure is usually safe and might be needed for constipation. But, harmful straining uses too much force and can cause serious problems. It’s important to know the difference to manage bowel movements safely.
Alternative Techniques to Pushing
There are many ways to manage bowel movements without pushing or straining. Some include:
- Using a stool softener to ease stool passage
- Choosing the right sitting position on the toilet to reduce strain
- Using gentle breathing techniques to relax the pelvic floor muscles
- Supporting the abdomen during bowel movements to lessen pressure on the surgical site
Timeline for Resuming Normal Bowel Habits
The time it takes to get back to normal bowel habits after a hysterectomy varies. It can take several weeks. The type of surgery, the patient’s health, and following post-operative instructions play a role in this timeline.
| Timeline | Expected Changes in Bowel Habits |
| First Week | Constipation is common due to anesthesia and pain medications. |
| 2-4 Weeks | Bowel habits start to normalize as physical activity increases and medications are adjusted. |
| 6-8 Weeks | Most patients see a return to their pre-surgery bowel habits. |
Timeline of Bowel Function Recovery
Knowing how long it takes for bowel function to recover after a hysterectomy is key. It helps manage expectations and aids in a smooth healing process. Everyone recovers differently, but there are general guidelines to follow.
First 72 Hours Post-Surgery
In the first 72 hours after surgery, bowel movements might be slow. This is because of anesthesia and pain meds. It’s normal for bowel movements to be irregular or not happen at all during this time. Drinking plenty of water and eating foods that are easy to digest is recommended.
First Week Post-Surgery
In the first week, bowel movements may start to feel more normal. They can be irregular, though. Some people might get constipated, while others might have more frequent bowel movements. Taking short walks can help get things moving again.
Weeks 2-6 After Surgery
By weeks 2-6, most people see a big improvement in their bowel habits. The body starts to adjust to the surgery changes, and bowel movements get more regular. Eating more fiber can help with this adjustment.
Long-term Digestive Changes
Over time, some people might notice changes in their bowel habits. These can include changes in how often they go, how solid their stools are, or how easy it is to have a bowel movement. Eating well, staying hydrated, and exercising regularly can help manage these changes.
| Timeframe | Bowel Function Changes | Recommendations |
| First 72 Hours | Sluggish bowel movements, irregular or absent | Stay hydrated, easy-to-digest diet |
| First Week | Bowel movements start to return, may be irregular | Gentle physical activity, hydration |
| Weeks 2-6 | Bowel habits improve, becoming more regular | Dietary adjustments (increase fiber), physical activity |
| Long-term | Possible changes in bowel habits | Healthy diet, hydration, regular physical activity |
Safe Techniques for Bowel Movements After Surgery
Using the right techniques for bowel movements after a hysterectomy is key to a smooth recovery. It’s important to be careful with your daily activities, including bowel movements. This helps avoid complications and ensures a smooth healing process.
Proper Sitting Position on the Toilet
Sitting right on the toilet can greatly affect your bowel movements. We suggest sitting with your feet flat on the floor or on a footstool. Keep your back straight and lean forward slightly. This helps straighten your rectum and makes passing stools easier.
Gentle Breathing Techniques
Gentle breathing can relax your body during bowel movements, reducing strain. Breathe slowly in through your nose and out through your mouth. This calms your nervous system and makes the process easier.
Supporting Your Abdomen During Movements
Supporting your abdomen during bowel movements can offer comfort and reduce strain on your surgical site. Gently press a clean cloth or your hands against your abdomen. This support stabilizes the area and makes bowel movements less uncomfortable.
Using Assistive Devices Safely
There are many assistive devices that can make bowel movements safer and more comfortable after a hysterectomy. These include toilet stools, grab bars, and raised toilet seats. Always ensure they are securely installed and follow the manufacturer’s instructions.
| Assistive Device | Benefit | Safety Tip |
| Toilet Stool | Elevates feet to promote a natural squatting position | Ensure it’s stable and won’t slip |
| Grab Bars | Provides support when sitting down or standing up | Install securely to bear weight |
| Raised Toilet Seat | Makes it easier to sit down and stand up | Check that it’s firmly attached to the toilet |
By using these safe techniques, you can reduce discomfort and lower the risk of complications after a hysterectomy. Always talk to your healthcare provider if you have any concerns or questions about your bowel movements or recovery.
Hydration and Its Role in Preventing Constipation
Drinking enough water is key to avoiding constipation after a hysterectomy. Water makes stool softer, making it easier to pass. This helps prevent constipation.
Optimal Daily Fluid Intake During Recovery
It’s important to drink plenty of fluids while recovering. This helps your body heal and keeps your bowels regular. Aim for 8-10 glasses of fluid a day. Your needs might change based on how active you are and where you live.
Table: Daily Fluid Intake Recommendations
| Activity Level | Recommended Daily Fluid Intake |
| Low Activity | 8 glasses (64 oz) |
| Moderate Activity | 9-10 glasses (72-80 oz) |
| High Activity | 11-12 glasses (88-96 oz) |
Best Types of Fluids for Digestive Health
Not all drinks are good for your digestive health. Water is the best because it’s calorie-free and doesn’t have sugars or caffeine. Herbal teas and clear broths are also good choices.
“Adequate hydration is key to avoiding constipation. Water softens stool, making it easier to pass.”American Gastroenterological Association
Signs of Dehydration to Watch For
Dehydration can sneak up on you, which is common during recovery. Look out for dark yellow or amber urine, dry mouth, feeling tired, and dizzy. If you notice these signs, drink more fluids.
Creating a Hydration Schedule
To drink enough, make a hydration plan. Split your daily water into smaller amounts and drink at set times. You can also use reminders on your phone or a hydration app to help.
By focusing on hydration and following these tips, you can lower your risk of constipation after a hysterectomy. This will also help your recovery.
Dietary Strategies to Ease Bowel Movements
After a hysterectomy, managing bowel movements is key. Eating the right foods can help with constipation and keep your digestive system healthy. A balanced diet is important during recovery.
Fiber-Rich Foods to Include Gradually
Adding more fiber to your diet is a smart move. Start by slowly adding foods high in fiber. This helps soften your stool and keeps bowel movements regular.
- Fruits: Berries, apples, and pears are high in fiber and antioxidants.
- Vegetables: Broccoli, carrots, and leafy greens are rich in fiber and essential nutrients.
- Whole Grains: Brown rice, quinoa, and whole-wheat bread provide sustained fiber intake.
- Legumes: Beans, lentils, and chickpeas are excellent sources of fiber and protein.
Foods to Avoid During Recovery
Some foods can make constipation and discomfort worse during recovery. It’s best to limit or avoid these to help with digestion.
| Food Category | Examples | Reason to Avoid |
| Dairy | Cheese, milk, ice cream | Can cause constipation and bloating |
| Processed Foods | Fast food, processed meats | Low in fiber, high in unhealthy fats |
| High-Fat Foods | Fried foods, fatty meats | Can slow down digestion |
Meal Planning for Optimal Digestion
Good meal planning is essential for digestion. Focus on fiber-rich foods and balance your diet for better bowel health.
“A balanced diet that includes a variety of fiber-rich foods can significantly improve bowel movements and overall digestive health.” – Nutrition Expert
Small, Frequent Meals vs. Large Meals
Eating smaller, more frequent meals can ease digestion and reduce discomfort. This is very helpful during recovery.
- Benefits of Small Meals: Easier to digest, reduces strain on the digestive system.
- Benefits of Frequent Meals: Maintains energy levels, supports overall nutritional intake.
By following these dietary tips, patients can better manage bowel movements and support their recovery after a hysterectomy.
Over-the-Counter Solutions for Constipation Relief
Managing constipation after a hysterectomy is important for comfort. Over-the-counter solutions are a big help. Finding relief from constipation can be tough, but there are many options.
Safe Stool Softeners After Hysterectomy
Stool softeners are a gentle way to manage constipation. They make stool softer and easier to pass. Docusate sodium is a good over-the-counter option. Always follow the dosage and talk to your doctor before starting.
Appropriate Laxatives and Their Usage
Laxatives can quickly help with constipation, but use them wisely. There are stimulant laxatives and osmotic laxatives. Bisacodyl is a stimulant, and polyethylene glycol is an osmotic one. Choose the right one and follow the instructions to avoid problems.
Natural Supplements That May Help
Natural supplements can also help with constipation. Psyllium husk is a fiber supplement that promotes regular bowel movements. Prune juice and flaxseed can also soften stool and improve digestion. Always check with your doctor before trying new supplements.
Timing Medications for Maximum Effectiveness
When you take constipation relief medications matters a lot. Take them as directed or as your doctor advises. Consistency is key for best results. Also, stay hydrated and eat fiber-rich foods to help.
Physical Activity Guidelines to Promote Bowel Movements
Physical activity is key to healthy bowel movements after a hysterectomy. The right activities at the right time can help your recovery. They can also prevent bowel movement problems.
Safe Movements in the First Weeks
In the first weeks after surgery, focus on gentle movements. Stretching in bed or light leg lifts can help. Avoid heavy lifting, bending, or hard activities during this time.
Gentle Walking and Its Benefits
Gentle walking is highly recommended after a hysterectomy. It helps with bowel movements and overall recovery. It improves circulation and lowers blood clot risk. Start with short walks and increase as you can.
Gradual Return to Exercise
As you recover, you can start regular exercise again. Listen to your body and don’t overdo it. Begin with low-impact exercises like yoga or swimming. They are easy on the body and good for digestion.
Activities That Support Digestive Health
Some activities are great for digestive health and bowel movements. These include:
- Abdominal massage
- Pelvic tilts
- Light cardio exercises
- Yoga poses that target the abdominal area
| Activity | Benefits for Bowel Movements |
| Gentle Walking | Stimulates bowel movements, improves circulation |
| Abdominal Massage | Aids in digestion, relieves constipation |
| Pelvic Tilts | Helps stimulate bowel movements, strengthens core |
Adding these activities to your recovery plan can help with bowel movements. They support your overall health after a hysterectomy.
Pelvic Floor Considerations After Hysterectomy
It’s important to know how a hysterectomy changes the pelvic floor. This change helps manage bowel function and aids in healing. The pelvic floor is made of muscles, ligaments, and tissues. It supports pelvic organs, keeps them in place, and helps with bowel movements.
Impact of Surgery on the Pelvic Floor
A hysterectomy can change the pelvic floor a lot. The removal of the uterus can shift organs and weaken muscles. Understanding these changes is key to a smooth recovery.
Gentle Pelvic Floor Exercises for Recovery
Doing gentle pelvic floor exercises, like Kegels, can help. These exercises make the muscles stronger. Start slowly and with a healthcare provider’s guidance to avoid injury.
- Begin with short contractions and gradual releases.
- Increase the duration and frequency as advised by your healthcare provider.
- Practice deep breathing to help relax the pelvic floor muscles.
Coordination Between Pelvic Floor and Bowel Function
The pelvic floor and bowel function are closely connected. Weakness in the pelvic floor can cause bowel problems. Strengthening the pelvic floor can improve bowel habits and reduce complications.
“Pelvic floor rehabilitation is a critical component of post-hysterectomy care, helping patients regain control over their bowel movements and improving their quality of life.” – Expert in Pelvic Floor Rehabilitation
When to Consult a Pelvic Floor Specialist
If you have ongoing bowel issues, pain, or incontinence after a hysterectomy, see a pelvic floor specialist. They can give personalized advice, manage issues, and support your recovery.
By understanding the effects of hysterectomy on the pelvic floor and taking steps like gentle exercises, patients can better their recovery. They can also keep their bowel function in check.
Hormonal Changes and Their Impact on Digestion
After a hysterectomy, hormonal changes can affect digestion. We will look at how these changes impact digestion and what patients can do to manage symptoms.
Ovary Removal and Hormonal Shifts
Removing ovaries during a hysterectomy can cause menopause right away. This leads to big hormonal changes. These changes can mess with digestion, causing issues like constipation.
Key effects of ovary removal on digestion:
- Changes in bowel habits
- Increased risk of constipation
- Potential for weight gain or loss
Estrogen’s Role in Digestive Function
Estrogen is key for healthy digestion. It helps control bowel movements and keeps the gut healthy. Without ovaries, estrogen levels drop, leading to digestive problems.
Estrogen’s benefits for digestion include:
- Regulating bowel movements
- Maintaining gut health
- Influencing the gut microbiome
Hormone Replacement Therapy Considerations
Hormone Replacement Therapy (HRT) is often used after ovary removal. It helps by adding estrogen to counteract hormonal changes. This can ease digestive issues.
Considerations for HRT:
- Potential benefits for digestive health
- Risks and side effects
- Individualized treatment plans
Long-term Digestive Management Strategies
Managing digestion long-term after a hysterectomy needs a broad approach. This includes changing diets, staying hydrated, and adding physical activity. The activity should match the patient’s recovery stage.
Long-term strategies include:
- Dietary adjustments to ease digestion
- Adequate hydration
- Gradual return to physical activity
Warning Signs: When to Contact Your Doctor
After a hysterectomy, knowing when to call your doctor is key. Some pain is okay, but other signs might mean you need help fast.
Severe or Prolonged Constipation
Constipation after a hysterectomy is common. But, if it’s really bad or lasts too long, it’s a red flag. If you can’t go for more than three days or have severe abdominal pain, call your doctor. Also, if you see bloody stools or vomiting, get help right away.
Signs of Bowel Obstruction
A bowel obstruction is a serious issue after surgery. Look out for severe abdominal pain, vomiting, and obstipation. If you see these signs, get medical help fast.
Symptoms of Infection or Complications
Watching for infection signs is important. Look for fever, increased pain, redness or swelling around the incision site, or foul-smelling discharge. If you see any, call your doctor right away.
Unusual Pain or Bleeding During Bowel Movements
Seeing unusual pain or bleeding during bowel movements is a warning. If you have heavy bleeding, severe pain, or passage of clots, talk to your doctor. These could mean problems like internal sutures being affected.
In short, knowing these signs and talking to your doctor can help your recovery go smoothly after a hysterectomy.
Patient Experiences with Post-Surgery Bowel Issues
After a hysterectomy, many patients face bowel problems that affect their recovery. These issues differ from person to person. They depend on the surgery type, health, and post-op care.
Common Challenges Reported by Patients
Patients often deal with constipation, hard bowel movements, and discomfort early on. Some also see lasting changes in their bowel habits. These changes can last weeks or months.
Key challenges include:
- Constipation and straining during bowel movements
- Abdominal bloating and discomfort
- Changes in bowel habits, such as diarrhea or constipation
- Pain or discomfort during bowel movements
Successful Management Strategies
It’s key to manage bowel issues well for a smooth recovery. Patients find help in diet changes, staying hydrated, and gentle exercise.
Some successful strategies include:
- Increasing fluid intake to soften stool
- Incorporating fiber-rich foods to promote regular bowel movements
- Engaging in gentle exercises, such as walking, to stimulate bowel function
- Using stool softeners or laxatives as recommended by healthcare providers
Recovery Timeline Expectations
Knowing the recovery timeline helps manage expectations and anxiety. Bowel function usually returns to normal in a few weeks. But, this can vary.
General recovery timeline:
- First week: Bowel movements may be irregular, with possible constipation
- 2-6 weeks: Gradual return to normal bowel habits
- Long-term: Some patients may experience persistent changes in bowel habits
Emotional Aspects of Digestive Challenges
The emotional side of bowel issues is important. Patients might feel frustrated, anxious, or embarrassed by their symptoms.
It’s essential to acknowledge these feelings and seek support when needed. Healthcare providers can offer guidance and reassurance. They help patients deal with this tough part of their recovery.
Conclusion
Managing bowel movements after a hysterectomy is key for a smooth recovery. Many women face constipation after surgery. But, with the right strategies, it can be managed well.
Understanding your body’s changes after surgery is important. Drinking enough water, eating fiber-rich foods, and doing gentle exercises help. These actions promote healthy bowel movements and lower the risk of complications.
Knowing the recovery timeline and watching for warning signs is vital. Following the guidelines in this article helps you deal with constipation after surgery. It also supports your overall health during recovery.
FAQ
Is it okay to push to poop after a hysterectomy?
It’s not a good idea to strain or push hard after a hysterectomy. This can harm the surgical site and pelvic floor. Instead, try gentle techniques and manage constipation with diet, hydration, and safe exercise.
What are the main causes of constipation after a hysterectomy?
Constipation after a hysterectomy can come from several sources. These include anesthesia effects, pain meds, less activity, and surgery trauma. Knowing these causes helps in managing and preventing constipation.
How can I manage constipation after a hysterectomy?
To manage constipation, stay hydrated and eat foods high in fiber. Also, do gentle exercises and consider safe laxatives or stool softeners. Using safe bowel movement techniques is key.
What are the risks of straining during bowel movements after a hysterectomy?
Straining can be risky, causing damage to the surgical site and pelvic floor. It can also increase bleeding risk and affect internal sutures. Avoid straining and use gentle techniques instead.
How long does it take for bowel function to recover after a hysterectomy?
Recovery time for bowel function varies. Bowel movements may be slow in the first 72 hours. They usually start to get better in the first week and keep improving. Long-term changes in digestion can also happen.
What are some safe techniques for bowel movements after a hysterectomy?
Safe techniques include sitting right, using gentle breathing, and supporting your abdomen. You might also use assistive devices. These methods reduce strain and discomfort.
How important is hydration in preventing constipation after a hysterectomy?
Staying hydrated is very important to prevent constipation. Drinking enough water helps soften stool and promotes regular bowel movements. Drink plenty of water and other hydrating fluids during recovery.
What dietary changes can help ease bowel movements after a hysterectomy?
Eating foods high in fiber and avoiding constipation-causing foods can help. Small, frequent meals are also beneficial. These changes can ease bowel movements.
Are there any over-the-counter solutions for constipation relief after a hysterectomy?
Yes, safe over-the-counter solutions include stool softeners, laxatives, and natural supplements. Always use these with a healthcare provider’s guidance and at the right time for best results.
How can physical activity promote bowel movements after a hysterectomy?
Gentle activities like walking can help stimulate bowel movements. Gradually adding more exercise and activities that support digestive health can also be beneficial.
How does a hysterectomy affect the pelvic floor, and what exercises can help?
A hysterectomy can affect the pelvic floor. Gentle exercises can help in recovery and improve pelvic floor and bowel function coordination. A pelvic floor specialist can provide personalized advice.
Can hormonal changes after a hysterectomy affect digestion?
Yes, hormonal changes, like those from removed ovaries, can affect digestion. Understanding estrogen’s role in digestion and considering hormone replacement therapy is important for long-term digestive health.
What are the warning signs that I should contact my doctor about after a hysterectomy?
Warning signs include severe or prolonged constipation, bowel obstruction signs, infection symptoms, and unusual pain or bleeding. Seek medical help if you notice any of these.
Reference:
Hysterectomy Does Not Cause Constipation – JP Roovers, PMC, 2008