Last Updated on December 2, 2025 by Bilal Hasdemir
Step-by-step guide on how to prepare gastrointestinal surgery, including dietary changes and necessary tests. Nearly 1 million Americans have gastrointestinal surgery every year. Many have a better recovery because of good preoperative care. Effective preparation is key to reduce risks and ensure a good outcome.
Preparing for surgery involves more than the procedure alone. It includes medical checks, talking to an anesthesiologist, and changing your lifestyle. Knowing these steps can make your surgery and recovery better.
Key Takeaways
- Understand the importance of medical clearance before surgery.
- Follow specific dietary guidelines to prepare for surgery.
- Make necessary lifestyle modifications to enhance recovery.
- Be aware of the role of anesthesia consultation in preoperative care.
- Plan for post-operative care to ensure a smooth recovery.
Understanding Gastrointestinal Surgery

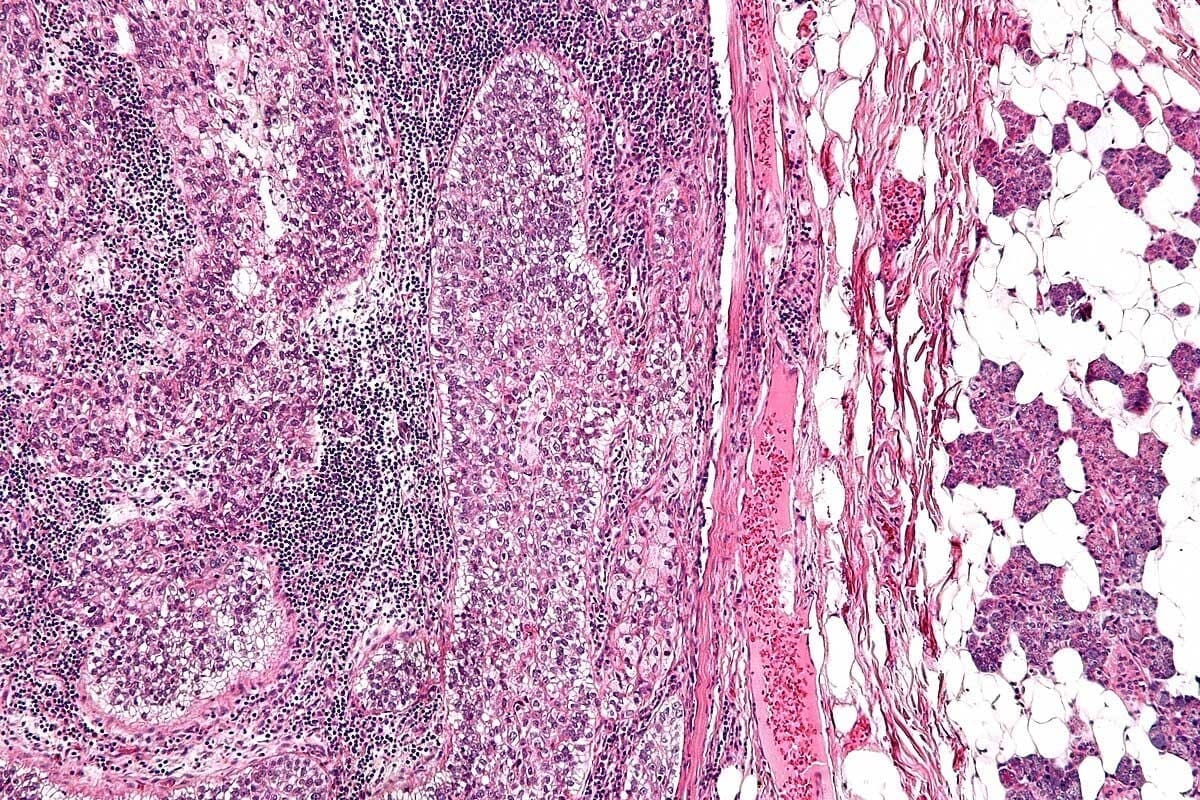
It’s important for patients to understand gastrointestinal surgery. This surgery treats many digestive system issues. It involves complex procedures.
Common Types of Gastrointestinal Surgeries
Gastrointestinal surgeries include several types. These are resections, repairs, and reconstructions. Each type treats different conditions and needs specific preparation.
- Resections: This involves removing a part of the intestine or stomach with disease.
- Repairs: It fixes defects or damage in the gastrointestinal tract.
- Reconstructions: It aims to fix the digestive system’s normal function after surgery or disease.
Why Proper Preparation Matters
Proper preparation is key to reduce risks and get the best results from surgery. Patients need to do medical tests pre surgery. These include blood work and imaging scans.
- Medical tests help find out how bad the condition is and plan the surgery.
- Imaging scans, like CT scans or MRI, show detailed views of the body and any problems.
- Patients with certain health issues might need cardiologist clearance to make sure they can safely have surgery.
Knowing the type of surgery needed and preparing well can greatly improve outcomes and recovery.
Initial Consultation with Your Surgeon
Your first meeting with the surgeon is key to getting ready for surgery. It’s a chance to talk about the surgery, any worries you have, and what your care will be like.
Essential Questions to Ask
Make a list of questions for your surgeon before you meet. Ask about their experience with the surgery, possible risks, and what recovery will be like.
- What experience do you have with this type of gastrointestinal surgery?
- What are the possible risks and complications of the procedure?
- How will I be taken care of after the surgery?
Understanding the Informed Consent Process
The informed consent process is very important before surgery. Your surgeon will explain the surgery, risks, and benefits. This helps you make a well-informed choice about your care.
It’s important to read the consent form carefully. If you don’t understand something, ask your surgeon.
Considering a Second Opinion
Some patients might want to get a second opinion before surgery. This can give more insight into your condition and treatment plan. It can help clear up any doubts.
If you’re thinking about a second opinion, talk to your surgeon. They can share their view and help decide what’s best for you.
Medical Clearance Requirements
Before surgery on the stomach, patients need medical clearance. This is a key step. It involves tests to make sure they’re ready for the surgery.
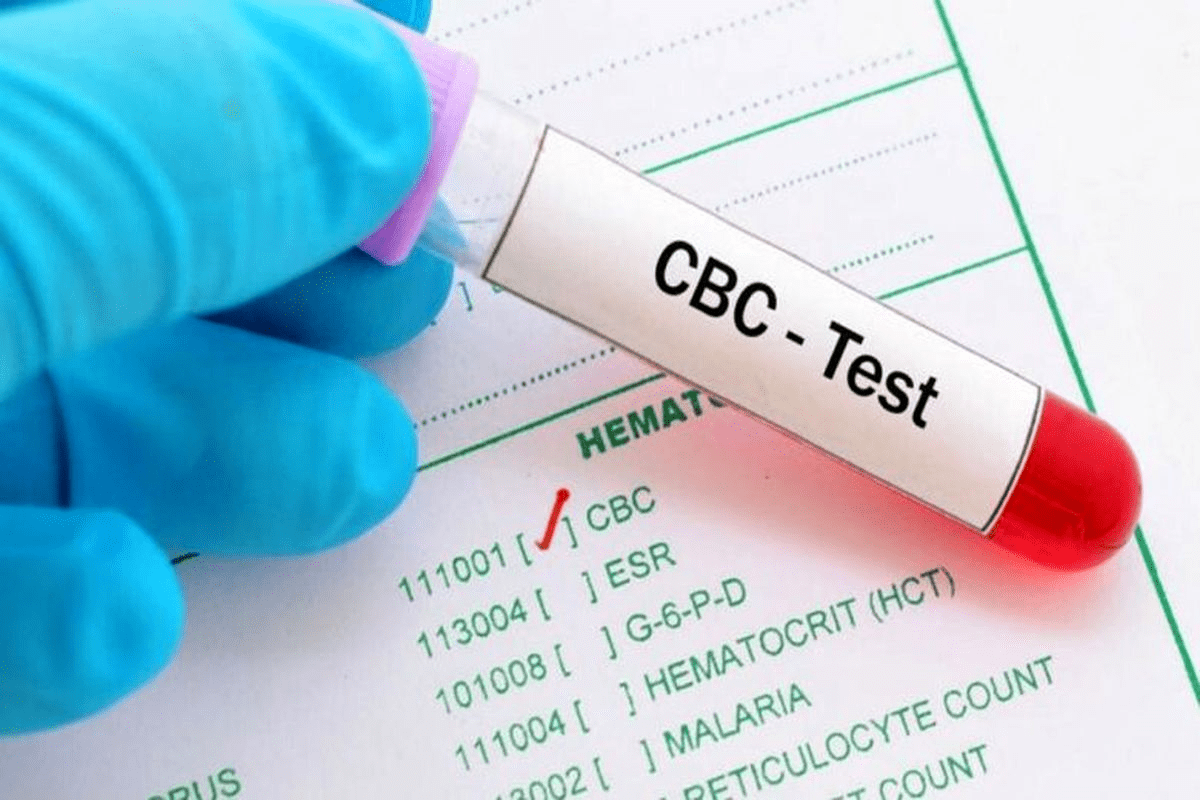
Required Blood Work and Lab Tests
Surgeons check a patient’s health with blood work and lab tests. These tests help find any risks. They include:
- Complete Blood Count (CBC) to check for anemia or infection
- Blood chemistry tests to evaluate liver and kidney function
- Coagulation studies to assess bleeding risks
- Blood type and cross-match in case of a blood transfusion
Table 1: Common Blood Work and Lab Tests
Test | Purpose |
CBC | Checks for anemia or infection |
Blood Chemistry | Evaluates liver and kidney function |
Coagulation Studies | Assesses bleeding risks |
Imaging Scans and Diagnostic Procedures
Imaging scans and other tests are key for checking the stomach and nearby areas. They include:
- Computed Tomography (CT) scans to see inside organs
- Endoscopy to look inside the digestive tract
- Ultrasound to check liver or other organ function
Cardiac Clearance for High-Risk Patients
Patients with heart problems or at risk for heart issues need cardiac clearance. This means talking to a cardiologist. They might do tests like:
- Electrocardiogram (ECG) to check heart rhythm
- Stress test to see how the heart works under stress
- Echocardiogram to look at heart structure and function
Getting medical clearance helps lower surgery risks. It makes recovery easier for patients.
Anesthesia Consultation and Preparation
Getting ready for gastrointestinal surgery means taking a few important steps. One key step is a detailed anesthesia consultation. This meeting is vital to make sure you’re ready for the anesthesia part of your surgery.
What to Expect During Your Anesthesia Consultation
You’ll meet with an anesthesiologist during your consultation. They will talk about your medical history, past surgeries, and current medications. This info helps decide the best anesthesia for you.
Key topics to be covered during the consultation include:
- Your overall health and any pre-existing conditions
- Previous experiences with anesthesia, including any complications
- The type of anesthesia to be used for your surgery
- Potential risks and side effects associated with the anesthesia
Discussing Anesthesia Options and Risks
Your anesthesiologist will go over the different anesthesia options for your surgery. They will talk about the good and bad sides of each. This helps you choose the best care for you.
It’s essential to ask questions during this consultation, such as:
- What type of anesthesia is most suitable for my procedure?
- Are there any specific risks associated with the recommended anesthesia?
- How will my pain be managed after surgery?
Previous Anesthesia Reactions to Report
If you’ve had anesthesia before, tell your anesthesiologist about any bad reactions. This info is key for your anesthesia plan.
Reactions to report include:
- Nausea or vomiting
- Allergic reactions
- Difficulty breathing or other respiratory issues
By sharing your past experiences and current health, your anesthesiologist can create a plan just for you. This plan aims to reduce risks and keep you comfortable during and after surgery.
Medication Management Before Surgery
Knowing how to adjust your medications before surgery is key to a good outcome. Always follow your surgeon’s advice on which medicines to keep taking or stop before your surgery.
Medications to Stop Before Surgery
Some medicines can raise the risk of bleeding or mix badly with anesthesia. Blood thinners like warfarin, aspirin, and clopidogrel are often stopped a few days before surgery. But, how long depends on the medicine and your health.
Other medicines that might need to be stopped or changed include:
- Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen
- Certain herbal supplements that can affect bleeding or anesthesia
Medications to Continue Taking
Not all medicines need to be stopped. Medications for chronic conditions like high blood pressure, diabetes, or asthma are usually kept up unless told to stop by your surgeon.
Tell your healthcare provider about all the medicines you’re taking. This includes:
- Prescription drugs
- Over-the-counter medications
- Vitamins and supplements
Allergy Considerations and Documentation
Telling your healthcare team about any allergies is very important. This includes allergies to medicines, latex, or other substances that might be used during surgery. Documenting your allergies helps keep you safe and prevents bad reactions during surgery.
Here’s a quick guide on what to talk about with your healthcare provider about medication and allergies:
Medication/Allergy Type | Action Required | Notes |
Blood Thinners | Stop a few days before surgery | Consult your surgeon for specific instructions |
Chronic Condition Medications | Continue as directed | Inform your surgeon about all medications |
Medication Allergies | Document and inform healthcare team | Ensure your medical records are updated |
By managing your medicines and documenting allergies, you can help make your surgery safe and successful.
How to Prepare for Gastrointestinal Surgery: Dietary Guidelines
Getting your diet right before gastrointestinal surgery is key for a good outcome. A balanced diet helps your body get ready for surgery and recover well.
Nutritional Optimization Before Surgery
Nutritional optimization is more than just eating healthy. It’s about making sure your body has the nutrients it needs to heal and recover. A diet rich in proteins, vitamins, and minerals is essential. Proteins help repair, vitamins aid in healing, and minerals support bodily functions.
Eat lean proteins like chicken, fish, and legumes. Whole grains, fruits, and vegetables give you the vitamins and minerals you need. Drinking plenty of water is also important.
Pre-Surgery Diet Recommendations
In the weeks before surgery, eat foods that are easy to digest and full of nutrients. Avoid high-fiber and spicy foods to reduce discomfort. Stick to bland foods like bananas, rice, applesauce, and toast (BRAT diet) if your doctor suggests it.
Food Group | Recommended Foods | Foods to Avoid |
Proteins | Lean meats, fish, eggs, tofu | Processed meats, high-fat foods |
Fruits and Vegetables | Fresh, cooked, or canned fruits and vegetables | Raw or high-fiber options if not tolerated |
Grains | White bread, pasta, rice | Whole grains, high-fiber cereals |
Supplements to Consider or Avoid
While a balanced diet is important, some supplements can help. But always talk to your doctor before taking any supplements. Some can interact with medications or have bad effects during surgery.
- Consider: Protein supplements if you’re having trouble getting enough protein from food.
- Avoid: Herbal supplements like ginkgo biloba, garlic, and ginger as they can increase bleeding risk.
Bowel Preparation Protocols
Before surgery, patients must clean their bowels. This step is key to avoid complications. It makes sure the colon is clean, reducing infection risks and improving surgery results.
Laxatives and Cleansing Solutions
Laxatives and cleansing solutions are used for bowel prep. They come in different forms like oral solutions, suppositories, or enemas. The choice depends on the surgery type, patient health, and surgeon’s preference.
Common laxatives include:
- MiraLAX (polyethylene glycol)
- Dulcolax (bisacodyl)
- Fleet Phospho-Soda (sodium phosphate)
It’s vital to follow your healthcare provider’s exact instructions. The laxative type and dosage can differ.
Dietary Restrictions During Bowel Prep
Changing your diet is a big part of bowel prep. You’ll be on a clear liquid diet the day before surgery. This includes:
- Clear broths
- Electrolyte-rich drinks like sports drinks
- Clear juices like apple or grape juice
- Water
Staying away from solid foods and some liquids is key. It helps make sure your bowel is empty and clean for surgery.
Timeline for Bowel Preparation
The bowel prep timeline varies based on your healthcare provider’s instructions. It usually starts a day or two before surgery. Following this timeline is important for effective cleansing.
Typical steps include:
- Starting a clear liquid diet 24 hours before surgery
- Taking laxatives or cleansing solutions as directed, usually the evening before or morning of surgery
- Completing the bowel prep by the time specified by your healthcare provider
Fasting Guidelines Before Surgery
It’s key for patients getting surgery in the stomach area to know about fasting rules. These rules help avoid problems during and after surgery. Following them is important for a safe surgery.
Standard NPO (Nothing by Mouth) Instructions
NPO means nothing to eat or drink. Doctors tell patients to not eat or drink anything for a few hours before surgery. This time can be 8 to 12 hours, depending on the surgery and the patient’s health.
It’s important to stick to these rules to avoid choking on stomach contents during surgery. Patients should stop eating solid foods and most liquids at the right time. This makes sure their stomach is empty during the surgery.
Clear Liquid Allowances
Some patients can drink clear liquids before surgery. Clear liquids are things like water, clear broths, and some sports drinks. Drinking these can help keep patients hydrated without the risk of choking.
But, it’s important to listen to the doctor’s advice on clear liquids. The kind and amount allowed can change based on the surgery and the patient’s needs.
Special Considerations for Diabetic Patients
Diabetic patients need special care before surgery. Keeping blood sugar levels right is important to avoid too low or too high blood sugar. They should talk to their doctor for advice on managing their diabetes before surgery.
Doctors might need to change medication or diet to keep blood sugar safe. It’s important to watch blood sugar levels closely before surgery. Patients should be ready to change their plan if needed.
Lifestyle Modifications for Optimal Surgical Outcomes
Getting your body ready for surgery can make recovery easier and faster. Healthy habits before surgery improve your physical health and lower the chance of problems during and after surgery.
Smoking Cessation Strategies
Smoking increases the risk of surgery complications like infections and slow healing. It’s best to quit smoking 4-6 weeks before surgery. Here are ways to stop smoking:
- Ask your doctor about quitting programs and medicines.
- Try nicotine replacement therapy (NRT) or prescription drugs for withdrawal.
- Avoid things that make you want to smoke.
- Join a support group or counseling for help.
The American Cancer Society says quitting smoking improves your health and lowers surgery risks.
“Quitting smoking is one of the most important steps you can take to improve your health, specially if you’re facing surgery.”
Alcohol Restriction Guidelines
Drinking alcohol before surgery can lead to bleeding, affect anesthesia, and slow recovery. Stop drinking alcohol at least 48 hours before surgery. Follow these guidelines:
Alcohol Consumption Level | Recommended Cessation Period |
Moderate Drinking | At least 48 hours before surgery |
Heavy Drinking | At least 1 week before surgery |
Talk to your healthcare provider about your drinking habits to find the best plan for you.
Physical Activity Recommendations
Regular exercise before surgery boosts your heart health, helps recovery, and lowers risks. Here are some tips:
- Do at least 30 minutes of moderate exercise most days.
- Avoid intense exercises that might hurt your body.
- Try low-impact activities like walking, swimming, or cycling.
Being active before surgery can improve your surgery results. Health experts say being active is key for a healthy lifestyle, even when preparing for surgery.
Mental and Emotional Preparation
Starting your journey to a successful surgery is all about mental and emotional prep. As you get ready for your surgery, it’s key to manage your mental health. This ensures a smooth recovery and the best results.
Managing Anxiety and Stress
Feeling anxious and stressed is normal before surgery. Managing these feelings is vital for your well-being. Try deep breathing, progressive muscle relaxation, and visualization to calm your mind and body.
Staying in touch with loved ones or joining a support group can also help. Sharing your journey and learning from others can be very comforting.
Relaxation Techniques and Mindfulness
Using relaxation techniques and mindfulness can lower your stress and boost your mental health prep. Mindfulness is about being in the moment, focusing on your breath, and letting go of worries.
Technique | Description | Benefits |
Meditation | Focusing your mind on a single point | Reduces stress, improves focus |
Deep Breathing | Slow, deliberate breathing | Calms the nervous system |
Progressive Muscle Relaxation | Tensing and relaxing muscle groups | Reduces physical tension |
Setting Realistic Expectations
Having realistic expectations about your surgery and recovery is key. Recovery times can differ, so be patient with your body as it heals.
Talk to your healthcare provider about what to expect. This can help lower your anxiety and make the journey less scary.
Hospital Admission Process
Getting ready for gastrointestinal surgery can be stressful. Knowing what happens during hospital admission can help. The admission process is key to a smooth surgery.
Pre-Registration Requirements
First, you’ll need to pre-register. Call the hospital’s admissions to share insurance and contact info. Do this early to avoid delays on surgery day. Have your insurance cards and ID ready.
Day of Surgery Arrival Procedures
Arrive at the hospital early on surgery day. You’ll check in at the admissions area. Then, you’ll go to the pre-op area. Bring your insurance card, ID, and any papers from your surgeon.
What to Expect in Pre-Op
In pre-op, nurses will get you ready for surgery. You’ll change into a gown, get an IV, and have your vital signs checked. You’ll also talk to your anesthesiologist about your anesthesia. Having a support person is helpful.
Knowing the hospital admission process can ease your stress. Being prepared helps you focus on recovery and a good surgery outcome.
Preparing Your Home for Recovery
Getting your home ready for recovery is key to a smooth healing process after surgery. A tidy home environment lowers the chance of complications. It also helps keep you comfortable and focused on getting better.
Setting Up a Recovery Space
Having a special recovery area is a must. It should be quiet, comfy, and easy to get to. If you live in a house with more than one floor, make a cozy spot on the ground floor. Or, move furniture to clear a path to the bathroom and other important spots.
Key considerations for your recovery space:
- A comfortable bed or recliner
- Easy access to water, medications, and a phone
- A clear path to the bathroom
- Minimal clutter to reduce fall risks
Stocking Essential Supplies
Having the right supplies ready before surgery can prevent last-minute trips out. Here are some things to think about:
- Prescription medications and any necessary documentation
- Comfort foods and easy-to-digest meals
- Water and electrolyte-rich beverages
- Comfortable clothing and loose-fitting garments
- Personal care items like toiletries and a thermometer
Assistive Devices You May Need
Depending on your surgery and needs, you might need special devices to help with recovery. Some common ones include:
- Grabber or reaching tool
- Shower chair or bench
- Walker or crutches
- Raised toilet seat
Talk to your healthcare provider to find out the best devices for you.
Building Your Support System
A strong support system is key for a smooth recovery after surgery. Having family, friends, and professional caregivers by your side can greatly help. They make your recovery journey easier.
Family and Friend Support Coordination
Getting help from family and friends is important. Make a list of tasks you need help with, like grocery shopping and cooking. This way, your loved ones can help out and feel involved.
It’s vital to tell your support network what you need. Let them know how they can help, whether it’s cooking meals or driving you to appointments. Just having someone to talk to can be a big help.
Professional Caregiving Options
At times, you might need professional caregivers, like if you live alone. Look for local caregiving agencies that offer the care you need. They can help with daily tasks and watch over your health.
When picking a caregiving agency, check their reputation and the qualifications of their staff. Make sure they can provide the care you need, whether it’s short-term or ongoing.
Support Groups and Resources
Joining a support group can be very helpful. These groups let you share your story, get advice, and meet others who understand what you’re going through. Look for groups focused on gastrointestinal surgery.
There are also online resources and educational materials that can help. Use these to learn more about your recovery and how to manage it well.
The Day Before Surgery Checklist
The day before your surgery is very important. You need to make sure everything is ready. This will help make your surgery go smoothly.
Final Preparations and Reminders
Review the instructions from your healthcare team on the day before. Confirm your arrival time and know what to expect. Have all your documents and information ready.
- Review and confirm your surgery schedule.
- Understand the pre-operative instructions.
- Prepare any last-minute questions for your surgeon.
Packing Your Hospital Bag
Packing your hospital bag early can help you relax. Pack comfortable clothes, personal hygiene items, and anything that makes you feel at home.
- Comfortable clothes for discharge.
- Toiletries and personal hygiene items.
- Phone and charger.
- Insurance cards and identification.
Last-Minute Documentation
Make sure you have all your documents ready. This includes insurance cards, identification, and medical records.
- Insurance cards.
- Identification.
- Medical records.
- Advance directives, if applicable.
By following this checklist, you’ll be ready for your surgery. Stay calm and ask your healthcare team if you have any questions.
Conclusion: Ensuring the Best Possible Surgical Experience
Getting ready for gastrointestinal surgery needs a detailed plan. This includes medical checks, talking to the anesthesiologist, managing medications, following diet rules, and making lifestyle changes. By following these steps, patients can have the best surgical experience.
A well-prepared patient is more likely to have a smooth and successful surgery. This means not just the day before but also the weeks leading up to it. Good preparation is key.
To prepare well for gastrointestinal surgery, it’s important to follow the recommended steps. This includes bowel prep, fasting, and making lifestyle changes. By doing this, patients can reduce risks and ensure a great surgical experience.
FAQ
What are the preop fasting guidelines before gastrointestinal surgery?
Before surgery, you need to stop eating and drinking for a while. The usual rule is to not eat or drink anything after midnight the night before. But, this can change based on the surgery and the type of anesthesia you’ll get.
What is bowel preparation for gastrointestinal surgery, and how do I prepare?
Bowel prep cleans your bowel to lower infection risks during surgery. You’ll take laxatives or cleansing solutions and follow a diet as your surgeon tells you. They’ll also give you a timeline for when to start.
What medical tests are required before gastrointestinal surgery?
You’ll need blood work, lab tests, and imaging scans to check your health. Your surgeon will tell you which tests you need based on your health and past medical history.
How do I manage my medications before gastrointestinal surgery?
You might need to stop some medicines that could affect surgery or anesthesia. But, you should keep taking medicines that are important for your health. Talk to your surgeon about your medicines.
What lifestyle modifications should I make before gastrointestinal surgery?
Quit smoking, cut down on alcohol, and adjust your exercise. These changes can improve your surgery results and lower risks of problems.
How can I prepare mentally and emotionally for gastrointestinal surgery?
To prepare mentally, manage your stress and anxiety. Use relaxation and mindfulness. Having a support system and a plan for after surgery can also help.
What should I expect during the hospital admission process for gastrointestinal surgery?
Expect to pre-register and arrive at the hospital on surgery day. You’ll do pre-op procedures. Be ready to give documents and follow hospital rules.
How do I prepare my home for recovery after gastrointestinal surgery?
Set up a recovery area, get essential supplies, and find assistive devices. This makes your recovery easier and more comfortable.
What kind of support system should I have in place after gastrointestinal surgery?
Your support system can include family, friends, caregivers, and support groups. Having a plan for after surgery helps you recover better.
What are the final preparations I should make the day before gastrointestinal surgery?
Pack your hospital bag, finish any last paperwork, and review your surgery schedule and instructions from your surgeon.
How can I optimize my nutrition before gastrointestinal surgery?
Eat a healthy diet full of nutrients. Your surgeon or a nutritionist can give you specific diet advice for your needs.
Are there any specific supplements I should consider or avoid before gastrointestinal surgery?
Some supplements might not be safe before surgery because of possible interactions with anesthesia. Talk to your surgeon about your supplements.
How can I manage my stress and anxiety before gastrointestinal surgery?
Use relaxation and mindfulness to manage stress and anxiety. Talking to your surgeon or a mental health expert can also help.
References
National Institutes of Health. Evidence-Based Medical Insight. Retrieved from
https://www.niddk.nih.gov/health-information/digestive-diseases/gastrointestinal-surgery/prepare